Cancer Screening Guidelines
• Cervical dysplasia: See below
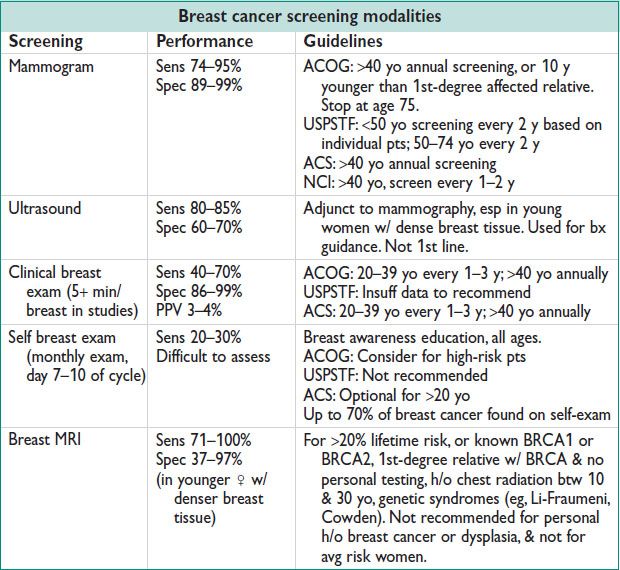
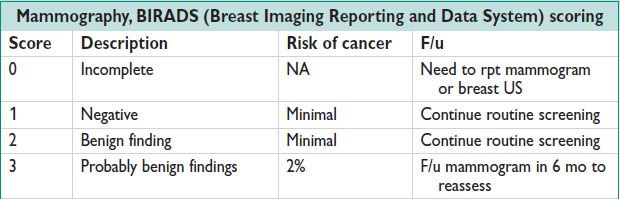
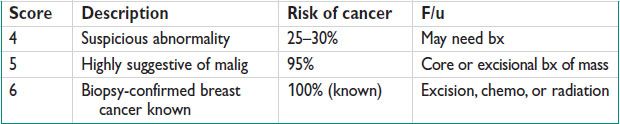
• Breast cancer: See below (Obstet Gynecol 2011;118:372)
• Colorectal cancer: Begin age 50 yo. Consider 45 yo if AA. Younger if FHx. Prefer colonoscopy q10y; other acceptable methods:
Fecal occult bld or fecal immunochemistry testing q1y w3 collected samples
Flexible sigmoidoscopy q5y
Combination of fecal occult bld & flexible sigmoidoscopy
Double contrast barium enema q5y
• Skin cancer: Counsel regarding ultraviolet exposure. Consider annual skin exam & referral for high risk. Use asymmetry/border/color/diameter/enlargement criteria.
• There are no recommended guidelines for routine screening for ovarian, endometrial, or lung cancer. H&P guide investigation.
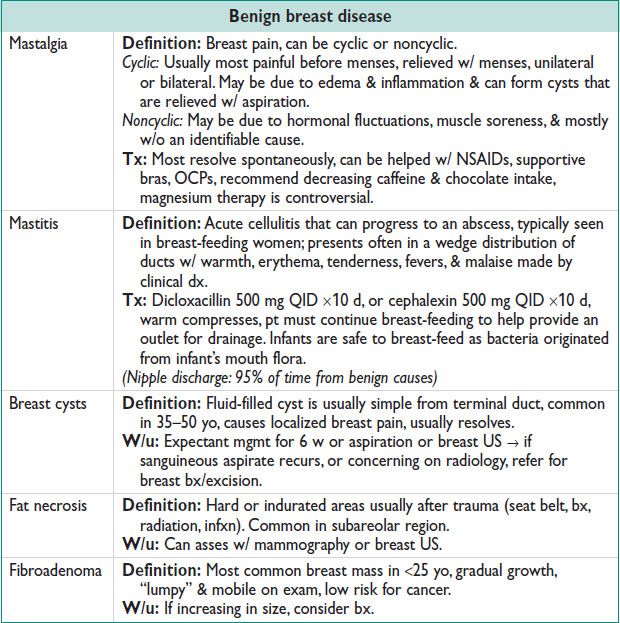
BENIGN BREAST DISEASE
Workup of a Breast Mass
• Palpable breast mass → mammogram/US → needle bx after imaging or 2 w prior (to avoid artifact) w/ FNA or core needle bx → excision if concerning or rpt exam in 6 w
Likely benign mass: Mobile, soft, smooth, <2 cm
Concerning mass: Hard, fixed, single, irreg margins, >2 cm, adenopathy, bloody nipple discharge, overlying skin changes, nonsymmetric breast appearance
• Triple test = clinical exam + imaging + breast bx → >99% NPV for concordant negative triple test. If all negative, monit q6mo by clinical exam alone. If any of these assessments sugg malig → excision.
Abnormal Radiology Findings
• Poorly defined soft tissue density, irreg borders – sometimes in a “star” appearance
• Clustered microcalcifications in 1 area
• Calcification w/i a soft tissue mass/density
• Asym w/i the breast, or skewing of breast tissue
• New abnormality not previously seen
• Worrisome findings: Soft tissue mass, clustered microcalcifications
• Most common breast mass in <25 yo, gradual growth, “lumpy” on exam, low risk for cancer → if increasing in size, consider bx
Nipple Discharge
• Very common complaint, usually benign
• Nml discharge: Common on stimulation, bilateral, serous
• Galactorrhea: Milky discharge unrelated to Preg, bilateral. Causes: Unknown, endocrine abnormalities a/w amenorrhea or hypothalamic dysfxn from endocrine abnormalities or pituitary mass, many psychiatric meds (Dopamine inhibitors).
W/u: HPI asking about visual changes, HAs, menses, thyroid sx, current meds; PE looking at visual field defects (tunnel vision).
Labs: Prolactin, TSH, free T4, CT head looking for a pituitary adenoma if elevated prolactin.
• Nonbenign discharge: Unilateral, bloody (can guaiac test if not visible), serous, or colored discharge can be a/w breast mass or overlying skin changes. Caused by carcinoma, intraductal papilloma, duct ectasia, fibrocystic changes.
W/u: Send discharge for cytology, mammogram if >35 yo or breast US if <35 yo. Cytology is of little value & has a low sens.
BREAST CANCER
Epidemiology
• Breast cancer is the most common cancer among women. 2nd most common cause of cancer death in women (after lung cancer). From 1998–2007 the incid & mortality rates have decreased. Developed nations have a higher incid than developing.
• AA women have a lower incid rate, higher mortality rate, & higher stage at dx.
Risk Factors
• Age >40 yo: 95% of breast cancers occur in women >40 yo
• FHx of breast cancer: 1st-degree relatives, premenopausal breast cancer, BRCA1 & BRCA2 mutations (tumor suppressor genes, autosomal dominant, account for 5–10% dx, but confer >80% lifetime breast cancer risk).
BRCA1/2: 50–85% risk breast cancer, 15–40% risk ovarian cancer → risk reducing mastectomy decreases risk by 90%. BRCA testing recommended for 1st-degree relative w/ breast cancer, relative w/ breast cancer <50 yo, 3+ 1st- or 2nd-degree relatives w/ breast cancer, breast/ovarian cancer in 1st- or 2nd-degree relative, 2+ 1st- or 2nd-degree relatives w/ ovarian cancer, male breast cancer (Obstet Gynecol 2008;111:231).
• Increased hormonal exposure: Early menarche (<12 yo), late menopause (>55 yo), older age w/ 1st Preg, fewer pregnancies (all these → increased lifetime estrogen exposure)
• Personal h/o breast cancer: 0.5–1% risk of developing breast cancer in contralateral breast, majority of recurrences are w/i the 1st 5 y
• Radiation exposure: 35% lifetime risk
• Diet & exercise: Physical activity & wt control are protective
Premalignant Lesions
• Atypical hyperplasia: Ductal or lobular, proliferative lesion similar to carcinoma in situ; includes intraductal papilloma, ductal epithelial hyperplasia, sclerosing adenosis → excision
• DCIS: Most common noninvasive breast cancer (1 of 5 new cases), usually dx by mammogram alone, can have breast conserving rx ± tramoxifen ± XRT
• LCIS: More common in premenopausal women, 1% risk/y of invasive cancer, sometimes found incidentally → tamoxifen vs. resection
Invasive Cancer
• Infiltrating ductal: 60–70% breast cancer; includes mucinous, tubular, & medullary carcinomas, classified by cell type, architecture of mass, & pattern of spread
• Infiltrating lobular: 10–15% breast cancer, arising in lobules, multifocal, higher incid of bilaterally
• Inflamm: 6% of breast cancer, p/w skin changes, rapid onset in a few weeks, causes diffuse induration & swelling. Dx w/ punch bx of skin & mammogram, tx w/ chemo
• Phyllodes tumor: Similar to fibroadenoma, epithelial lined spaces surrounded by monoclonal & neoplastic stromal cells. Classified as benign, intermediate, or malignant based on atypia, mitosis, abundance of stromal cells, median age of dx 40 yo, can metastasize to distant organs w/ lung as primary site; tx w/ wide local incision.
• Paget dz: Presents as focal skin changes, assoc mass identified in 60% of cases. Underlying DCIS in 2/3 of cases & invasive cancer in 1/3
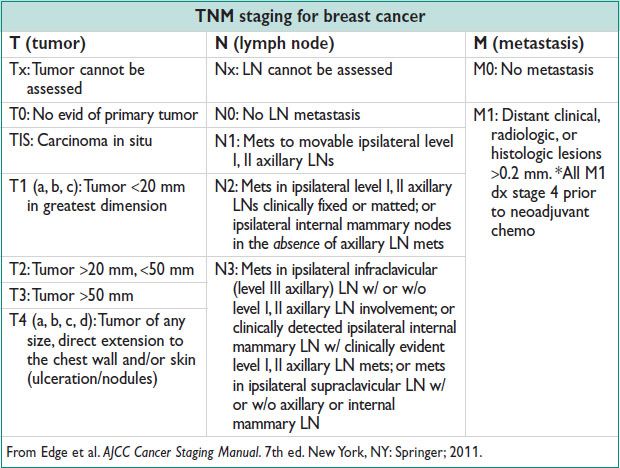
Breast Cancer Staging/Prognosis
• Tumor size & nodal metastasis strongly correlated w/ prog
• High expression of estrogen or progesterone a/w better prog
• Overexpression of HER2 (human epidermal growth factor receptor) a/w worse prog
• ER/PR status a/w improved survival rates b/c of targeted therapy of SERMs & aromatase inhibitors (reduce circulating estrogens)
Treatment
• Depends on localization of cancer may be chemo, radiation, Surg, any combination of medical & Surg. #1 lawsuit topic for gynecologist (apart from OB): Failure to diagnose or adequately/quickly refer breast cancer (Med Law 2005;24:1).
Surg: Std of care is breast conserving Surg = lumpectomy or partial mastectomy w/ 0.5–1 cm margins often w/ preop wire localization
General Ob/Gyns refer to breast specialist or general surgeon for eval & excision
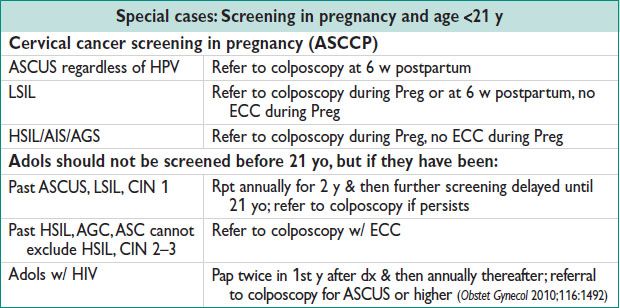
CERVICAL CANCER SCREENING
Epidemiology & Definitions (Obstet Gynecol 2012;120:1222)
• 2nd most common cancer in women worldwide. Mean age at dx: 40–59 y; bimodal distribution peaks 35–39 y & 60–64 y. Cervical cancer ↓ 50% from 1975 to 6.6/100000 women in 2008 due to pap smear screen.
Pathophysiology
• Caused by HPV infxn. An effective immune system clears HPV infxn; cervical cancer thought to be from long-term HPV infxn. >90% young healthy women clear cervical HPV w/i 1–3 y.
• HPV: E (early) & L (late) E6, E7 proteins expressed in malignant cells. E6 → degradation of tumor suppressor p53 → ↑ cell proliferation. E7 binds tumor suppressor pRb (retinoblastoma gene product) → release E2F transcription factors → ↑ replication & cell division. Unchecked cell cycle → ↑ malig.
High-risk HPV strains: 16, 18, 31, 33, 35, 45, 58 are carcinogenic
Low-risk HPV strains: 39, 51, 52, 56, 59, 68, 73, 82 (6, 11 cause genital warts)
• High-risk pts: Increased sexual contacts, new sexual partner, HIV+ or immunosuppression. These pts do not effectively clear the virus.
Pap Smear Guidelines (J Low Genit Tract Dis 2012;16:175)
• Pap smear adequate if transformation zone (junction of squamous & columnar cells w/ embryonic component) is present for cytologic eval. Sens 51%; spec 98%. HPV typing from pap smear cells can also be performed.
Start screening ≥21 yo regardless of sexual Hx. Do NOT screen ≤21 yo, except HIV+ pts. Recent ↓ in testing frequency retains benefits but minimizes harms & unnecessary procedures. Regardless of pap screening, annual Gyn exam recommended for all. If abn pap, consult current ASSCP guidelines (www.asccp.org).
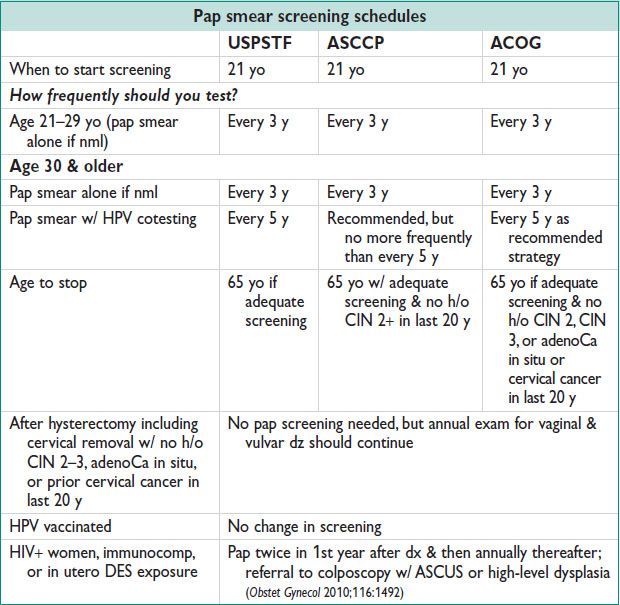
• Pap results reported as:
ASCUS: Atypical cells of undetermined significance
LSIL: Low-grade squamous intraepithelial lesion ∼ corresponds to CIN 1
HSIL: High-grade squamous intraepithelial lesion ∼ corresponds to CIN 2–3
AGC: Atypical glandular cells (means columnar cells, has association with CIN 2–3)
• Management:
ASCUS → reflex high-risk HPV testing; if HPV positive refer to colposcopy; if HPV negative rpt according to age appropriate guidelines (www.asccp.org) – OR → rpt pap in 6 mo → if rpt = ASCUS or more refer to colposcopy, if negative return to annual screening
Pts w/ negative cytology & positive HPV cotesting should either be referred directly to colposcopy or perform high-risk HPV typing. If high-risk type then referral to colposcopy should be made. If no high-risk type (16 or 18) then rpt w/ coscreening in 1 y.
LSIL/HSIL/AGC: Refer to colposcopy
Colposcopy
• Definition: Direct visualization of the cervix, vagina, & vulva w/ a mobile lighted binocular microscope to identify, map, & bx cervical lesions. Deemed adequate if transformation zone is visualized on all sides since this is the region in which abn changes occur. Visualization is aided by:
Acetic acid: Dehydrates cells → lighter appearance in dysplastic cells w/ ↑ n/c ratio/↑ chromatin = “acetowhite changes.”
Lugol iodine: Stains nml cervicovaginal epithelial cells dark due to high glycogen content, while dysplastic cells are lighter; used in place of or in addition to acetic acid.
• Abn colposcopic findings include:
Punctation: Small bld vessels visible as small dots
Mosaicism: An interspersing of white & nml epithelial cells
Acetowhite changes: A range of white-hued epithelium w/ diffuse or sharp borders
Atypical vessels: Larger vessels w/i lesions may indicate a more advanced lesion
• Any abn lesions are biopsied to evaluate for preinvasive cancer; colposcopy does not always mean bx; only abn lesions & endocervical canal are sampled.
• Endocervical curettage: Curetting the endocervical canal to obtain glandular cells or nonvisualized lesions.
• Bx results: Reported as:
CIN 1/mild dysplasia: Confined to lower 1/3 of squamous epithelium
CIN 2/mod dysplasia: Abn cells extending into the middle third of epithelial layer
CIN 3/sev dysplasia: Abn cells extending into the upper third of epithelium
CIS: Full thickness abn cells w/ no invasion of basement membrane
Cervical Dysplasia Management (Obstet Gynecol 2013;121:829)
• CIN 1 → can follow conservatively w/ surveillance; consider conization if persists >2 y
• CIN 2 → consider conization or follow w/ rpt pap/colposcopy, esp if young
• CIN 3 → conization/LEEP
• CIS → conization
• Invasive cancer → refer to Gyn oncology (see Chap. 21)
• See ASCCP for most up to date recommendations (www.asccp.org)
LIPIDS & CHOLESTEROL
Definitions and Treatment
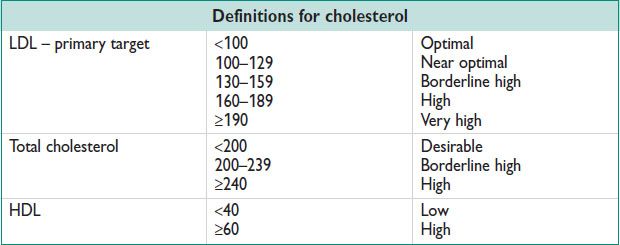
• Cardiovascular dz is the leading cause of death (all ages) in women (24%)
• Start screening total cholesterol, HDL at 20 yo, then once every 5 y
• ACOG: Start every 5 y from age 45; at well-woman visits or initial OB or w/ PCP
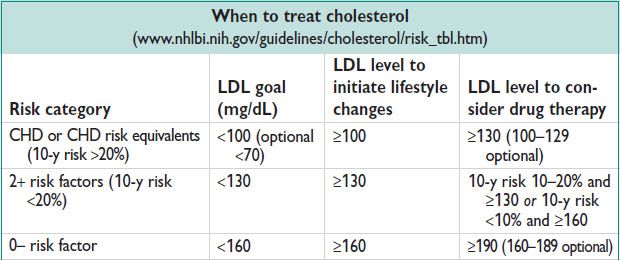
• CHD risk equivalents: Clinical coronary, symptomatic carotid dz, peripheral artery dz, abdominal aortic aneurysm, DM.
• CHD risk factors: Cigarette smoking, HTN (BP ≥140/90 or on an anti-HTN med), HDL ≤40, FHx of premature CHD (M <55 yo, F <65 yo in 1st-degree relative), age (F ≥55 yo).
• 10-y risk calculated using Framingham point risk scores w/ points for age, total cholesterol, smoking, HDL, & SBP.
• For latest guidelines see: J Am Coll Cardiol 2013 (PMID 2422016).
• Hormone effects on lipids:
Estrogen: ↓ LDL, ↑ HDL, & ↑ TG
Progestin: Antagonized estrogen changes → ↑ LDL, ↓ HDL, & ↓ TG
• ACOG recommends: LDL >160 or multi CAD risk factors, counsel toward nonhormonal contraception. 2× ↑ MI risk in  w/o CAD on hormonal therapy
w/o CAD on hormonal therapy
• Postmenopausal women on HRT (estrogen &/or progestin) → 29% ↑ in CHD events; no indication for HRT to prevent CHD. Women on HRT had a 41% ↑ in stroke events (JAMA 2002;288:321). Newer data since the WHI trial sugg younger postmenopausal women (<50 yo) on HRT do not have ↑ CHD. See Chap. 5.
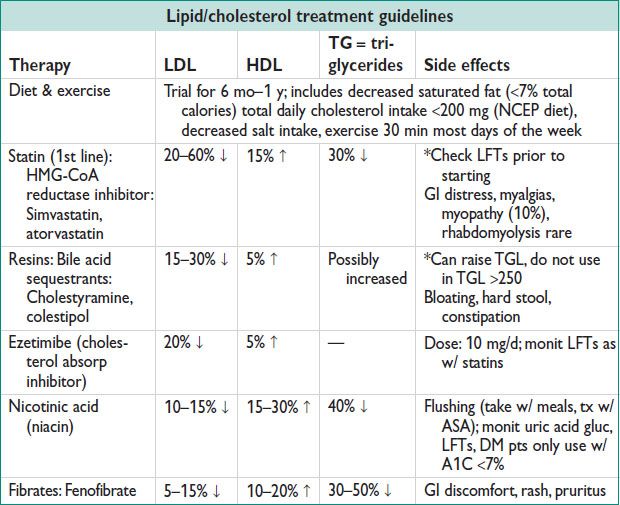
OBESITY
Definitions
Epidemiology (CDC NHANES, 2009–2010)
• 35.7% of all US adults are obese, a dramatic ↑ in the past 20 y; affects 1 in 5 pregnant women.
• 17% of all US children & adols are obese → leading to increased rate of heart dz, diabetes, & metabolic syn.
Obesity and Gynecology
• Infertility: Oligo-ovulation & anovulation, ↓ gonadotropin resp, primary rx is wt loss.
• Contraception: ↓ effectiveness of patch, combined OCPs, & implants. No difference in efficacy for Depo-Provera, few studies on other contraceptives. Metabolic changes → altered half-life or storage in adipose tissue.
• Anesthesia/surgical risk: ↑ difficulty w/ spinal/epidural anesthesia, ↑ intubation risk w/ higher Mallampati score, consider preoperative anesthesia consult, ↑ wound breakdown w/ laparotomy. ↑ DVT risk, consider prophylaxis, ambulation, SCDs, compression stockings.
• Endometrial cancer risk: Unopposed estrogen (androstenedione → estrogen by adipose tissue aromatase) → endometrial hyperplasia.
Obesity and Obstetrics (Obstet Gynecol 2013;121:213)
• Fetal anomalies: ↑ anomalies such as cleft lip/palate, neural tube, cardiac defects, ↑ macrosomia, ↑ miscarriage, 2–4× ↑ stillbirth.
• Antepartum complications: Obese  ↑ services & testing w/ Preg 2/2 difficulty measuring fundal ht, 57% of time wt gain is higher than recommended (11–20 lb for obese). ↑ large for gestational age infants. ↑ gestational diabetes, gestational HTN, preeclampsia, & fetal macrosomia.
↑ services & testing w/ Preg 2/2 difficulty measuring fundal ht, 57% of time wt gain is higher than recommended (11–20 lb for obese). ↑ large for gestational age infants. ↑ gestational diabetes, gestational HTN, preeclampsia, & fetal macrosomia.
• Labor & deliv: Difficult to follow fetal HR w/ tocodynamometer → ↑ interventions such as fetal scalp electrode placement. Protracted labor curve & ↑ labor dystocia → ↑ cesarean deliv. ↓ VBAC success rate. ↑ shoulder dystocia.
Treatment
• Nonsurgical: Nutrition & exercise programs, goal setting w/ provider, close f/u appointments, some limited pharmacotherapy; goal BMI <25.
• Surgical: Bariatric Surg for BMI >40 or >35 w/ other comorbidities w/ gastric banding, sleeve gastrectomy, or gastric bypass. Attention to contraception should be paid to women who get bariatric Surg as their fertility may ↑.
OSTEOPOROSIS
Definition (Obstet Gynecol 2012;120:718)
• Low bone mass, microarchitectural deterioration, increased bone fragility. Defined by WHO based on DEXA T-scores:
T-score: Std deviation from mean BMD of a healthy young (30 yo) adult
Nml: T-score ≥–1
Osteopenia: T-score <–1 but >–2.5
Osteoporosis: T-score <–2.5
Z-score: Std deviation from mean BMD of age-matched pop, informative in cases of sev osteoporosis
Epidemiology (AJOG 2006;194:S3)
• 8–17% US postmenopausal women have osteoporosis
• Incid increases w/ age → 48–70% affected by age 80
• By age 70, Caucasian women in US have a 40% risk of hip, spine, or forearm fracture
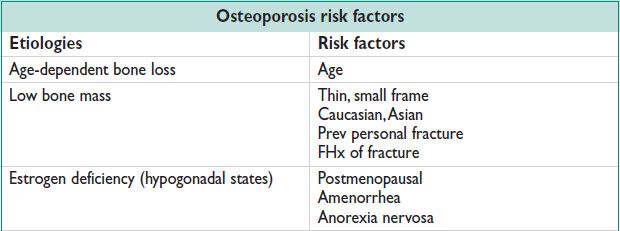
Etiology
Clinical Manifestations
• Clinically silent until fracture. Hip fracture, esp trochanteric vs. intracapsular, is the most serious complication. Vertebral fracture often p/w back pain, kyphosis, & loss of ht. Forearm fracture also possible.
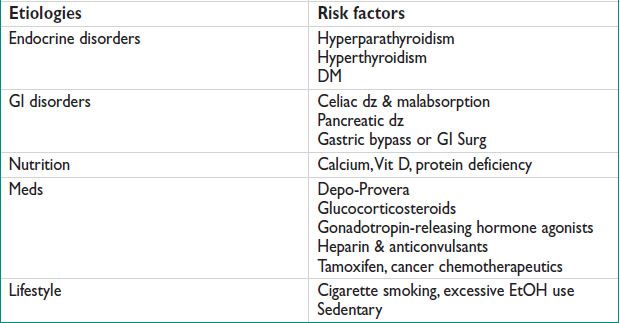
Screening
• FRAX risk assessment tool (www.shef.ac.uk/FRAX/) calculates 10-y fracture risk.
• DEXA (gold std) at 65 yo, earlier if postmenopausal w/ fracture, or risk factors (h/o fragility fracture, body wt <127 lb, medical causes of accelerated bone loss, smoker, alcoholism, rheumatoid arthritis, FHx of hip fracture in parent). FRAX 10-y risk >9.3% (65 yo risk) → early screening. Rpt screening not earlier than 2 y unless new risk factor.
• Other screening modalities (US, CT, x-ray, photon absorptiometry) are available but are less cost-effective, accurate, & available.
• Biochemical markers of bone turnover include:
Bone resorption markers: Hydroxyproline, pyridinium cross-links
Bone formation markers: Alk phos, osteocalcin, procollagen I propeptides
Fasting urinary calcium/Cr ratio indicates balance btw resorption & formation
Treatment and Medications
• Prevention and nonpharmacologic: Regular weight-bearing exercise + 800 IU Vit D daily + 1200 mg calcium daily + avoid cigarette smoking & excessive EtOH intake. Fall precautions for older or unsteady pts. ACOG calcium/Vit D recommendations:
Age 9–18: Calcium 1300 U QD, Vit D 600 U QD
Age 19–50: Calcium 1000 U QD, Vit D 600 U QD
Age 51–70: Calcium 1200 U QD, Vit D 600 U QD
Age ≥70: Calcium 1200 U QD, Vit D 800 U QD
• Pharmacologic: Initiate rx for >50 yo & vertebral/hip fracture or T-score ≤–2.5 at the femoral neck or spine or T-score –1 to –2.5 at the femoral neck or spine & 10-y fracture risk ≥3% or 10-y osteoporosis fracture risk ≥20% or low trauma fracture (esp vertebral/hip).
Bisphosphonates: 1st line, oral or IV administration (alendronate, risedronate, ibandronate, etidronate). Side effects – esophagitis, myalgias
SERM: Oral (raloxifene). Side effects – vasomotor sx, DVT, leg cramps
Calcitonin: Subcutaneous or nasal administration. Side effects – nausea, rhinitis
Parathyroid hormone: Subcutaneous administration. Side effects – HyperCa, nausea, leg cramps
Estrogen: Oral, transdermal administration. WHI demonstrated ↓ osteoporosis for both estrogen alone & estrogen–progestin therapy. Side effects – ↑ VTE, cardiovascular dz, breast cancer.
• Monitoring resp to therapy: F/u DEXA 2 y after beginning of therapy, decreased frequency thereafter if adequate resp. N-telopeptide urine measurement is useful in monitoring drug compliance or in pts w/ malabsorption, only useful if on antiresorptive meds.
SKIN CANCER SCREENING
Basal Cell Carcinoma (J Natl Compr Canc Netw 2010;8:836; BMJ 2003;327:794)
• Definition: Arises from epidermal basalis, locally invasive
• Epidemiology: Most common skin cancer. Likely 1–3 million BCC/y in US. 30% lifetime risk if Caucasian.
• Risks: Age, race, UV light exposure esp intermittent & intense, chronic arsenic exposure, ionizing radiation, immunosuppression, & PUVA therapy for psoriasis
• Pathophysiology: Sun exposure/inflammation. Genetics – PTCH1, chromo 9, tumor suppressor gene, two-hit hypothesis.
• Clinical manifestations: 70% on face, 15% on trunk
Nodular: 60% of cases, flesh-colored papule, pearly or translucent, telangiectatic vessel, may have ulceration
Superficial: 30% of cases, mostly on trunk, scaly plaque, rimmed w/ translucent micropapules
Morpheaform: Smooth, flesh-colored plaques, atrophic, ill-defined borders, aggressive
Basal cell nevus syn: Autosomal dominant inheritance, PTCH1 mutation, p/w multi BCCs at a young age, macrocephaly, bifid ribs, bone cysts, palmar pitting, & medulloblastoma.
• Tx: Less aggressive BCC (<6 mm diameter on face/hands/feet, <10 mm on head/neck, <20 mm all other areas; nodular or superficial histopathology, no perineural invasion; primary lesion, defined borders, immunocompetent, no prior radiation) → electrodessication & curettage, surgical excision. More aggressive BCC → Mohs Surg, surgical excision, XRT.
• Prog: Excellent, metastasis rate 0.55%, but 40% of pts → 2nd BCC ≤5 y
Squamous Cell Carcinoma (NEJM 2001;344:975)
• Definition: Arises from epidermal keratinocytes, locally invasive
• Epidemiology: 2nd most common skin cancer, 4–9% lifetime risk for US women
• Risks: Same as BCC, see above
• Pathophysiology: UV light, esp >30000 cumulative hours, similar to BCC. p53 mutation & other tumor suppressor genes. Prevention: Protection from sun exposure, retinoids.
Actinic keratoses: Precursor lesion, scaly erythematous macules, 1% progress to SCC, 60% of SCC arise from actinic keratoses
• Clinical manifestations: 55% on head/neck, 35% on arms/legs
SCC in situ (Bowen dz): Well-defined borders, scaly plaque, erythematous
Invasive SCC: Hyperkeratotic papules or nodules, firm, may have ulcerations
Verrucous carcinoma: Well-defined, cauliflower-like growths
Xeroderma pigmentosum: Multigenic, autosomal recessive, sev sun sens, degeneration of skin & eyes
Epidermolysis bullosa: Blister formation w/ no prev trauma, increased risk of aggressive SCC
• Tx: Staging based on TNM criteria after full-body exam → surgical excision, cryotherapy, radiation, Mohs Surg, topical 5-fluorouracil per staging
• Prog: 5-y cure rate >90%, 1% mortality rate, tumor staging correlates w/ recurrence & metastasis
Melanoma (NEJM 2006;355:51)
• Definition: Arises from epidermal melanocytes, most fatal form of skin cancer
• Epidemiology: 7th most common form of cancer in women
• Risks: Age, race, UV light exposure esp acute & intermittent, atypical nevi, high nevus count, FHx. MRAT: www.cancer.gov/melanomarisktool/
• Prevention: Insuff evid to recommend universal screening by USPSTF, but remain alert. High-risk pts → yearly screening from a dermatologist
• Clinical manifestations:
Superficial spreading melanoma: 70% of all melanomas, variably pigmented macules, irreg borders
Nodular melanoma: 15–30% of all melanomas, darkly pigmented, pedunculated nodules
Lentigo maligna melanoma: Begins as brown macule that grows to be darker, asym, & have raised areas
Acral lentiginous melanoma: <5% of all melanomas, most common form of melanoma in darker-skinned people, most commonly on palms of hands & soles of feet
ABCDE: Asymmetry, border irregularities, color variegation, diameter >5 mm, evolving lesion (Dermatology 1998;197:11). Sens 97% if single criterion met, 43% if all 5 criteria met. Spec 36% if single criterion met, 100% if all 5 criteria nml.
Glasgow criteria: Referral if 1 major criterion, presence of minor criteria reinforces need for referral
Major: Change in size or new lesion, change in shape, change in color
Minor: Diameter >6 mm, inflammation, crusting or bleeding, sensory change
Ugly duckling sign: Used to observe a pt w/ multi nevi, refer if a pigmented lesion appears different than the surrounding lesions
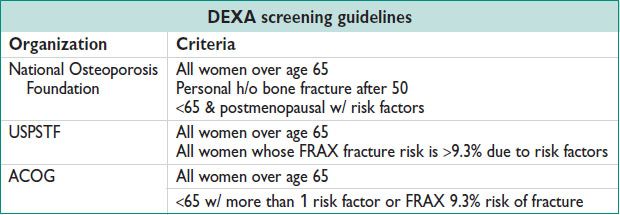
• Tx: Staging based on tumor thickness, mitotic rate, & ulceration → wide local excision, LN excision, & adjuvant immunotherapy
• Prog: Based on tumor thickness (J Clin Oncol 2009;27;6199)
DOMESTIC VIOLENCE
Definitions
• Intentional controlling or violent behavior by someone in a relationship w/ the victim. Includes physical, sexual, verbal, & emotional abuse as well as economic depriv.
• IPV: Victim is often intimately involved w/ her abuser.
• Common couple violence: Not connected to general control behavior, arises in a single argument where one/both partners are injured.
• Intimate terrorism: General pattern of abuser control, emotional & psychological abuse, not mutual, more likely to escalate over time, more likely to involve serious injury.
• Violent resistance: Self-defense, violence by victim against abuser.
• Phases of abuse: Tension-building: Poor communication, fear, victim tries to pacify the abuser. Acting-out: Outburst of violent, abusive behavior. Honeymoon: End of violence → affection & apology.
Epidemiology
• Affects over 1 million  each year. 54% of
each year. 54% of  report an abusive relationship in the past.
report an abusive relationship in the past.
• Higher prevalence if under age 35, single, divorced/separated, abuse EtOH or drugs, smoke, pregnant, lower socioeconomic class, h/o childhood abuse.
• Elder abuse: 10% of women over 65 report physical, sexual, or verbal abuse or neglect. Risks: Advanced age, AA, disability in self-care, dementia, depression, h/o hip fracture, h/o stroke, social isolation, low socioeconomic status, institutional staffing shortages.
• Preg: Domestic violence affects 7–20% of pregnancies, 3-fold higher risk if Preg is unintended, Preg can result from reproductive coercion (forced Preg by contraception sabotage). Victims more likely to deliver preterm & by cesarean section. 3-fold ↑ risk of attempted/completed homicide. Highest risk of IPV in 3rd trimester & postpartum.
• No typical abuser or victim, IPV affects all ages, races, & socioeconomic classes.
Clinical Manifestations
• Inconsistent explan of injuries or delay in seeking rx. Somatic complaints (HAs, abdominal/pelvic pain, fatigue). Depression, anxiety, eating disorders.
• Presenting late to prenatal care. Frequent ED visits. Noncompliance w/ rx. Skin tears, bruises, bone fractures, malnutrition, dehyd, & pressure ulcers common in victims of elder abuse.
• Most injuries on breasts, abd, & genitals, esp in Preg. Defensive wounds on hands, arms. Bruises of different ages.
Diagnostic Workup/Studies
• Screen routinely in all pregnant pts, for well-woman/preventive visits. No strong evid that routine screening decreases harm (USPSTF).
• SAFE questions (JAMA 1993;269:2367)
“Do you feel safe in your relationship?”
“Have you ever been in a relationship where you have been threatened, hurt, or afraid?”
“Are your family/friends aware that you have been hurt? Could you tell them and would they be able to give you support?”
“Do you have a safe place to go and resources you need in an emergency?”
• Abuse assessment screen: Identifies physical or sexual abuse in Preg (JAMA 1992;267:3176)
“Within the last year, have you been hit, slapped, kicked, or otherwise physically hurt by someone?”
“Since you’ve been pregnant, have you been hit, slapped, kicked, or otherwise physically hurt by someone?”
“Within the last year, has anyone forced you to have sexual activities?”
• BASE & the CTS can be used to screen for elder abuse (JAGS 2004;52:297)
Treatment and Medications
• RADAR: Routinely screen, Ask direct questions, Document your findings, Assess safety, Review options. Provide supportive counseling & validation of a pt’s fear.
• Assess risk for escalation: Presence of weapons in the home, increasing violence frequency/severity, partner’s knowledge that victim is planning to leave, threats of homicide.
• Refer to social workers, safe houses, ER. 1–800–799-SAFE provides information regarding local resources in every state.
• Specific, detailed, accurate, & nonjudgmental documentation is essential in case the victim seeks legal redress. Mandatory reporting of child abuse in all states. Many states require elder abuse reporting. Some states require IPV reporting for adult women as well.
SUBSTANCE ABUSE
Definitions
• Use: Sporadic consump, no adverse effects
• Abuse: Maladaptive pattern or inappropriate use of a substance, adverse effects from use
• Dependence: Individual persists in substance use despite problems
Physical: Characterized by withdrawal sx if abrupt cessation of substance or antag administered
Psychological: Need for substance either for positive effects of use or to avoid negative effects of abstinence
• Addiction: Behaviors that include impaired control, compulsive use, use despite harm, & craving
Epidemiology
• Affects 10% of the general pop. 48% of 12th graders have reported using an illicit substance at some point. 140 million people worldwide are EtOH dependent.
• 30% of suicides relate to EtOH abuse. Accounts for up to 40% of hospital admissions.
Clinical Manifestations
• Repetitive use → drug tolerance → withdrawal sx when drug is stopped, including depression, anxiety, malnutrition, wt loss, suicidality, agitation, & sleep disturbances.
• EtOH: P/w tolerance, blackouts or memory lapses, sleep disturbances, tremors. Intoxication = slurred speech, incoordination, unsteady gait, nystagmus, memory impairment, stupor, or coma.
• Delirium tremens: Withdrawal syn of sev EtOH abuse, hallucinations, disorientation, tachycardia, HTN, fever, agitation, diaphoresis.
• Cocaine: Acute intoxication = increased energy/alertness/sociability, euphoria, decreased fatigue/need for sleep/appetite, pupillary dilation. Chronic use = cognitive impairment, risk–reward decision making, suicidality. Withdrawal = depression, anxiety, fatigue, difficulty concentrating, anhedonia, increased appetite, increased sleep.
• Opioids: Acute intoxication = sedation, euphoria, respiratory depression, pupillary constriction, constipation, slurred speech. Withdrawal = anxiety, irritability, drug cravings, tachypnea, rhinitis, muscle aches, nausea/vomiting, diarrhea, sweating, tremors.
• On physical exam note papillary size (dilation/constriction), behavior, tachycardia, speech patterns, skin inspection for injection marks, hepatomegaly, signs of HIV/AIDS, nasal mucosal atrophy/nasal septum perforation, signs of STI.
Diagnostic Workup/Studies
• Screening tools:
CAGE-AID: Adapted for EtOH & drug abuse (Wis Med J 1995;94:135):
“Have you ever tried to cut down on your alcohol or drug use?”
“Do you get annoyed when people comment on your alcohol or drug use?”
“Do you feel guilty about things that you have done while drinking or using drugs?”
“Do you need an eye-opener to get started in the morning?”
T-ACE: Specifically for EtOH abuse in Preg:
“How many drinks does it take you to feel high?” (T = tolerance)
“Do you feel annoyed by people complaining about your drinking?”
“Have you ever felt the need to cut down on your drinking?”
“Have you ever had a drink first thing in the morning?” (E = eye-opener)
Single-item screening test: 100% sens, 73% spec
“How many times in the past year have you used an illegal drug or used a prescription med for nonmedical reasons?”
• Labs: Urine or serum toxicology screening
Treatment and Medications
• Stages of change (Am Psychol 1992;47:1102):
Precontemplation: Lack of awareness of problem, no intention to change behavior.
Contemplation: Aware of problem, weighing pros & cons to solve problem, no commitment to change action but considering changing behavior in next 6 mo.
Preparation: Intend to take action in the next month, some reductions in problem behavior.
Action: Modification of behavior/experiences/environment to overcome problem.
Maintenance: Extends from 6 mo onward, working to prevent relapse & consolidate gains achieved in the action phase.
• FRAMES: Physician motivational interviewing to help trigger pt change. Giving feedback based upon a thorough assessment. Helping the pt take responsibility for changing. Giving clear advice on what behavior must change. Offering a menu of options for making the change. Expressing empathy for the ambivalence & difficulty in making changes. Evoking self-efficacy to foster commitment & confidence.
• Nonpharmacologic: Cognitive behavior therapy, family therapy, exposure therapy.
• Pharmacologic:
Methadone: Synthetic opioid, long half-life, used to treat opioid dependence.
Buprenorphine: Semisynthetic opioid, used to treat opioid dependence.
Naltrexone: Opioid receptor antag, used to treat opioid & EtOH dependence.
Disulfiram: Causes acute sens to EtOH leading to adverse affects if EtOH used (ie, nausea & vomiting), used to treat EtOH dependence.
Bupropion: Antidepressant & smoking cessation aid.
Varenicline: Aid in smoking cessation, more effective w/ physician support.
• Prog: Remission in 35–60% of pts varies based on duration, social support, comorbid conditions, level of functioning at initiation of rx, premorbid functioning.
DEPRESSION AND PSYCHIATRIC DISEASE SCREENING
Definitions
• Major depression criteria: Depressed mood or anhedonia + 5 or more of the following sx present most of the day for nearly every day of 2 consecutive weeks: Depressed mood, anhedonia, insomnia/hypersomnia, change in appetite/wt, psychomotor retardation/agitation, low energy, poor conc, thoughts of worthlessness or guilt, recurrent thoughts of death or suicide. Remember, SIGE CAPS: Sleep, Interest, Guilt, Energy, Concentration, Appetite, Psychomotor, Suicide.
• Bipolar d/o: Includes both manic episodes (distinct periods of abnormally & persistently elevated, expansive, or irritable mood, lasting at least 1 w) & depressive episodes.
• Dysthymia: Depressed mood for at least 2 y w/ less numerous sx than major depression. May have symptom-free periods of <2 mo during this time.
• Adjustment d/o: Depressed mood or functional impairment in resp to an identifiable stressor w/i 3 mo of onset of the stressor & resolved w/i 6 mo.
Epidemiology
• 17% lifetime prevalence for major depression, 3% for dysthymia in US. 40% recurrence rate in 2 y. 25–50% of people w/ bipolar dz attempt suicide.
• Women almost twice as likely as men to be affected.
• Risks: Internalizing factors (genetics, neuroticism, low self-esteem, early-onset anxiety d/o, past h/o major depression), externalizing factors (genetics, substance misuse, conduct d/o), adversity (trauma, stressful life events, parental loss, low parental warmth, divorce, marital problems, low social support, low education).
Diagnostic Workup/Studies (Psychiatry Res 2011;187:130)
• Screening (2-item tool): “During the last month, have you felt down, depressed, or hopeless?” & “During the last month, have you felt little interest or pleasure in doing things?” PHQ-9: Assesses 9 sx of DMS-IV-TR definition of depression.
• EPDS: Validated for postpartum depression
Treatment and Medications
• Screen for bipolar dz & manic sx prior to initiating therapy for depression.
• Psychotherapy: Similar efficacy to pharmacotherapy. Includes cognitive therapy, behavioral therapy, & interpersonal therapy.
• Pharmacotherapy: 50–60% response w/ med (SSRIs, SNRIs, TCAs, MAOIs).
SSRIs are 1st-line therapy. Start low dose & ↑ as necessary to minimize side effects. Evaluate pts every 1–2 w in the 1st 8 w of therapy. If no resp in 8 w switch to another antidepressant.
• Refer if sev depression endangering the life of the pt or others. Failed to respond to initial rxs. Psychotic depression. Depression that is part of bipolar or schizoaffective d/o.
CONTRACEPTION AND STERILIZATION
Epidemiology (Contraception 2011;83:397)
• ∼50% of pregnancies in US are unintended.
• PRAMS: 33% of  w/ unintended Preg did not think they could get pregnant at the time of conception; 22% stated their partner did not want to use contraception; 16% cited side effects; 10% cited access.
w/ unintended Preg did not think they could get pregnant at the time of conception; 22% stated their partner did not want to use contraception; 16% cited side effects; 10% cited access.
• Contraceptive efficacy should be compared to 85% unprotected Preg rate in 1 y. Assessed by perfect (failure rate if used exactly according to guidelines) & typical use (failure rate for the usual compliance).
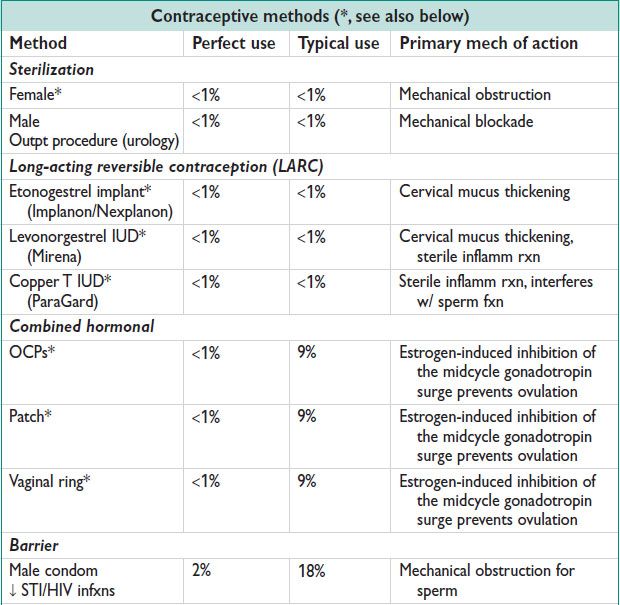
*Special Considerations
• WHO or CDC criteria for contraceptive considerations w/ medical problems, see www.cdc.gov/reproductivehealth/unintendedpregnancy/usmec.htm
• Female sterilization (Am J Obstet Gynecol 1996;174:1161):
Postpartum salpingectomy: Most effective method of female sterilization; after deliv.
Interval sterilization: Sterilization at other than postpartum period.
Unipolar coagulation is the most effective method of laparoscopic female sterilization.
Hysteroscopic sterilization (Essure) was not available for the CREST study, but is highly effective, outpt. Minimally invasive method w/o limitations by BMI, adhesive dz. Requires confirmation of tubal occlusion w/ hysterosalpingogram at 3 mo.
• Combined hormonal methods (= estrogen + progestin):
Side effects – breakthrough bleeding, breast tenderness, HA, nausea/vomiting.
OCPs: Both estrogen & progesterone or progesterone-only pills. Can interact w/ other meds (Abx, antiretrovirals, antiepileptics) → potential ↓ efficacy of either or both meds. Useful for menorrhagia, dysmenorrhea, hirsutism, & acne. ↓ risk of endometrial & ovarian cancer. Monophasic vs. multiphasic preparations are available. Monthly vs. continuous dosing is feasible, continuous dosing may be preferable for cyst formation prevention, endometriosis, PMS/PMDD, lifestyle reasons.
Contraceptive patch: Replaced weekly × 3 w then removed for 1 w (menses). ↑ thromboembolic events compared to combined OCPs.
Vaginal ring: Placed intravaginally × 3 w then removed for 1 w (menses). Small ↑ in vaginitis, vaginal discharge, & leukorrhea compared to OCPs.
• Progestin-only methods:
Mech of action: Thickened cervical mucus, thinned endometrium, ovulation inhib
Side effects: Breakthrough bleeding, acne, follicular cysts, wt gain, mood changes
POP: Preg rate <1% perfect use, 9% typical use. Must be taken every day. Shorter half-life, therefore missed doses more signif.
DMPA: Preg rate <1% perfect use, 6% typical use. One intramuscular or subcutaneous injection every 90 d (12 w). Side effects: Wt gain 3–6 kg/y, esp in obese adols, ↓ BMD, but reversible after discontinuation (DEXA scan not recommended).
Etonogestrel implant (Implanon/Nexplanon): Placed in upper arm, in-office, effective for 3 y. Side effects: Breakthrough bleeding common → major reason for early discontinuation, no ↓ BMD like DMPA, risks of insertion include pain, bleeding, infxn, expulsion, & difficult removal.
Levonorgestrel IUD (Mirena): Inserted in-office, lasts for 5 y. Effective for menorrhagia, dysmenorrhea, endometriosis, endometrial hyperplasia, & possibly Grade 1 Stage I endometrial cancer. Adolescence, nulliparity, prev STI, & prev ectopic Preg are not contraindications to IUD placement. ↑ ectopic Preg w/ IUD, but overall rate of ectopic ↓ due to decreased Preg.
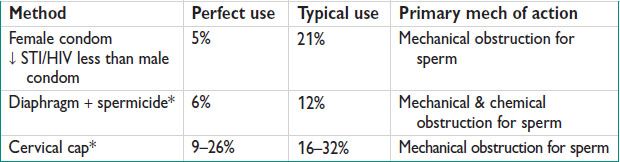
• Nonhormonal methods
Copper IUD: Inserted in-office. Effective for 10 y. Does not impact menstrual regularity, but may cause slightly heavier menses. Adolescence, nulliparity, prev STI, & prev ectopic Preg are not contraindications to IUD placement.
Diaphragm with spermicide: Requires annual fitting, not common in US. Refit if recent Preg or change in wt. Increases risk of urinary tract infxn. Insert 6 h prior to intercourse, remove 6–24 h after intercourse.
Cervical cap: Requires annual fitting, not common in US. Insert 20 min to 4 h prior to intercourse, remove 24–36 h after intercourse.
Withdrawal: Preg rate: 4% perfect use, 22% typical use. Used by up to 56% of women using contraception, usually secondary in conjunction w/ condoms.
Lactational amenorrhea: Preg rate: 2% perfect use, 5% typical use. Effective for 1st 6 mo postpartum only if exclusive breast-feeding (only nutrition for infant), breast-feeding every 4 h during the day & at least every 6 h at night, no menses if ≥56 d postpartum.
Rhythm method: Preg rate: 0.4–5% perfect use, 12–23% typical use. Relies on regular menstrual cycles & the limited viability of ova/sperm w/o fertilization. Can use menstrual calendars, cervical mucus changes, basal body temperature, or ovulation kits to avoid intercourse during midcycle fertile days.
EMERGENCY CONTRACEPTION (EC)
Definition (Obstet Gynecol 2010;115:1100)
• Use of drugs or a device (IUD) as an emergency measure to prevent Preg.
• Intended for occasional or back-up use, not as a primary contraceptive method.
• Indications: No contraception used during sexual intercourse w/i the prev 120 h. Contraceptive failure or incorrect use of a contraceptive w/i the prev 120 h including condom breakage, 2 missed combined OCPs, POP taken more than 3 h late, 2 w late for DMPA injection, dislodgement of cervical cap/diaphragm/skin patch/vaginal ring, expulsion of IUD.
• Access: Physicians should be aware of national & state laws regarding the availability of & prescribing emergency contraception. Available w/o a prescription to people of age 17 or older.
Mechanism of Action
• May include 1 or more of the following: Inhibition or delay of ovulation. Interference w/ tubal transport or fertilization. Prevention of implantation. Regression of corpus luteum.
• EC does not interrupt Preg & is ineffective after Preg has been established.
• Efficacy: 75% Preg rate reduction w/ the use of oral EC (if 1000 women had intercourse in the middle 2 w of their cycle, 80 would normally become pregnant but w/ use of oral EC the rate is reduced to 20). Efficacy influenced by: Time from unprotected intercourse to administration. Pt’s BMI: 2–4× higher risk of Preg if overweight or obese for oral EC. Timing of unprotected intercourse to day of cycle. Further intercourse after use of EC (4× higher risk vs. those that did not report further intercourse).
Treatment and Medications (Cochrane 2008;2:3)
• Physical exam & lab tests not req prior to EC. Exclude Preg esp before IUD.
• Levonorgestrel (Plan B): 1.5 mg PO in a single dose. Effective up to 120 h from unprotected intercourse, though most effective w/i 1st 72 h. 98% of pts menstruate w/i 21 d (mean 7–9 d). Administer Preg test if no menses w/i 28 d.
Side effects – irreg bleeding, nausea/vomiting (give antiemetics). Redose if vomiting w/i 2 h of administration.
• Ulipristal (Ella): 30 mg PO in a single dose. Selective progesterone receptor modulator. Effective up to 120 h from unprotected intercourse. Likely more effective than levonorgestrel from 72–120 h after unprotected intercourse.
• Copper IUD (ParaGard): Must be inserted w/i 120 h from unprotected intercourse.
More effective in overweight/obese women than levonorgestrel. Provides long-term, effective contraception along w/ EC.
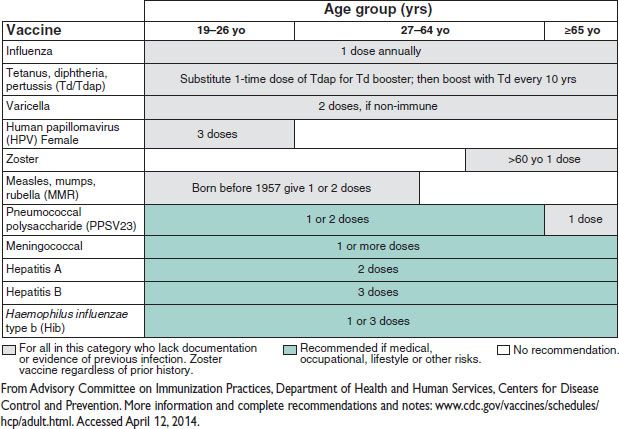
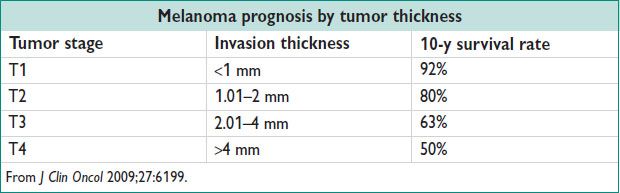
VACCINATIONS
Figure 1.1 Recommended United States Adult Immunization Schedule 2014