Fig. 13.1
Embolization of the fibroids
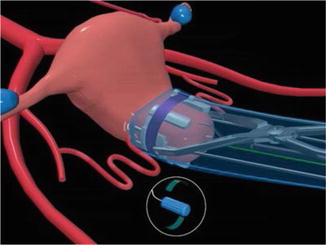
Fig. 13.2
Temporary clamping of the uterus
13.2 Uterus Circulation
Uterus has a very rich blood supply through two extrinsic arterial systems, the uterine and ovarian arteries. Intrinsic uterine arteries consist of ascending uterine, arcuate, radial, and peripheral arteries implicating free flow through the uterus. Fibroids receive their blood supply from the intrinsic arteries, primary from branches of arcuate arteries, and the vessels are located in the pseudocapsule around the fibroids. The ipsilateral uterine and ovarian arteries are connected by communicating branches. In addition to its primary (uterine artery) and secondary (ovarian artery) extrinsic blood supply, the uterus enjoys a vast network of lesser known arterial collaterals (Burbank and Hutchins 2000). If the blood supply from the right or left uterine artery is occluded, blood from the left or right artery will supply the myometrium by communications through arcuate arteries. Finally, if both uterine arteries are occluded, blood flow to the myometrium will develop from the ovarian arteries through communicating arteries. In addition to the primary and secondary blood flow, the uterus has a vast network of collateral arterial communication from the aorta external iliac and femoral artery branch (Chait et al. 1968) (Fig. 13.3).
Fig. 13.3
Blood supply to uterus
Diagram showing the extrinsic arteries of the left side of the uterus, including the aorta and the renal and ovarian arteries arising from the abdominal aorta, the uterine artery arising from the internal iliac artery, and the uteroovarian communicating artery. Symmetrical arteries are present on the right but are not shown.
13.3 Fibroid Life Cycle
Fibroid degeneration is the physiological way of terminating further growth of fibroids. Fibroids are particularly susceptible to degeneration because their rapid growths need increased blood supply. Fibroids have unsubstantiated connection to the uterine blood supply and as a consequence they frequently outgrow their blood supply, and consequently two thirds of the fibroids show degeneration (Huang et al. 1996). Larger fibroids are more frequently associated with degenerative changes compared to the smaller ones (Cramer et al. 1996). The different types of degenerative changes are hyaline or myxoid degeneration (75 %), calcification (10 %), cystic degeneration (10 %), fatty degeneration, and red degeneration during pregnancy (Fig. 13.4).
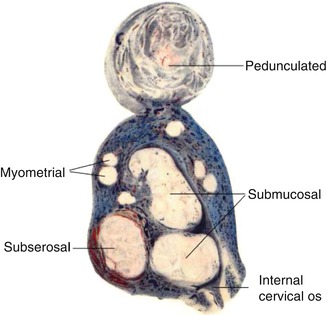
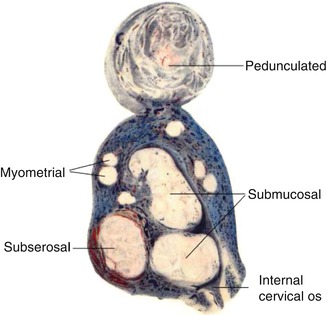
Fig. 13.4
Different types of fibroids and degeneration
13.4 Implication of Uterine Ischemia
When the uterine circulation is interrupted, unperfused myometrium quickly becomes hypoxic which will create pain. During ischemia, myometrial energy is derived anaerobically from the breakdown of glycogen through the glycolytic pathway (Laudanski 1985). After the uterine arteries are occluded, most blood stops flowing in myometrial arteries and veins, and the uterus becomes ischemic. It is postulated that myomas are killed by the same process that kills trophoblasts – transient uterine ischemia (Burbank 2004).
Over time, stagnant blood in these arteries and veins clots. Then, tiny collateral arteries in the broad ligament including communicating arteries from the ovarian arteries open and cause clots within myometrium to lyse and the uterus to reperfuse. Fibroids, however, do not survive this period of ischemia (Lichtinger et al. 2003). This is a unique organ response to clot formation and ischemia. After the uterine arteries are bilaterally occluded, either by uterine artery embolization or by laparoscopic obstruction, women with fibroids experience symptomatic relief after some time.
13.5 Practical Aspects of Procedure: Uterine Artery Occlusion
In 1964, Bateman reported the successful treatment of menorrhagia in four patients with fibroids and three with functional uterine bleeding (Bateman 1964). This was the first published article that demonstrates that uterine artery occlusion by ligation, division, or excision is an effective treatment for menorrhagia associated with fibroids and in patients without pathology.
Laparoscopic bipolar coagulation of uterine arteries and anastomotic sites of uterine arteries with ovarian arteries represents another modality of avoiding hysterectomy in some women (Liu 2000; Liu et al. 2001). This procedure was first described in 2000 in three women with symptomatic fibroids who required conventional surgical treatment. Uterine size and dominant fibroid size were assessed by ultrasonography before and after surgery. Both uterine arteries, as well as anastomosis zone of uterine arteries with ovarian arteries, were occluded in all three women. Surgery was uneventful, and patients were hospitalized for only 2 days. All women experienced improvement in symptoms with no complications. Postoperative ultrasound showed progressive reduction in size of the dominant fibroid (Liu 2000).
In another study 46 premenopausal women, age 43 (34–51) years with symptomatic uterine fibroids, undergoing radiologic embolization (n = 24) or laparoscopic closure of the uterine arteries (n = 22) (Hald et al. 2004, 2007; Istre et al. 2004). The laparoscopic technique reduced picture blood assessment score after 6 months by 50 % in both groups. Uterus volume was also reduced by 35–40 % in both groups. Postoperative pain and use of pain relief differed significantly, as patients required more pain medication after embolization: ketobemidon 38 mg compared with 16 mg in the laparoscopic group (P = 0.008). In conclusion, we found that laparoscopic occlusion of uterine vessels is a promising new method for treating fibroid-related symptoms, with less postoperative pain than embolization and comparable effects on symptoms.
Women with fibroid(s) unsuitable for laparoscopic myomectomy (LM) were treated with uterine artery embolization (UAE) or laparoscopic uterine artery occlusion (LUAO). Before the procedure, patients treated with UAE (n = 100) had a dominant fibroid greater in size (68 vs. 48 mm) and a mean age lower (33.1 vs. 34.9 years) than surgically treated patients (n = 100). After 6 months, mean shrinkage of fibroid volume was 53 % after UAE and 39 % after LUAO (p = 0.063); 82 % of women after UAE, but only 23 % after LUAO, had complete myoma infarction (p = 0.001). Women treated with UAE had more complications (31 vs. 11 cases, p = 0.006) and greater incidence of hysteroscopically verified intrauterine necrosis (31 vs. 3 %, p = 0.001). Both groups were comparable in markers of ovarian functions and number of nonelective reinterventions. The groups did not differ in pregnancy (69 % after UAE vs. 67 % after LUAO), delivery (50 vs. 46 %), or abortion (34 vs. 33 %) rates. The mean birth weight of neonates was greater (3,270 vs. 2,768 g, p = 0.013) and the incidence of intrauterine growth restriction lower (13 vs. 38 %, p = 0.046) in post-UAE patients.
Both methods are effective in the treatment of women with future reproductive plans and fibroids not suitable for LM. UAE is more effective in causing complete ischemia of fibroids, but it is associated with greater risk of intrauterine necrosis. Both methods are an effective treatment for PPH and fibroids. Pregnancy is possible after UAE. Recurrent PPH is a serious and frequent complication. Synechia is also a potential complication. Desire of childbearing should be considered when choosing embolization or surgery and, in case of embolization, the choice of material used (Berkane and Moutafoff-Borie 2010a). Further studies on future fertility after UAE are needed as well as information on fertility after surgery have low rate of serious complications (except for a high abortion rate) (Mara et al. 2012).
Hysteroscopic examination of the uterine cavity revealed that patients previously treated for intramural myoma(s) by uterine artery embolization had a significantly higher incidence of abnormal findings compared with patients treated by laparoscopic occlusion of uterine arteries (59.5 % vs. 2.7 %). In particular, there was a higher incidence of necrosis in the uterine cavity of patients subjected to uterine artery embolization (43.2 %) compared with patients after surgical uterine artery occlusion (2.7 %) (Kuzel et al. 2011).
UAE is used to treat postpartum hemorrhage (PPH) and fibroids. This effective therapy is replacing surgery in many cases. One of the main goals of UAE is to preserve the uterus and therefore fertility (pregnancies, menses, and ovarian reserve). Pregnancies after this technique have been described. The main complications encountered during these pregnancies are not only PPH but also miscarriages and cesarean deliveries after UAE for fibroids. Conflicting results varying from completely well tolerated to serious complications such as definitive negative effect on endometrium and ovary function have been reported. Nevertheless, the series differ in that they included women of different ages and used different materials for vessel occlusion (definitive microparticles of varying sizes, temporary pledgets of gelatin sponge, etc.).
UAE is an effective treatment for PPH and fibroids. Pregnancy is possible after UAE. Recurrent PPH is a serious and frequent complication. Synechia is also a potential complication. Desire of childbearing should be considered when choosing embolization or surgery and, in case of embolization, the choice of material used. Further studies on future fertility after UAE are needed as well as information on fertility after surgery (Berkane and Moutafoff-Borie 2010b).
Another new advanced technology is ExAblate 2100 system (Insightec Ltd, Haifa, Israel) for magnetic resonance imaging (MRI)-guided focused ultrasound surgery on treatment outcomes in patients with symptomatic uterine fibroids, as measured by the nonperfused volume ratio.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


