No.
Hospital
Birth
Age
Gender
MRI type
Epiphysiolysis surgery
Site
Resection surgery
Reconstruction method
Chemo
Follow-up (months)
MSTS
Limb length (L/R cm)
Complication
Pathology
1.
JN
2001/4/21
11
Male
2
2012/7/11
Left proximal tibia
2012/8/2
Distraction osteogenesis
Cisplatin, adriamycin and ifosfamide
30
29
82/81
None
Osteosarcoma
2.
JN
2004/9/6
7
Female
2
2012/7/30
Left distal femur
2012/8/29
Alcohol inactivated autograft replantation
Cisplatin, adriamycin and ifosfamide
17
28
82/84
Autograft fracture
Osteosarcoma
3.
JN
2008/7/12
6
Female
2
2014/8/18
Right distal femur
2014/8/27
Microwave inactivation with external fixation
Cisplatin, adriamycin and ifosfamide
5
28
74/74
None
Osteosarcoma
4.
JN
2005/8/20
9
Male
2
2014/9/1
Right proximal tibia
2014/9/24
Microwave inactivation with external fixation
Cisplatin, adriamycin and ifosfamide
6
30
77/77
None
Osteosarcoma (chondroblast)
5.
JN
2006/1/10
8
Male
1
2014/10/17
Left distal femur
2014/11/7
Microwave inactivation with external fixation
Cisplatin, adriamycin and ifosfamide
3
30
72/72
None
Osteosarcoma
6.
ZZ
1996/11/27
15
Female
3
2011/7/9
Left distal femur
2011/8/4
Allograft replantation
Methotrexate, pirarubicin, carboplatin and ifosfamide
41
23
69/69
Joint stiffness
Osteosarcoma
7.
ZZ
1994/9/1
15
Female
2
2010/4/30
Left distal femur
2010/5/13
Allograft replantation
Methotrexate, pirarubicin, carboplatin and ifosfamide
21
29
76/76
Pulmonary metastasis
Osteosarcoma
8.
ZZ
2003/4/10
9
Female
1
2012/11/22
Left distal femur
2012/11/22
Inactivated autograft replantation
Methotrexate, pirarubicin, carboplatin and ifosfamide
21
25
58/58
Autograft nonunion
Osteosarcoma
9.
ZZ
1995/4/14
15
Male
1
2010/7/21
Left distal femur
2010/7/29
Allograft replantation
Methotrexate, pirarubicin, carboplatin and ifosfamide
54
24
70/74
Infection and allograft rejection
Osteosarcoma
10.
ZZ
1995/9/15
11
Male
2
2010/1/19
Left distal femur
2010/2/6
Allograft replantation
Methotrexate, pirarubicin, carboplatin and ifosfamide
59
29
81/84
Pulmonary metastasis
Osteosarcoma
11.
TJ
2004/9/1
9
Male
3
2013/9/23
Left distal tibia plus lung mets
2013/10/21
Distraction osteogenesis
Doxorubicin and cisplatin
17
18
Unknown
Recurrence and amputation
Osteosarcoma
12.
TJ
2008/1/30
6
Female
1
2014/5/16
Left distal tibia
2014/6/17
Distraction osteogenesis
Doxorubicin and cisplatin
7
22
Unknown
Delayed union
Ewing’s sarcoma
13.
TJ
2006/1/5
8
Male
2
2014/8/14
Left distal femur
2014/9/10
Distraction osteogenesis
Doxorubicin and cisplatin
4
21
Unknown
Infection
Osteosarcoma
14.
TJ
2004/11/18
6
Male
1
2012/6/28
Right distal tibia
2012/8/20
Distraction osteogenesis
Doxorubicin and cisplatin
22
30
Equal
None
Osteosarcoma
15.
XJ
2003/8/12
8
Male
1
2012/5/25
Left proximal tibia
2012/6/21
Allograft replantation with pedicled fibula
Methotrexate, cisplatin, adriamycin and ifosfamide
26
30
Equal
Skin ulcer and local infection
Osteosarcoma
In JN from July 2012 to October 2014, five patients were treated with epiphysiolysis before tumor excision; there were three boys and two girls, with median age of 8 years (6–11 years) at surgery. Three neoplasms were located in distal femur and two in proximal tibia. On the basis of the Enneking staging system [3], in all five patients the disease was in stage IIB. All tumors were pathologically diagnosed as osteosarcoma, with four being of the osteoblastic type and one of the chondroblastic type. Preoperative chemotherapy was given in two courses on a neoadjuvant basis with cisplatin, Adriamycin and ifosfamide [4]. The reconstruction methods after tumor resection were distraction osteogenesis in one patient, alcohol inactivated autograft replantation in one patient, and microwave inactivation with external fixation in three patients.
In ZZ, between April 2010 and November 2012 [5], five patients were treated with epiphysiolysis before tumor excision; there were two boys and three girls, with median age of 13 years (9–15 years) at surgery. All five neoplasms were located in left distal femur. On the basis of the Enneking staging system, disease was at stage IIB. All tumors were pathologically diagnosed as osteosarcoma. Preoperative chemotherapy, which was given twice on a neoadjuvant basis, was with methotrexate, pirarubicin, carboplatin and ifosfamide. The reconstruction methods after tumor resection were inactivated autograft replantation in one patient, and allograft replantation with internal fixation in four patients.
In TJ from June 2012 to August 2014, four patients were treated with epiphysiolysis before tumor excision. The patients were three boys and one girl; median age at surgery was 7 years (6–9 years). One neoplasm was in the left distal femur, and three were in the proximal tibia. Three patients were in Enneking stage IIB; one boy was in stage III with pulmonary metastasis. The tumors of the three boys were pathologically diagnosed as osteosarcoma; the girl had a Ewing’s sarcoma. Preoperative chemotherapy was doxorubicin and cisplatin, which were given in three courses on a neoadjuvant basis. The method chosen for reconstruction after tumor resection was distraction osteogenesis in all four patients.
In XJ, one 8-year-old boy with a neoplasm in his left proximal tibia received epiphysiolysis before tumor excision, in May 2012. Disease was at stage IIB and pathologically diagnosed as osteosarcoma. Preoperative chemotherapy was in three courses, on a neoadjuvant basis, and with methotrexate, cisplatin, Adriamycin and ifosfamide. The method chosen for reconstruction was allograft replantation with vascularized fibula.
All patients received postoperative courses of neo-adjuvant chemotherapy. The follow-up schedule involves revisions every 3 months in the first and second year, and then every 6 months for the next 3 years. Postoperative results were evaluated according to the MSTS limb function score system. Statistical analysis involved calculation of the correlation between related factors, survival, and postoperative function.
14.1.2 Results
In JN, after a mean follow-up of 12 months (3–30 months), all children were alive and four patients were disease-free. One girl experienced fracture of an inactivated autograft and required a second operation with internal fixation. This girl, who was 7 years old at the initial surgery, was the only of the patients to suffer any limb discrepancy. The other four children showed equal lower limb length of 82, 74, 77 and 72 cm [6] (Fig. 14.1). At the most recent follow-up, no cases of recurrence or metastasis were found, and the mean MSTS score was 29 (ranging between 28 and 30).
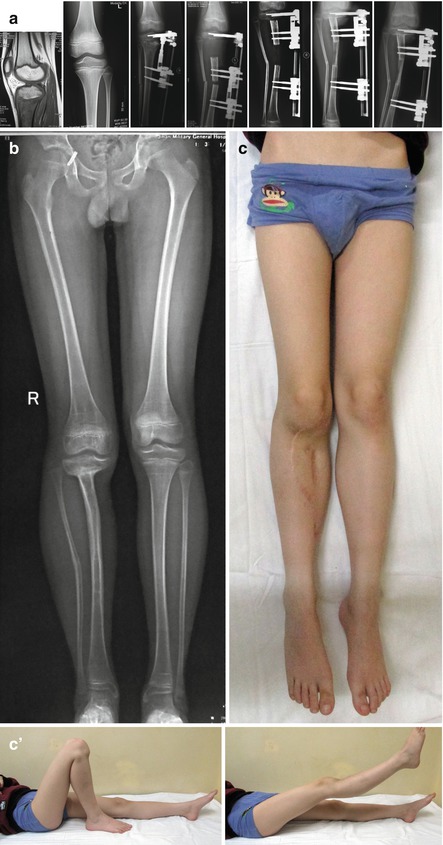
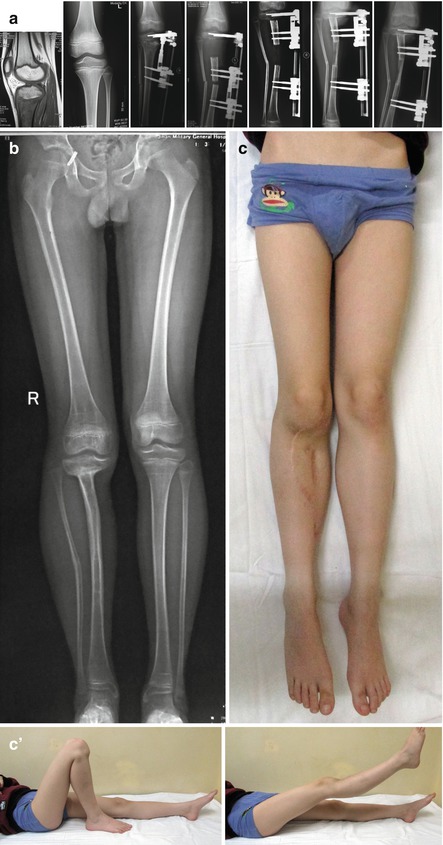
Fig. 14.1
(a) The preoperative MRI showed the tumor to be in contact with the physis. Physeal distraction was achieved, and reconstruction was made through bone transport. After 30 months, X-ray showed full bone union. (b, c) The boy showed limb equivalence with MSTS score of 30 (Endorsed by Pro.XiuChun Yu)
Of the ZZ patients, one died of pulmonary metastasis 6 months after start of treatment (epiphysiolysis). After a mean follow-up of 39 months (21–59 months), the other four children treated at ZZ were alive [5] but with certain complications: one girl had knee joint stiffness (30 months after epiphysiolysis); one boy was found to have pulmonary metastasis (31 months after epiphysiolysis (Fig. 14.2); one girl suffered non-union of an inactivated autograft, which required a second round of surgery with bone grafting (4 months after epiphysiolysis); and one boy suffered allograft infection (7 months after epiphysiolysis). The four surviving patients all have a degree of limb discrepancy: from 3 to 5 cm. At the most recent follow-up, no cases of recurrence were found, and the mean MSTS score was 26 (from 23 to 29).


Fig. 14.2
(a) Eleven year boy. The preoperative MRI showed the tumor to be nearly in contact with epiphysis, classified as Type 2. After epiphysiolysis, the patient underwent tumor resection and allograft reconstruction. Twelve months later, X-ray study showed full bone union; After 29 months, pulmonary metastasis was detected; treatment was thoracoscopic resection of pulmonary nodule. After 54 months, (b–d) the patient was alive with no metastasis; lower limb discrepancy was 4 cm. MSTS score was 29 (Endorsed by Pro.QiQing Cai)
In TJ, after a mean follow-up of 12 months (4–22 months), all four children were alive. One, a 6-year-old boy, had no recurrence, no complications, limb equivalence, and an MSTS score of 30. One boy suffered tumor recurrence above the epiphysis and underwent a second operation, with above-knee amputation. One boy had wound infection (3 months after epiphysiolysis); limb length discrepancy has not been recorded. One, the girl, had delayed union of the distal tibia and limb length discrepancy has not yet been recorded. At the most recent follow-up, the mean MSTS score was 23 (from 18 to 30).
After a follow-up of 26 months, the 8-year-old boy with OS treated at XJ was without recurrence, disease-free, and had limb equivalence. However, he experienced skin ulceration and local infection 1 year after the first operation and underwent further surgery to remove the internal fixation and perform transposition of the muscle flap. At the latest follow-up, the MSTS score was 30.
In summary, of the 15 patients, after a mean follow-up of 22 months (4–59 months), 12 (80 %) showed no evidence of disease, and eight (53 %) showed limb equivalence. Just one patient experienced local recurrence above the epiphysis. Seven patients (47 %) suffered complications, such as, skin ulceration, infection, delayed union, autograft fracture, and joint stiffness. Pooling evaluations of the most recent follow-ups, the mean MSTS score was 26.4, ranging between 18 and 30.
14.1.3 Discussion
The limb salvage procedure should not delay adjuvant therapy; reconstruction should be enduring and not be associated with a large number of local complications requiring secondary procedures and frequent hospitalization; and function of the limb should be at least as good as that obtained by amputation [7].
In most cases of osteosarcoma, especially in young patients, resection of a metaphyseal tumor with a 3–5 cm safe margin implies loss of the adjacent joint and such loss usually leads to limb length discrepancy. However, a safe margin in the context of a metaphyseal tumor can be obtained without sacrificing the epiphysis: as described by Cañadell, in tumors that do not cross the growth plate, physeal distraction provides a safe margin while averting loss of the epiphysis [2]. The growth cartilage itself is believed to provide a dependable margin of safety and so the 3–5 cm margin suggested by most authors is unnecessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


