Fig. 3.1
Different types of uterine malformations. (a) Uterus septus cervix duplex vagina septa. (b) Uterus septus cervix septa. (c) Uterus communicans septus cervix septa vagina septa. (d) Uterus bicornis duplex vagina septa. (e) Uterus didelphys cervix duplex vagina septa
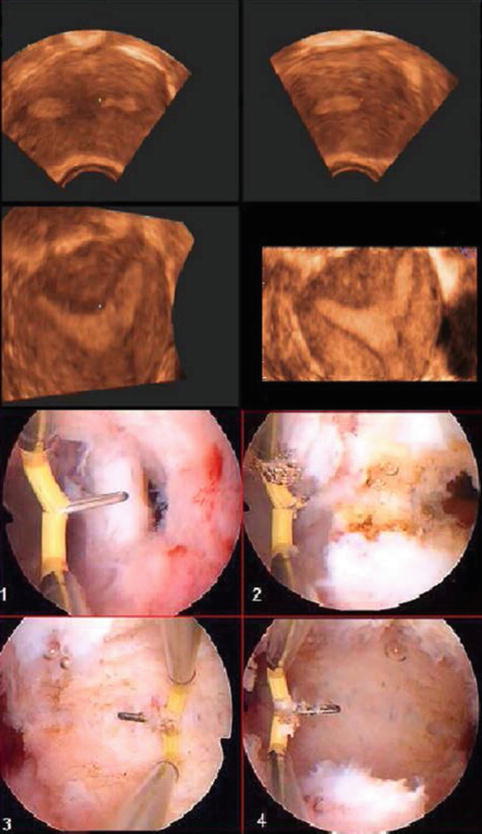
Fig. 3.2
Three-dimensional ultrasound and metroplasty of the uterine septum
3.2 Materials and Methods
A total of 114 women were investigated and their fertility outcome was followed for an average of 2 years. Patients with some degree of Mullerian malformation, as detected at their local gynecologist on transvaginal ultrasound or at our department during admission for any condition connected to the anomaly, were included in our study. The patients were assessed using B-mode, 3D ultrasound examinations using a Voloson 730 Expert (General Electric Healthcare, Zipf, Austria) with a vaginal multifrequency probe (5–9 Hertz). An initial B-Mode examination provided morphologic evaluation of the pelvic organs, including uterine size and endometrium thickness, followed by a saline infusion sonography in most of the patients with findings suggestive of a uterine septum. The operations were performed under general anesthesia using the following surgical technique for all patients. During hysteroscopy, the automatic pressure cuff (Olympus, Center Valley, PA) maintained an infusion pressure of 100 mmHg, and suction of 10–15 mmHg was applied to the outflow tube to achieve a sufficient flow. The TCRis resectoscope (Olympus), Ch. 26 model WA 22061 with 12 optic 22001A (Hamburg, Germany), using NaCl 0.9 % (Braun, Melsungen, Germany) as irrigant, with a needle of 5 mm was then used to perform the metroplasty. The needle was used with a bipolar cutting current of 280 W to incise the lower segments of the septum from side to side until the tubal ostia were visualized. The high power is needed for the ignition of the plasma only. A couple of milliseconds after the ignition, the generator automatically regulates the power down to normal values around 100 W. The septum excision was stopped approximately 10 mm from the line between the two ostia. In six patients, a total uterine septum was identified. In these cases, the incision was made horizontally toward the other obliterated cavity, starting just after the internal ostium. In cases with a double cervix the same procedure was performed leaving the cervices intact (Fig. 3.1). The received information was entered in statistical software (SPSS, version 14, SPSS 22 Inc., Chicago, IL). Patient characteristics of the study groups were analyzed with one way analysis of variance in case of normally distributed continuous variables, and Pearson’s chi-square test in case of dichotomous data. Confidence intervals for difference in means were calculated. Pearson’s chi-square was also used to analyze differences of preference among the study groups. A paired-samples t test was used to compare expected visual analog scale scores for both investigations. All tests were two-sided and P values < .05.
3.3 Results
One hundred fourteen women underwent hysteroscopic examination in case of larger than 1/4 of the uterine size septum a resection was performed, with a mean age of 31 (19–42 years). Eight small septum was found to be small and not in need of resection. Uterine septa were found as part of the workup for the following events: infertility workup (33.3 %), first trimester miscarriage (22.8 %), three or more miscarriages (22.8 %), Cesarean section (11.4 %), premature delivery (7.9 %), normal delivery (1.8 %) (Table 3.1). We evaluated the septum size in the 114 women. Ten (8.8 %) had a septum consisting one-quarter of their uterus, 18 (15.8 %) a septum one-half of their uterus, and 86 (75.4 %) a septum larger than one-half of their uterus. Six women had a total septum and were included in the septum larger than one-half of their uterus group. The different diagnostic events leading to diagnosis of the uterine septum per septum size is presented in Table 3.2. The uterine septum was successfully resected in all 106 women. No intra- or postoperative complications were noted. One hundred and three out of 114 women desired a future pregnancy. Seventy-two (69.9 %) of these women achieved a successful pregnancy after metroplasty, with 63 (87.5 %) subsequent term deliveries, and 9 (12.5 %) premature deliveries. Twenty-two (30.6 %) of the 72 women who had live births delivered by Cesarean section. Twenty-four (23.3 %) women who desired future fertility did not become pregnant, and 7 (6.8 %) had a spontaneous miscarriage. Eleven women were not interested in future fertility; however, they opted for surgery at time of diagnosis. In examining the outcomes in women divided up by group of septum diagnosis, we found the following rates of live birth following metroplasty: infertility workup (56.3 %), miscarriage (77.6 %), normal/premature delivery (80 %), and Cesarean section (66.7 %) (Table 3.1). We found different pregnancy outcomes after metroplasty of the various septum sizes as is presented in Table 3.2. To compare the pregnancy outcome after metroplasty of a different septum size the material was divided in two groups: one group with a septum size of one-quarter or one-half and one other group with a septum size larger than one-half of their uterus. The pregnancy outcome of a septum size one-quarter or one-half is significantly different from the pregnancy outcome after metroplasty of septum larger than one-half of the uterus (chi-square: P < .001). There were only four women in our study with the combination of a septum consisting one-quarter of their uterus and the diagnosis following a first trimester miscarriage. After metroplasty none of these women became pregnant, although all four had desired fertility. ANOVA linear regression showed no significant difference of age in the different events leading to diagnosis (P¼.708) and no significant difference in age and pregnancy outcome (P¼.160).
Table 3.1
Pregnancy outcome after metroplasty
Diagnosis following | Infertility workup | Miscarriagea | Normal/premature delivery | C-section | Total group |
|---|---|---|---|---|---|
Pregnancy outcome: | 38 (33.3 %) | 52 (45.6 %) | 11 (9.7 %) | 13 (11.4 %) | 114 |
Live birth | 18 (56.3 %) (3 premature) | 38 (77.6 %) (4 premature) | 8 (80 %) (1 premature) | 8 (66.7 %) (1 premature) | 72 (69.9 %) |
Miscarriage | 3 | 4 | – | – | 7 (6.8 %) |
No pregnancy | 11 | 7 | 2 | 4
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|