Whole medical systems
• Homeopathic medicine
• Naturopathic medicine
• Traditional Chinese medicine
• Ayurveda
• Tibetan medicine
Biologically based practices
• Herbal products
• Nutritional supplements
• Vitamins
• Dietary supplements
Mind-body medicine
• Meditation
• Biofeedback
• Relaxation
• Guided imagery
• Prayer
• Music therapy
• Tai Chi Chuan
Manipulative practices
• Chiropractic manipulation
• Massage
• Osteopathic manipulation
Energy medicine
• Acupuncture
• Qigong
• Reiki
• Therapeutic touch
Commonly utilized forms of CAM include biologically based practice, mind-body medicine, manipulative and body-based practice, and energy medicine. Biologically based practices of CAM employ the use of the substances from nature, including herbs, nutrition, vitamins, and dietary supplements. Mind-body medicine involves a variety of techniques designed to enhance the mind’s capacity to affect bodily functions and symptoms. Some examples of mind-body medicine include meditation, biofeedback, relaxation, guided imagery, prayer, and music therapy. (Refer to Chap. 34: Non-pharmacological Distraction Techniques as Sedation Adjunct.) Manipulative practices are based on manipulation and movement of the body. These include massage, chiropractic or osteopathic manipulation. Energy medicine employs the usage of energy fields. Some examples include acupuncture, qigong, reiki, and therapeutic touch.
Use of CAM in the pediatric population is increasing in popularity. In the United States, approximately 38 % of adults and 12 % of children currently use some form of complementary medicine [1]. The surgical environment is one in which CAM has become particularly popular with pediatric patients, families, and health care professionals. Pediatric patients require sedation more often than adults for medical procedures. They are at higher risk for respiratory depression and life-threatening hypoxia, and peri-procedure anxiety is directly related to fear, unfamiliar environments, and a loss of control. CAM can be used as a noninvasive modality for decreasing patients’ anxiety and assisting with sedation.
Music
Music has been widely used for healing purposes through the ages. It is recognized as a safe, inexpensive, and effective anxiolytic adjunct to medical procedures. Music therapy employs the use of experiencing or making music for therapeutic purposes. It can serve as an adjuvant therapy in critically ill patients. In a randomized controlled trial, ten critically ill patients were allocated to a music or a no-music group. The music group received a special selection of slow movements from Mozart’s piano sonatas, which had been analyzed for compositional elements for relaxation. The music was delivered for 1 h via headphones, where the control subjects wore headphones without music. Music application was shown to significantly reduce the amount of sedative medication needed to achieve a comparable degree of sedation. In those receiving the music intervention, plasma concentrations of growth hormone increased, whereas those of interleukin-6 and epinephrine decreased. The reduction in systemic stress hormone levels was associated with a significantly lower blood pressure and heart rate. Music may exert its sedative effects by a neurohumoral pathway involving interactions between the hypothalamo-pituitary axes with the adrenal medulla via mediators of the unspecific immune system [2]. A multicenter randomized controlled trial utilized music therapy to help reduce anxiety and sedation among 373 patients receiving mechanical ventilation for acute respiratory failure. The music intervention group (126 patients) could select their preferred pieces of music to listen to as they wanted. The patient-directed music listening group had relative decreases of about 36 % in anxiety, sedation intensity, and sedation frequency as compared with usual care [3].
The use of intraoperative music in awake patients decreases patient-controlled sedative and analgesic requirements. A randomized controlled study of 35 adults undergoing urologic procedures with spinal anesthesia and patient-controlled intravenous propofol sedation randomly assigned patients to intraoperative music via headset or to no intraoperative music. The patients in the music group required significantly less propofol for sedation than patients in the control group [4]. A randomized controlled study of 43 adults undergoing lithotripsy treatment of renal or ureteral calculi and receiving patient-controlled intravenous opioid analgesia also randomly assigned patients to either a music or no-music group. The patients who listened to music had a significant reduction in alfentanil requirements [4]. By using self-report validated behavioral and physiological measures of anxiety, 93 adult patients were evaluated before, during, and after surgery. Patients who listened to music of their choice during the preoperative period reported less anxiety [5].
A randomized controlled trial of 70 children undergoing surgical procedures indicated that children are less anxious and show increased compliance during induction when exposed to a single care-provider in a dimmed, quiet operating room with background music [6]. In another study, 123 children were randomly assigned into one of three groups: interactive music therapy, oral midazolam, and a control group. The children who received midazolam were significantly less anxious during the induction of anesthesia than the children in the music therapy and control groups. There was no difference in anxiety during the induction of anesthesia between children in the music therapy group and children in the control group. Music therapy may be helpful on separation and entrance to the operating room, depending on the therapist; however, it does not appear to relieve anxiety during the induction of anesthesia [7].
Sixty pediatric patients receiving either chloral hydrate or music therapy for electroencephalography testing revealed that music therapy may be a cost-effective, risk-free alternative to pharmacological sedation [8]. There has been report of a high success rate of utilizing music for pediatric patients undergoing computerized tomography scans, echocardiograms, initiation of intravenous lines, and electroencephalograms (EEGs). Music therapy is a cost-effective intervention for most pediatric facilities [9]. It can be used as an adjuvant therapeutic measure in pediatric sedation.
Hypnotherapy
Hypnotherapy is the induction of a trance-like state to facilitate relaxation of the conscious mind. The hypnotic trance is neither a sleep state nor a state of unconsciousness. It is a state of altered consciousness in which attention can be focused on some things to the exclusion of others. Relaxation, immobilization, and altering or abolishing painful stimuli are frequently seen with hypnosis. A study of 49 embolization procedures on 30 patients utilizing medical hypnosis revealed that 45 of the procedures were successfully performed using hypnosis [10].
Faymonville et al. did a study of positron emission tomography in 11 healthy volunteers to identify the brain areas in which hypnosis modulates cerebral responses to a noxious stimulus. Hypnosis decreased both pain sensation and the unpleasantness of noxious stimuli. Noxious stimulation caused an increase in regional cerebral blood flow in the thalamic nuclei and anterior cingulate and insular cortices. The hypnotic state induced a significant activation of a right-sided extrastriate area and the anterior cingulate cortex. The interaction analysis showed that how the activity in the anterior cingulate cortex was related to pain perception and unpleasantness was different from the hypnotic state than in control situations. Both intensity and unpleasantness of the noxious stimuli were reduced during the hypnotic state [11].
Lang and colleagues did a randomized study of 236 women referred for large core needle breast biopsy to receive standard care, structured empathic attention, or self-hypnotic relaxation during their procedures. The study demonstrated that hypnosis can be successfully integrated to core needle biopsy for the diagnosis of breast cancer. The adjunctive use of hypnosis by trained members of the procedure team resulted in substantially less anxiety and a reduction in pain, compared to two other randomized conditions: routine care and sympathetic assistance. After more than an hour, the hypnotic analgesia was clearly superior to that obtained in standard care or the nonspecific empathy conditions [12].
A study explored the use of hypnosis for pain and anxiety management in six colonoscopy patients who received a hypnotic induction and instruction in self-hypnosis on the day of their colonoscopy, compared to ten consecutive patients who received standard care. Hypnosis appeared to be a feasible method of managing anxiety and pain associated with colonoscopy, reduced the need for sedation, and may have other benefits, such as reduced vasovagal events and recovery time [13].
Ghoneim et al. did a randomized controlled trial of 60 patients to evaluate the usefulness of tape-recorded hypnosis instruction on perioperative outcome in surgical patients. The hypnosis group received an audio tape to listen to daily for the immediate preoperative week. The controlled group did not receive a tape. Anxiety was reduced before surgery by means of the audio tape containing hypnotic instructions, however, for no discernible reason, and there was an increase in the incidence of vomiting [14]. Balini et al. studied 46 patients undergoing percutaneous transluminal coronary angioplasty of the left anterior descending coronary artery. They were randomized to receive medication or hypnotic sedation during the procedure. The increase in cardiac sympathetic activity associated with balloon inflation and myocardial ischemia during percutaneous transluminal coronary angioplasty of the left anterior descending coronary artery was selectively eliminated by hypnosis but not by drug sedation [15].
A meta-analysis performed on 18 controlled trials suggested that the addition of hypnosis substantially enhanced treatment outcome. The average client receiving cognitive-behavioral hypnotherapy showed greater improvement than at least 70 % of clients receiving non-hypnotic treatment. Hypnotherapy enhances the effects of cognitive-behavioral psychotherapy, including anxiety, insomnia, pain, and obesity [16].
Hypnotherapy is one of the oldest forms of psychotherapy. It encourages the patient to use his or her imagination to improve health and health behaviors. While most of the current research is on its use in the adult population, hypnotherapy may be integrated into pediatric sedation in the future.
Guided Imagery
Patients who undergo sedation usually experience some fear and apprehension about their procedures. Guided imagery is a simple, low-cost therapeutic tool that can help counteract these feelings. A randomized controlled trial of 130 patients underwent elective colorectal surgical procedures. They were assigned to receive either routine perioperative care or listen to guided imagery tapes for 3 days before their procedures, during the peri-procedure period, and for 6 days after the intervention. The patients in the guided imagery group experienced considerably less preoperative and postoperative anxiety and pain, and required nearly 50 % less narcotic medications than patients in the control group [17].
Guided imagery was successfully utilized in 56 patients undergoing radiology interventional procedures. They were enrolled in a standardized protocol with script guided imagery to produce a state of self-hypnotic relaxation. Each of the patients developed an imagery scenario. Although there were common trends in the chosen imagery, such as nature, travel, family, home, and personal skills, the chosen topics were highly individual. This variable made prerecorded tapes or provider-directed imagery unlikely to be equally successful [18].
Anodyne imagery technique consists of conditioned relaxation, induction of a trance state, and guided processing of the patient’s internal imagery. A study involved 100 patients undergoing interventional radiologic procedures. Anodyne imagery eased patients’ anxiety and fears and reduced the amount of midazolam and fentanyl used during interventional radiologic procedures, possibly improving procedural safety and augmenting the speed of recovery [19].
Guided imagery technique can produce analgesia and anxiolysis. Though the technique is highly individualized, it has a potential to be integrated into pediatric sedation in the future.
Acupuncture and Related Techniques
Used for more than two millennia, acupuncture is one of the oldest medicinal practices in the world. It is part of traditional Chinese medicine. Since its reintroduction in the United States in the early 1970s, acupuncture has become a widely used complementary medical therapy, used to maintain and restore health through the stimulation of acupuncture points by the insertion of hair-thin needles through the skin. In traditional Chinese Medicine and acupuncture, illness is caused by imbalance of a person’s energy called qi. Qi is created between heaven and earth. Qi flows through the entire body of living creatures. Acupuncture promotes the flow of “qi,” which is equivalent to energy. Endogenous opioid peptides in the central nervous system play a major role in mediating the effect of acupuncture [20]. Several acupuncture-related techniques, including electro-acupuncture, moxibustion, cupping, acupressure, and auricular therapy, are commonly applied. Complications from acupuncture treatment are rare.
Acupuncture can be used to assist upper endoscopic and colonoscopy procedures. In a study of 106 patients, those receiving midazolam rated the procedure as slightly less troublesome than those receiving acupuncture. Oxygen saturation, blood pressure, and heart rate were significantly lower in patients receiving midazolam [21]. In a randomized controlled trial of 55 patients who received colonoscopy examination with either electro-acupuncture analgesia or meperidine analgesia, the analgesic effect of both groups was the same. The electro-acupuncture group has fewer side effects, particularly in regard to dizziness. Serum concentration of beta-endorphin in both groups showed similar trends of change during colonoscopy. Changes in serum concentration of epinephrine, norepinephrine, dopamine, cortisol, and beta-endorphin were also similar between these two groups [22]. Another study of 30 patients undergoing colonoscopy was randomized to receive acupuncture, sham, or no acupuncture. Midazolam was used for sedation for all three groups. The acupuncture group experienced less pain and required less midazolam than the other two groups. The demand for sedative drugs during colonoscopy was decreased through the use of acupuncture by reducing the discomfort and anxiety of the patients [23].
In a study of 56 patients undergoing lithotripsy procedures, patients were enrolled into either an acupuncture or sham group. Using a combination of auricular and body acupuncture, patients had less pre-procedural anxiety and required less intra-procedural analgesia [24]. Another study involving 35 patient undergoing lithotripsy procedures showed that electro-acupuncture was an effective method for inducing sedation with analgesia without any demonstrable side effects [25].
Acupuncture or acupressure on the extra-one, EX-HN3, (Yin-Tang) acupuncture point is effective in producing sedation. The extra-one, EX-HN3, (Yin-Tang) acupuncture point is located on the forehead, at the midpoint between the eyebrows (Fig. 32.1).
Fig. 32.1
Extra-one, EX-HN3, (Yin-Tang) acupuncture point locates on the forehead, at the midpoint between the eyebrows
A prospective, randomized, single-blind, controlled study assigned 52 patients either to acupuncture on Yin-Tang or to a sham acupuncture group. The bispectral index (BIS) values in the acupuncture group were significantly lower than in the sham group [26].
A study of 50 patients was randomly assigned to acupuncture of the Yin-Tang point or control point. Acupuncture application significantly decreased the BIS value compared to the control group [27].
Acupressure over this point produces analgesic and sedative effects. A study of 52 children undergoing endoscopic procedures was randomized to receive acupressure bead intervention either at the extra-one (Yin-Tang) acupuncture point or at a sham point. Anesthetic techniques were standardized and maintained with intravenous propofol infusion. Children receiving the acupressure on the extra-one (Yin-Tang) point experienced reduced anxiety. There were no significant changes in BIS values between the groups, and the total intra-procedural propofol requirements did not differ between them. Acupressure bead intervention at the extra-one (Yin-Tang) acupuncture point reduced pre-procedural anxiety in children undergoing endoscopic procedures, however [28]. A study involving 22 healthy female volunteers was randomized to receive acupressure on either the extra-one (Yin-Tang) point or a sham point. Acupressure at the extra-one (Yin-Tang) point significantly reduced needle insertion pain compared to acupressure at the sham point. Acupressure at the extra-one (Yin-Tang) acupuncture point significantly reduced the low frequency/high frequency ratio of heart rate variability responding to needle insertion. This implies a reduction in sympathetic nervous system activity [29].
A crossover study of volunteers indicated that acupressure on the extra-one (Yin-Tang) acupuncture point can significantly reduce BIS values and verbal stress scores [30, 31]. In a randomized controlled trial of 48 volunteers, 5 min of acupressure on the extra-one (Yin-Tang) acupuncture point significantly reduced the EEG spectral entropy values [29]. A randomized trial of 61 parents indicated that acupressure at the extra-one (Yin-Tang) acupuncture point can have anxiolytic and sedative effects on parents in the preoperative holding area before their children’s surgery [32].
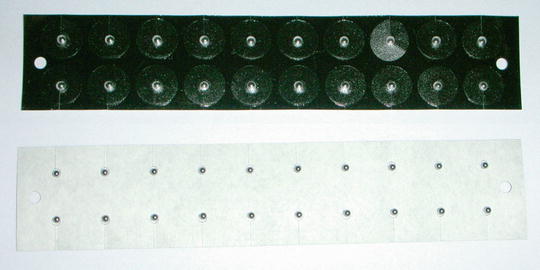
Ear acupuncture (Fig. 32.2), also known as auricular therapy, is based on the principles of traditional Chinese medicine. It is practiced as a sole treatment or in conjunction with body acupuncture therapy, and is an effective treatment for acute anxiety. Ear acupuncture can decrease preoperative anxiety in adults undergoing outpatient surgery [33]. A study of 67 patients undergoing dental extraction compared the efficacy of auricular acupuncture, intranasal midazolam, placebo acupuncture, and no treatment for reducing dental anxiety. Patients having dental extractions were randomized to one of four groups: auricular acupuncture, placebo acupuncture, intranasal midazolam, and a no-treatment group. Anxiety was assessed before the interventions, after 30 min, and after the dental extraction. The auricular acupuncture group and the midazolam group were significantly less anxious at 30 min compared to patients in the placebo acupuncture group. Patient compliance assessed by the dentist was significantly improved if auricular acupuncture or application of intranasal midazolam had been performed [34].
Fig. 32.2
Location of auricular acupuncture points
Auricular acupuncture points may be stimulated for a longer period of time by using ear seeds or ear tacks. Ear seeds can be small seeds from the dry Vaccaria plant or can be made from stainless steel. These seeds are held in place on the ear with a small piece of adhesive tape (Fig. 32.3). Auricular acupressure is an effective treatment for anxiety during ambulance transport. In a study of 36 patients who required ambulance transport to medical facilities, patients were randomized to receive auricular acupressure at the relaxation point or at a sham point. Patients in the auricular acupressure group reported significantly less anxiety than patients in the sham group on arrival at the hospital [35]. Another randomized controlled trial of 38 patients with acute hip fractures received either bilateral auricular acupressure or the sham control during ambulance transport. Patients in the true intervention groups had less pain and anxiety and lower heart rates on arrival at the hospital [36].