aAll macroscopically visible lesions—even with superficial invasion—are allotted to stage IB carcinomas. Invasion is limited to a measured stromal invasion with a maximal depth of 5.00 mm and a horizontal extension of no >7.00 mm. Depth of invasion should not be >5.00 mm taken from the base of the epithelium of the original tissue—superficial or glandular. The depth of invasion should always be reported in millimeter, even in those cases with “early (minimal) stromal invasion” (~1 mm).
bOn rectal examination, there is no cancer-free space between the tumor and the pelvic wall. All cases with hydronephrosis or nonfunctioning kidney are included, unless they are known to be due to another cause.
Source: From Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105:103–104.
Surgical findings and radiographically guided biopsies of suspected lesions cannot be used to change or modify clinical FIGO staging. Stage IVA requires biopsy confirmation of bladder or rectal mucosal involvement. Stage IIIB indicates pelvic sidewall involvement or demonstration of a nonfunctioning kidney or hydronephrosis.
A TNM (Tumor, Node, Metastasis) staging system is proposed by American Joint Committee Commission on Cancer (AJCC) and is mainly used in documenting findings on surgical and pathologic evaluations as the pathologic stage of the disease. If there is ambiguity regarding the correct stage when two qualified professionals evaluate the patient, the lower stage is assigned.
Pretreatment Nodal Staging
The presence of paraaortic lymph node metastases is known to have a significant impact on progression-free and overall survival. Pretreatment knowledge of paraaortic spread could potentially direct treatment in a manner that could improve outcomes. Given the limitations of imaging in reliably detecting paraaortic micrometastases, surgical staging has been used. However, the role of surgical staging for locally advanced cervical cancer remains unclear.
PATHOLOGY
KEY POINTS
- Squamous CIS is a precursor lesion of invasive squamous carcinoma.
- Untreated squamous CIS results in invasive carcinoma in about one third of cases over a period of 10 years.
- Adenocarcinoma accounts for 20% to 25% of cervical carcinomas and is associated with HPV (usually type 18, but sometimes type 16).
- Adenosquamous carcinomas appear to be either histologically more aggressive or diagnosed at a later stage than adenocarcinomas of the uterine cervix.
Squamous Cell Carcinoma
Preinvasive Disease
Squamous CIS is a precursor lesion of invasive squamous carcinoma, and it is characterized by full-thickness atypia of the cervical epithelium. Endocervical glands may also be involved. The normal maturation of squamous epithelium is absent. There is no breach of the underlying basement membrane.
Microinvasive Carcinoma
Microinvasive squamous carcinoma is associated with squamous intraepithelial neoplasia, and it is characterized by small nests of cells that have escaped the basement membrane of the surface or glandular epithelium. Microinvasive carcinoma often displays cells that are larger, with more abundant eosinophilic cytoplasm than cells in the adjacent dysplasia.
A diagnosis of microinvasive squamous carcinoma of the cervix requires a loop electrosurgical excisional procedure or conization biopsy that encompasses the entire lesion and has negative margins (Fig. 7.1).
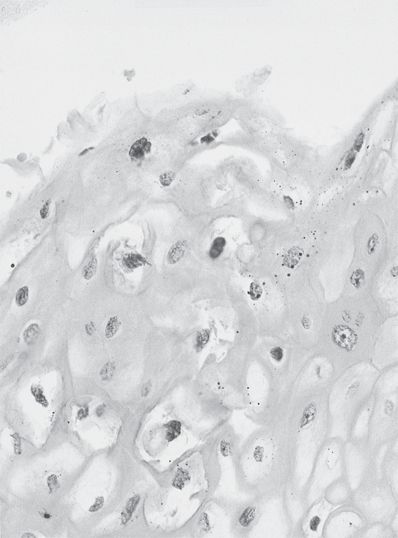
Figure 7.1 HPV changes. This squamous epithelium displays cells with large halos surrounding atypical nuclei (“koilocytotic atypia”).
Invasive Squamous Cell Carcinoma
Invasive cervical carcinoma arises from high-grade dysplasia, which may be detected up to 10 years before invasive carcinoma develops. Untreated squamous CIS results in invasive carcinoma in about one third of cases over a period of 10 years. Invasive carcinoma occurs most often after the age of 40 years, although it may be seen in young women. It is associated with HPV infection in more than 99% of cases. These tumors may consist of firm, indurated masses, or they may be ulcerated or polypoid. Microscopic examination reveals irregular, haphazardly infiltrating nests of cells with eosinophilic cytoplasm and enlarged, atypical, hyperchromatic nuclei.
Lymphatic and vascular space invasion may be present, especially in more deeply invasive tumors. Invasive squamous carcinomas are also graded, although treatment protocols do not depend on grade, and the histologic grade may not correlate with prognosis. Lesions are graded 1 to 3 (well, moderately, and poorly differentiated). Grade 2 (moderately differentiated) tumors represent the majority of invasive squamous carcinomas of the uterine cervix and are usually nonkeratinizing squamous carcinomas with nuclear pleomorphism, numerous mitoses, and an infiltrative pattern. Grade 3 (poorly differentiated) tumors either have smaller cells without neuroendocrine differentiation or are pleomorphic with anaplastic nuclei and sometimes a tendency to form spindle cells that must be distinguished from sarcoma by positive cytokeratin stains.
Adenocarcinoma
While the incidence of squamous carcinoma of the cervix has decreased in the past decades owing to cytologic screening, the number of cases of cervical adenocarcinoma has increased. Adenocarcinoma accounts for 20% to 25% of cervical carcinomas.
Adenocarcinoma in situ (AIS) is a precursor of invasive adenocarcinoma. It is found adjacent to many invasive adenocarcinomas, often accompanied by squamous dysplasia. Both AIS and invasive adenocarcinoma of the cervix are associated with HPV (usually type 18, but sometimes type 16).
AIS is characterized by preservation of the overall endocervical gland architecture. However, endocervical glands and surface epithelium are replaced to varying degrees by cells displaying atypia. Most adenocarcinomas in situ occur near the transformation zone, and skip lesions are unusual.
Other Epithelial Tumors
Adenosquamous carcinoma is a tumor composed of admixed malignant glandular and squamous elements. A recent multi-institutional study found that adenosquamous carcinomas are more commonly associated with higher tumor grade (p < 0.001) and vascular invasion (p = 0.002) than are adenocarcinomas. Adenosquamous carcinomas appear to be either histologically more aggressive or diagnosed at a later stage than adenocarcinomas of the uterine cervix.
Small Cell Carcinoma
Most neuroendocrine tumors seen in the uterine cervix represent small cell carcinomas. Even a small component of small cell carcinoma in a tumor of mixed type is associated with adverse outcome. These tumors are morphologically identical to those seen in small cell carcinoma of the lung. They are aneuploid tumors that show a strong association with type 18 HPV. Immunohistochemical stains for neuroendocrine markers, such as chromogranin and synaptophysin, may be helpful in the diagnosis. CD56 (neural cell adhesion molecule) is a sensitive marker for the diagnosis of small cell cancer in the cervix.
Mixed Epithelial, Mesenchymal Tumors, and Other Malignant Tumors
Uncommon malignant tumors of the cervix include sarcomas, malignant mixed müllerian tumors, endometrial stromal sarcomas, melanomas, granulocytic sarcomas, primitive neuroectodermal tumors, desmoplastic small round cell tumors, and primary germ cell tumors. Primary extranodal lymphomas of the uterine cervix are usually diffuse B-cell neoplasms.
PROGNOSTIC FACTORS
KEY POINTS
- Size of the primary tumor, depth of stromal invasion, lymphovascular invasion, and parametrial involvement have been correlated with disease-free survival in patients undergoing radical hysterectomy (RH).
- While FIGO stage is prognostically significant in predicting outcome, lymph node involvement is, in most studies, the most significant negative prognostic factor.
Tumor Size, Volume, and Margin Status
Size of the primary tumor, depth of stromal invasion, and parametrial involvement have been correlated with disease-free survival in patients undergoing RH. Lymphovascular space invasion and depth of cervical stromal invasion have also been associated with significantly poorer prognosis.
Size has also been correlated with increased pelvic failure rates in patients treated definitively with radiation. In patients with stage IB cervical cancer treated surgically, with or without RT, positive margin status conveyed a hazard ratio of 3.92 compared to negative margins. Also, margin status (distance in millimeter in patients with close margins) was significantly associated with an increased recurrence rate. In this series, postoperative RT eliminated local recurrences in patients with close margins and halved the recurrence rate in patients with positive margins.
Stage
The FIGO stage is universally accepted for its prognostic significance. Paraaortic node metastasis confers a much greater risk than measures of tumor volume, however, and emphasizes the fact that FIGO staging does not take into account important prognostic information such as nodal status.
Nodal Status
Lymph node involvement is, in most studies, the most significant negative prognostic factor. Reports emphasize higher 5-year survival rates (90% or higher) among surgically treated patients with no evidence of metastasis in the regional nodes, compared to patients with positive pelvic (50% to 60%) or paraaortic nodes (20% to 45%).
Lymphovascular Space Invasion
LVSI proved to be a significant prognostic factor in a surgical–pathologic study of 542 patients completed by the Gynecologic Oncology Group (GOG). Disease-free survivals were 77% and 89%, respectively, in patients with and without LVSI. Furthermore, LVSI was shown to correlate with pelvic adenopathy and with time to recurrence.
Hypoxia and Anemia
The presence of both hypoxia and anemia has been independently correlated in multiple studies with adverse outcomes in patients with cervical cancer. The data regarding anemia’s impact are largely retrospective, while hypoxia has been studied through direct tumor measurements in patients treated definitively with surgery as well as with radiation therapy. Studies have not confirmed the hypothesis of a direct correlation between anemia and tumor hypoxia, and the relationship between these two prognostic factors is complex. Several authors have suggested that a lower hemoglobin level could also be a marker for more aggressive disease as opposed to a physiologic variable that could be manipulated for therapeutic benefit.
Histopathology
Conflicting data exist regarding the prognostic significance of adenocarcinoma as compared with squamous cell carcinoma, with some studies suggesting similar survival rates for comparable stages and others suggesting inferior survival in the adenocarcinoma subgroup. There is evidence that adenosquamous carcinoma is either a histologically more aggressive tumor than cervical adenocarcinoma or is diagnosed later in the disease course.
Higher tumor grade and vascular invasion are statistically more common in adenosquamous carcinoma than adenocarcinoma of the cervix. The presence of small cell neuroendocrine carcinoma in any amount, even when associated with other types of neoplasm, is an independent prognostic factor associated with aggressive tumor behavior.
GENERAL MANAGEMENT AND RESULTS OF TREATMENT
KEY POINTS
- A quadrivalent vaccine targeting HPV types 16, 18, 6, and 11 is now recommended for all women of ages 9 to 26.
- As up to 30% of CIN and invasive cancers are caused by strains not in the vaccine, women who receive the vaccine are recommended to be followed according to guidelines already set for cytologic smears.
- Severe dysplasia/CIN and CIS are adequately managed with local therapies such as conization, laser ablation, cryotherapy, or a simple hysterectomy.
- Stage IA1 carcinoma is usually treated with conization or hysterectomy.
- Stage IA2 squamous cell carcinoma is a modified (type II) radical hysterectomy (MRH) and pelvic lymphadenectomy, although curative-intent RT is an equivalent option.
- Radical surgery and definitive chemoradiation have similar good outcomes for stage IB to IIA nonbulky tumors.
- Bulky IB2, IIB, IIIB, and IVA tumors are treated with curative-intent chemoradiation.
PREVENTION: HPV VACCINATION
Currently, there are two FDA-approved HPV vaccines that have been shown in randomized clinical trials to be highly effective in protecting against high-risk HPV infections. Both Gardasil (quadrivalent vaccine) and Cervarix (bivalent vaccine) protect against HPV types 16 and 18, the cause of 70% of cervical cancers and 50% of precancerous cervical lesions. Gardasil also protects against HPV 6 and 11, which are responsible for approximately 90% of genital warts. In addition to cervical cancer prevention, Gardasil is also approved for prevention of anal, vaginal, and vulvar cancers in women, as well as the prevention of anal and penile cancers in men. The American College of Obstetricians and Gynecologists recommends the quadrivalent or bivalent HPV vaccine for all women aged 9 to 26 years. As up to 30% of CIN and invasive cancers are caused by strains not in the vaccine, all women who receive the vaccine should follow standard screening recommendations. The HPV vaccine is given at 0, 2, and 6 months. The HPV vaccine is not effective in those with active HPV infection and abnormal cytology.
Severe Dysplasia and Carcinoma In Situ
Patients with severe dysplasia/CIN and CIS have essentially no risk of lymphatic involvement and are often treated with local therapies such as conization, laser ablation, cryotherapy, or a simple hysterectomy. These various techniques have comparable efficacy. Patients with HIV infection, high HPV viral load, positive margins, older age, and residual high-risk infection following conservative management have a higher recurrence rate. Reported rates of recurrent CIS and invasive cancer following therapeutic conization are low (<5%).
Factors associated with persistent disease or invasive cancer following cold knife conization include residual CIN 3, positive ectocervical and endocervical margins, multiquadrant disease, age greater than 50, and positive endocervical curettings. Patients with positive ECC after conization or positive endocervical margins on a cone specimen for CIS should have repeat conization prior to hysterectomy to avoid inappropriate treatment for invasive disease.
Since patients with CIS have virtually no risk of pelvic adenopathy, it is also appropriate to treat with only intracavitary RT. Tumor control rates of 100% have been reported. Grigsby and Perez successfully treated 21 such patients with a single intracavitary implant, delivering a mean point A dose of 46.12 Gy; no treatment sequelae were observed.
Stage IA
The concept of “microinvasion” (equating to FIGO stage IA) should define tumors that penetrate the basement membrane but have little or no risk of nodal involvement or dissemination. All macroscopically visible lesions are considered stage IB tumors.
Stage IA1 carcinoma is usually treated with conization or extrafascial hysterectomy. The control rate approaches 100%. Absence of LVSI plays a key role in opting for the conservative management of patients with MID as its presence may herald a higher incidence of lymphatic involvement as well as tumor recurrence.
Patients with FIGO IA2 disease with LVSI are not candidates for conservative surgical approaches in most circumstances. The recommended treatment for stage IA2 squamous cell carcinoma is a modified (type II) RH and pelvic lymphadenectomy, although curative-intent RT is an equivalent option. The average pelvic lymphatic metastasis rate from reported data is 5% to 13%. In patients who are medically inoperable, intracavitary RT may be used, with several series documenting excellent outcomes and low complication rates.
Adenocarcinoma Early Disease
The incidence of cervical adenocarcinoma has increased in the past 40 years. Almost all AIS lesions are associated with HPV, with 18 being the predominant type. The management of AIS is controversial. The term “microinvasion” may be inaccurate in describing glandular lesions as an accurate measurement of depth of invasion in glands may be difficult. The overall rate of residual disease in hysterectomy specimens after conization with negative margins is 25% and with positive margin is around 50%. Given the critical role of margin status post-conization, a cold knife technique may be preferred in patients with AIS. The recommended surveillance after conization for AIS includes cytology and ECC every 4 months. The most successful conservative management protocols require negative margins and no LVSI, and careful counseling and follow-up are warranted.
Stages IB to IIA (Nonbulky)
Stage IB is divided into IB1 (lesions < 4 cm) and IB2 (lesions confined to cervix > 4 cm). IB1 lesions and selected IIA lesions without extensive vaginal involvement can be treated with either RH and PLD (followed by tailored chemoradiation as indicated by surgical findings) or primary chemoradiation. Surgery is the preferred option in younger women as ovarian function and vaginal length, and thus sexual function, can generally be maintained. Transposition of the ovaries to the abdominal wall or the gutters away from the field of RT may prevent radiation-induced ovarian failure. Retention of ovarian function following ovarian transposition and postoperative radiation has been reported to range from 53% to 71%. The rate of ovarian metastasis is very low, about 0.9%, and thus, salpingo-oophorectomy is not part of RH.
Radical surgery and definitive chemoradiation have similar good outcomes. Typically, 5-year survival for stage IB patients is 85% to 90% and 65% to 75% for stage IIA. In a prospective study of RH ± RT (patients with parametrial involvement, deep stromal invasion, and/or positive nodes received postoperative RT) versus RT alone, no difference was seen in disease-related outcome. In the RH arm, 54% (62 out of 114) and 84% (40 out of 55) of stages IB1 and IB2 received postoperative RT, respectively. Severe morbidity was seen in 28% in the surgical arm (mostly combined surgery and RT) compared to 12% in the RT arm.
Stage IB patients who undergo radical surgery and are found to have poor prognostic pathologic features should receive adjuvant RT to decrease their risk for local recurrence. This high-risk group of patients is defined by the presence of two more of the following risk factors: lymphovascular space involvement, >1/3 stromal invasion, tumor size >4 cm. In a prospective study of adjuvant RT versus observation in this group of high-risk stage IB patients after surgery, adjuvant RT decreased the rate of local recurrence by 46% and progression-free survival by 42% at 10-year median follow-up for patients still alive at last contact.
Fertility-Sparing Surgery/Radical Vaginal and Abdominal Trachelectomy
Almost 30% of women diagnosed with cervical cancer will be less than 40 years of age and 40% will have early stage I disease. Preservation of fertility can be a major consideration in treatment if an acceptable oncologic outcome can be obtained. Recently, there have been major advances in fertility-sparing surgery (FSS) in women with stage IA2 to IB1 cervical cancers with the introduction of a procedure that involves transvaginal resection of cervical and paracervical tissues (vaginal radical trachelectomy) and proximal vaginal, placement of a permanent cerclage at the cervicouterine junction, and a laparoscopic pelvic lymphadenectomy.
The overall recurrence rate in the literature is about 4%, comparing favorably with standard treatment. Appropriate lesions include FIGO stage IA1 without extensive LVSI and IA2 or IB1 lesions less than 2 cm with limited endocervical involvement. A review reported that of patients electing FSS, 43% attempt conception, 70% conceive, 49% deliver at term, and 15% have cervical stenosis causing infertility.
Bulky IB Carcinoma of the Cervix
Bulky endocervical tumors and the so-called barrel-shaped cervix cancers have a higher incidence of central recurrence, pelvic and paraaortic lymph node metastasis, and distant dissemination. Historically, adjuvant extrafascial hysterectomy following preoperative RT was an accepted treatment approach. The GOG performed a randomized trial in which 256 eligible patients with carcinomas of the cervix ≥4 cm were treated with external beam and intracavitary irradiation, or with a slightly lower dose of intracavitary irradiation and the same external beam pelvic irradiation followed by an extrafascial hysterectomy. The 3-year disease-free survival and overall survival rates were 79% and 83%, respectively, and were virtually identical in the irradiation-alone and the combined irradiation and surgery groups. The incidence of progression was somewhat higher in the irradiation-alone group (46%) compared to the combined therapy group (37%) (p = 0.07). However, it appears that surgery does not contribute to increased survival compared to RT alone in patients with “bulky” stage IB disease. Furthermore, combined modality therapy was associated with a higher incidence of any reported adverse effects compared to RT alone (63% vs. 56%).
Stages IIB, IIIB, and IVA
Most patients in the United States with stage IIB disease are treated with curative-intent chemoradiation. With RT alone, the 5-year survival rate has historically been 60% to 65%, and the pelvic failure rate 18% to 39%. Similarly, most patients with stage III and IVA tumors are best treated with concurrent chemoradiation. Based on multiple randomized clinical trials, concurrent chemotherapy with irradiation is considered the standard of care. Although the studies used a variety of agents, the de facto standard has become once weekly cisplatin at a dose of 40 mg/m2 for six cycles. Other chemotherapy agents used successfully include 5-FU, mitomycin, carboplatin, paclitaxel, and epirubicin. Considering all eligible patients with stage IIB to IVA carcinomas enrolled in GOG-85, a 55% survival rate with platinum-based chemotherapy with RT was demonstrated after a median follow-up of 8.7 years. In this same group of patients, GOG-120 found a 66% survival rate with platinum-based chemoradiation. More recently, an international phase III randomized trial investigated whether the addition of concurrent and two additional cycles of adjuvant gemcitabine to cisplatin-based irradiation could further enhance clinical outcomes in stage IIB to IVA disease. At 3-year follow-up, progression-free and overall survival was higher in the gemcitabine arm compared to the standard regimen of cisplatin-based chemoradiation. This study, however, has been criticized for its statistical design and the paucity of late toxicity follow-up data.
The value of adjuvant chemotherapy following cisplatin-based chemoradiation in locally advanced cervical cancer patients is currently being explored in the OUTBACK study. This prospective, randomized, phase III trial endorsed by the GOG and RTOG randomizes patient to adjuvant carboplatin and paclitaxel or no additional therapy following primary cisplatin-based chemoradiation. The primary outcome to be addressed in this trial is improvement in overall survival.
External Irradiation Alone
Rarely, brachytherapy procedures cannot be performed because of medical reasons or unusual anatomic configuration of the pelvis or the tumor (e.g., extensive lesion and inability to identify the cervical canal, presence of a fistula). These patients may be treated with higher doses of external irradiation alone, although the results are inferior to those obtained with combined external beam and intracavitary irradiation.
UNUSUAL CLINICAL SITUATIONS
Invasive Carcinoma Treated by Simple Hysterectomy
Although uncommon, simple hysterectomy for an unrecognized invasive cervical cancer can occur in patients operated on for what is felt to be CIS, “microinvasive” disease, incorrectly diagnosed endometrial carcinoma, or for “benign” indications. If only microinvasive carcinoma is found, with no evidence of LVSI, no additional therapy is necessary. However, in patients with more advanced disease, simple extrafascial abdominal hysterectomy is not curative because the paravaginal/paracervical soft tissue, vaginal cuff, and pelvic lymph nodes are not removed.
While technically difficult, an adequate radical operation after previous simple hysterectomy may be appropriate for selected patients. Another approach favored by some is the use of adjuvant pelvic RT in patients with invasive disease of severity greater than microinvasive. In an exhaustive review of the literature comparing series of patients having reoperation with radical parametrectomy and LND versus those having postoperative RT, the weighted average 5-year survivals favored RT (68.7% vs. 49.2%).
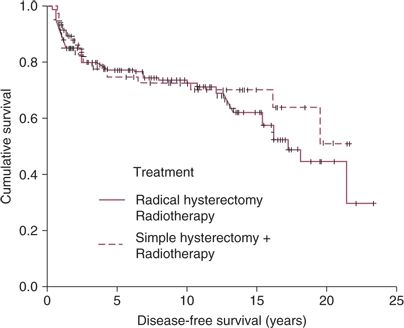
If the postoperative RT approach is chosen, postoperative irradiation should be administered immediately after recovery from operation, as prognosis is much worse if therapy is delayed. The potential contribution of concurrent platinum-based chemotherapy must be considered, particularly in view of the randomized study of patients treated after RH with high-risk features (Fig. 7.2).