 |
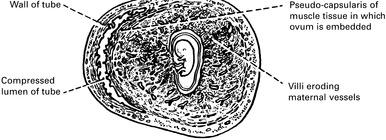
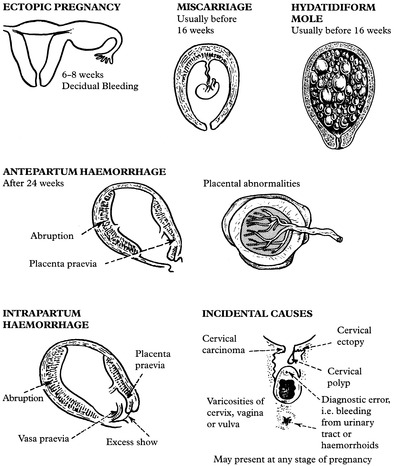
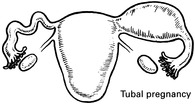
ECTOPIC PREGNANCY
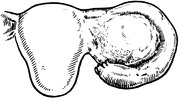
The fallopian tube is about 10 cm long. The diameter of the lumen varies from 1 mm in the interstitial portion to about 5 mm at the fimbriated end.
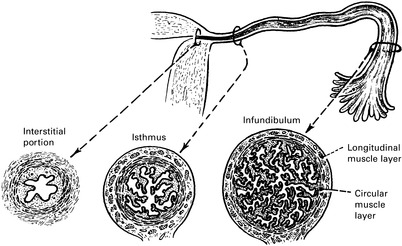 |
The musculature is of two layers, an inner circular and an outer longitudinal, and peristaltic movements are particularly strong during and after ovulation. The mucosa is arranged in plications or folds which become much more complete and plentiful as the infundibulum is approached.
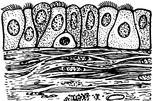
The mucosa consists of a single layer of ciliated and secretory cells, resting on a thin basement membrane. There is little or no submucosa and no decidual reaction, so muscle is easily invaded by trophoblast.
 |
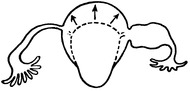
TUBAL PREGNANCY — IMPLANTATION
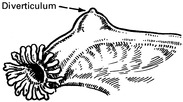
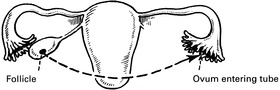
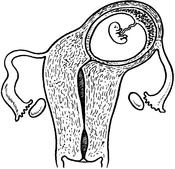
The ampulla is the commonest site of implantation, followed by the isthmus.
 |
Interstitial implantation is rare but very dangerous because it ends in rupture of the uterine muscle with severe haemorrhage.
 |
TUBAL PREGNANCY — OUTCOME
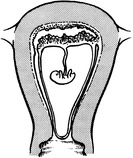
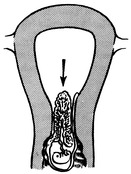
RUPTURE INTO LUMEN OF TUBE (TUBAL ABORTION)
This is usual in ampullary pregnancy at about 8 weeks. The conceptus is extruded, complete or incomplete, towards the fimbriated end of the tube, probably by the pressure of accumulated blood.
 |
There is a trickle of bleeding into the peritoneal cavity, and this may collect as a clot in the pouch of Douglas. It is then called a pelvic haematocele.
 |
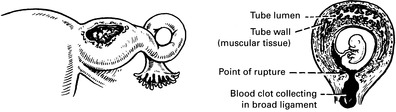
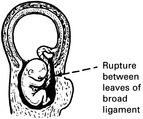
RUPTURE INTO THE PERITONEAL CAVITY
Sometimes rupture is extraperitoneal between the leaves of the broad ligament — broad ligament haematoma. Haemorrhage in this site is more likely to be controlled.
 |
TUBAL PREGNANCY — EFFECT ON UTERUS
The uterus enlarges in the first three months almost as if the implantation were normal and may reach the size of a gravid uterus of the same maturity. This is a source of confusion in diagnosis.
 |
The uterine decidua grows abundantly and when the embryo dies bleeding occurs as the decidua degenerates. Rarely it is expelled entire as a decidual cast.
 |
TUBAL PREGNANCY — SYMPTOMS AND SIGNS
PAIN in the lower abdomen is always present and may be either constant or cramp-like.
It may be referred to the shoulder if blood tracks to the diaphragm and stimulates the phrenic nerve, and it may be so severe as to cause fainting. The pain is caused by distension of the gravid tube, by its efforts to contract and expel the ovum, and by irritation of the peritoneum by leakage of blood.
VAGINAL BLEEDING occurs usually after the death of the ovum and is an effect of oestrogen withdrawal. It is dark brown and scanty and its irregularity may lead the patient to confuse it with the menstrual flow and thus, inadvertently, give a misleading history. In about 25% of cases tubal pregnancy presents without any vaginal bleeding.
INTERNAL BLOOD LOSS can be severe and rapid and the usual signs of collapse and shock will appear.
Acute internal bleeding is the most dramatic and dangerous consequence of tubal pregnancy, but it is less common than the condition presenting by a slow trickle of blood into the pelvic cavity.
PELVIC EXAMINATION in the conscious patient will demonstrate extreme tenderness over the gravid tube or in the pouch of Douglas if a haematocele has collected. If the pregnancy is sufficiently advanced and rupture has not occurred, a cystic (and very tender) mass may be felt in the fornix; but often tenderness is the only sign elicited.
PERITONEAL IRRITATION may produce muscle guarding, frequency of micturition, and later a degree of fever, all leading towards a misdiagnosis of appendicitis.
SIGNS and SYMPTOMS of EARLY PREGNANCY may be present and help to distinguish the condition from other causes of lower abdominal pain. The menstrual history may be confusing, as noted above, and when implantation occurs in the isthmus, tubal rupture may occur before the patient has missed a period.
ABDOMINAL EXAMINATION will demonstrate tenderness in one or other fossa. If there has been much intraperitoneal bleeding there will be general tenderness and resistance to palpation over the whole abdomen.
TUBAL PREGNANCY — DIFFERENTIAL DIAGNOSIS
1. Salpingitis.
2. Miscarriage.
3. Appendicitis.
4. Torsion of pedicle of ovarian cyst.
5. Rupture of corpus luteum or follicular cyst.
6. Perforation of peptic ulcer.
1. SALPINGITIS
Swelling and pain are bilateral, fever is higher and a pregnancy test is usually negative.
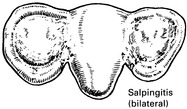 |
There may be a purulent discharge from the cervix.
2. MISCARRIAGE (threatened or incomplete)
Bleeding is the dominant clinical feature and usually precedes pain. The bleeding is red rather than brown and the pain is crampy or colicky. The uterus is larger and softer and the cervix patulous or dilated. Products of conception may be recognised on vaginal examination.
3. APPENDICITIS
The area of tenderness is higher and may be localised in the right iliac fossa. There may be a swelling if an appendix abscess was formed but is not so deep in the pelvis as a tubal swelling. Fever is greater and the patient may appear toxic. A pregnancy test will usually be negative although pregnancy and appendicitis can, of course, coexist.
 |
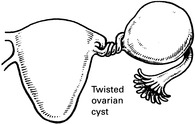
4. TORSION OF PEDICLE OF OVARIAN CYST
The mass so formed can usually be felt separate from the uterus, while a tubal pregnancy usually feels attached. Tenderness may be marked, and intraperitoneal bleeding may produce fever. Signs and symptoms of pregnancy are absent but there is a history of repeated sudden attacks of pain which pass off.
 |
5. RUPTURE OF CORPUS LUTEUM
It is virtually impossible to distinguish this, by examination, from a tubal pregnancy, but such a severe reaction is rare.
TUBAL PREGNANCY — AIDS TO DIAGNOSIS
2. Always think of tubal pregnancy; a woman with lower abdominal pain in whom there is a possibility of pregnancy should be regarded as having an ectopic until proved otherwise.
3. Pregnancy test. Highly sensitive modern pregnancy tests have made the early diagnosis of ectopic pregnancy much easier. A positive test will nearly always be found by the time of clinical presentation.
4. Ultrasound. The main value of ultrasound is to exclude an intra-uterine pregnancy. If this is done in the presence of a positive pregnancy test, ectopic pregnancy is likely. Increasingly, however, high-resolution ultrasound machines and transvaginal scanning may actually demonstrate the pregnancy outwith the uterus.
5. Laparoscopy. This remains the main means of diagnosis in suspected ectopic pregnancy although the increased use of transvaginal ultrasound and better pregnancy testing may make it unnecessary. The laparoscope is particularly useful for identifying an unruptured tubal pregnancy which is producing equivocal symptoms, and for excluding salpingitis and bleeding from small ovarian cysts. Laparoscopy may also enable operative treatment using minimally invasive methods.
 |
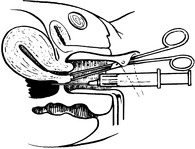
6. Culdocentesis. This means passing a needle through the posterior fornix into the pouch of Douglas. This may be helpful if laparoscopy is not available. Intraperitoneal blood does not readily clot and if such blood is obtained it is an indication for laparotomy.
 |
TUBAL PREGNANCY — TREATMENT
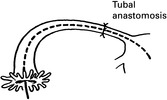
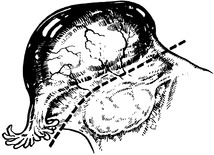
2. Laparotomy will usually be required where there is extensive intra-peritoneal bleeding. Blood and clot should be removed and a severely damaged tube excised (salpingectomy). This may, however, be effected by means of a laparoscope without recourse to open surgery.
 |
The earlier diagnosis of tubal pregnancy has allowed a more conservative approach to management, permitting greater prospects of less intervention such as laparoscopic salpingectomy or greater chance of future intra-uterine pregnancy by using methotrexate, a chemotherapeutic agent which destroys the abnormally sited trophoblast. This is usually given intramuscularly and its use results in resorption of the conceptus. If methotrexate is used then careful follow-up, to identify declining levels of HCG, is essential to determine that treatment has been effective and that surgical removal of the ectopic pregnancy is not indicated.
ABDOMINAL PREGNANCY
Clinical Features
1. There is a history of ‘threatened miscarriage’ with irregular bleeding.
2. Continued abdominal discomfort is felt and fetal movements are painful.
3. Fetal abnormality is common and fetal mortality is high.
 |
Diagnosis is difficult.
1. Palpation is unreliable even when fetal limbs are easily felt.
2. Ultrasound may show the fetus outwith the uterus and an abnormal fetal attitude due to lack of liquor.
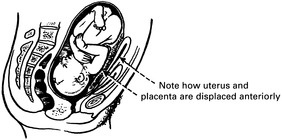 |
Treatment
Once diagnosed or strongly suspected, it is better to perform laparotomy in the interests of the mother. The fetus is removed, the cord tied and the abdomen closed. No attempt is made to detach the placenta unless it is clear that bleeding can be controlled.
If the condition is diagnosed around the time of fetal viability then delivery may be deferred to improve the prognosis for the fetus. This approach requires careful supervision and laparotomy may be required at any time.
MISCARRIAGE
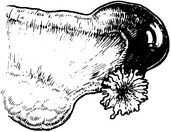
Up to 12 weeks, before the placenta is independently developed, miscarriage may be complete as shown, but from the 12th to 24th week the gestation sac is likely to rupture, leading to expulsion of the fetus, while the placenta is retained.
COMPLETE
Uterine contractions are felt, the cervix dilates and blood loss continues. The fetus and placenta are expelled complete, the uterus contracts and bleeding stops. No further treatment is needed.
or
INCOMPLETE
In spite of uterine contractions and cervical dilatation, only the fetus and some membranes are expelled. The placenta remains partly attached and bleeding continues. This miscarriage must be completed by surgical methods.
 |
Classification is based on a mixture of clinical and pathological concepts, and is sufficiently flexible to suit a condition in which diagnosis is often only presumptive. Sepsis can complicate any type of abortion and, in countries with restrictive laws on abortion, must often be due to criminal interference.
 |
MISCARRIAGE — AETIOLOGY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree