20 Urticaria and Angioedema
Etiology and Pathogenesis
Urticaria is characterized by the waxing and waning appearance of pruritic, erythematous papules or plaques with superficial swelling of the dermis (Figure 20-1). The swelling observed with urticaria and angioedema results from the movement of plasma from small blood vessels into adjacent connective tissue. Unlike atopic dermatitis, the pruritus of urticaria is driven by histamine. Histologically, urticarial lesions consist of a lymphocyte-predominant perivascular infiltrate. In CIU, the cellular infiltrate is similar to that seen in allergen-induced late phase skin response, and the cytokine profile is both TH1 and TH2.
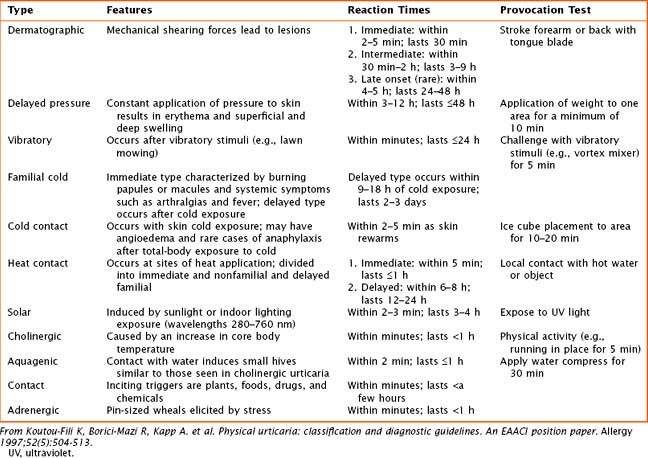
Physical Urticaria
Physical urticarias have a specific trigger that directly induces hives within minutes, with hives lasting minutes to a few hours. Physical urticarias are further classified into multiple subtypes (Table 20-1), each having a different physical trigger; thus, an individual can have more than one subtype. Mast cell degranulation is included in the pathogenesis of most subtypes of physical urticaria, including dermatographic, cholinergic, cold, and solar urticaria, but serum immunoglobulin may also be involved as demonstrated by passive transfer experiments.
Angioedema
Angioedema, which is a swelling of the dermis, subcutaneous, and submucosal tissues, often coexists with urticaria but typically persists past 24 hours (Figure 20-2). Angioedema is described as painful or burning in quality. The lack of pruritus in angioedema may be caused by fewer mast cells in the lower dermis and subcutis. Idiopathic angioedema coexists with urticaria, occurring in up to 50% of those with CIU. Angiotensin-converting enzyme (ACE) inhibitors can also trigger angioedema via the bradykinin pathway.
Clinical Presentation
Patients with long-lasting lesions or the presence of other systemic symptoms should be evaluated for other diseases (see Box 20-1). Urticarial vasculitis is classified by painful or pruritic lesions lasting longer than 48 hours and may leave residual skin changes unrelated to excoriation. Concurrent systemic complaints or abnormal laboratory findings indicative of an inflammatory process, such as an elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) or low complement levels, are seen. A skin biopsy is required to rule out urticarial vasculitis. Urticaria pigmentosa, a subset of mastocytosis, may mimic urticaria, although these lesions are typically pigmented and last longer than urticaria. The presence of fever with urticaria can occur in Schnitzler’s syndrome and Muckle-Wells syndrome. Schnitzler’s syndrome is described as recurrent urticaria with arthralgia, fever, and elevation in inflammatory markers in association with an elevation in IgM. Muckle-Wells syndrome is a periodic fever syndrome with urticaria associated with periodic, unexplained fevers.