4 | The Practice of Acupuncture in Obstetrics and Gynecology |
The advantage of acupuncture as a regulation therapy is its ability to treat functional disorders without causing many side effects, thus filling a vacuum in conventional medical care.
In the West, it used to be common practice to use acupuncture in pregnancy, birth, and delivery primarily due to its analgesic and mentally/emotionally relaxing properties. Acupuncture has more to offer than mere analgesics, particularly in regard to easing the process of giving birth. A shift in views was initiated through the renaissance of the ideal of a natural, gentle, and family-oriented form of obstetrics. Acupuncture, as a regulating treatment mode, complements conventional medicine, without forsaking the safety of modern obstetrics. Pregnant women are looking for safe, natural alternatives to the effective and sometimes risky methods of modern obstetrics. Acupuncture may be such an alternative. The basis of acupuncture is to stimulate the body’s own healing forces; it aids women and the babies through labor without interfering in their relationship. Acupuncture is an ideal therapy form for midwives because they consider themselves guides of the women. If supplied with the proper information, pregnant women are rather open to this treatment mode.
Today, several thousand midwives in Germany possess, in varying degrees, extensive knowledge about obstetric acupuncture.
Obstetrics
 List of Indications
List of Indications
Table 25 lists the obstetric indications for acupuncture as acknowledged in the West. Table 26 displays typical indications considered in the People’s Republic of China.
Table 25 List of proven indications for obstetric acupuncture
I. Indications during pregnancy – Hyperemesis gravidarum – Mild forms of EPH gestosis (hypertension/edema due to pregnancy) – Premature labor – Pain of various origins (lumbago, carpal tunnel syndrome, etc.) – Treatment of addictions during pregnancy – Influence on pathological positions of the fetus – Mental/emotional regulation – Birth preparation/induction |
II. Indications during delivery – Facilitation of a delivery without complications – Alleviation of pain, relaxation – Protracted birth due to functional causes (cervical dystocia and dysfunctional labor) – Placental detachment disorders |
III. Indications during childbed and nursing – Various pain conditions (e. g., episiotomy, after-pains, soreness) – Problems related to nursing (painful onset of lactation, galactostasis, early mastitis, lack of lactation) – Delayed uterine involution – Constipation – Urination disorders – Mental/emotional complaints during childbed (depression, insomnia) |
Table 26 Important obstetric TCM indications in China
First trimester • Hyperemesis gravidarum • Bleeding during the early stage of pregnancy, imminent abortion • Fever during the first trimester (only supportive) • Various disorders (edema, hypertension, hypotension, lung, liver, skin, and kidney disorders, etc.; generally only supportive) • Endocrine disorders (diabetes mellitus, thyroid disorders; only supportive) • Mental/emotional, psychiatric, and neurological disorders (supportive)
|
Second trimester • Bleeding, imminent abortion • Premature labor (only supportive) • Cervical incompetence (only supportive) • Colitis, cervicitis, amnionitis (only supportive) • Fever (only supportive) • Edema • Various disorders (hypertension, hypotension, lung, liver, skin, and kidney disorders, etc., generally only supportive) • Endocrine disorders (diabetes mellitus, thyroid disorders, only supportive) • Mental/emotional, psychiatric, and neurological disorders (supportive)
|
Third trimester/birth • Risk of premature delivery (premature labor, cervical incompetence, colpitis, cervicitis, amnionitis, placental insufficiency, etc.; only supportive) • Premature rupture of fetal membranes • Birth preparation and induction • Pain therapy before, during, and after childbirth (by itself or supportive) • Anesthesia (by itself or supportive)
|
Pregnancy
 General Regulation Based on Mental/Emotional Balance
General Regulation Based on Mental/Emotional Balance
Pregnancy and birth may put mental/emotional stress on a pregnant woman. Many pregnant women suffer from restlessness, anxiety, and sleep disorders. According to Chinese philosophy, mental/ emotional exhaustion and overstrain consume and damage the spirit (shen). Acupuncture can promote mental/emotional balance and comfortable sense of relaxation. The suitable acupuncture points are also indicated in all disease pictures that require mentally/emotionally balancing effects, for example, hyperemesis gravidarum, early labor, or for relaxation during birth.
Main points: First category
 • GV-20 • (extra point si shen cong) • HT-7 • PC-6 • KI-3
• GV-20 • (extra point si shen cong) • HT-7 • PC-6 • KI-3
Further Recommended Acupuncture Points
GV-14
HT-3
PC-7
KI-6
BL-23,
BL-62
LR-3
GB-34
SI-3
LU-7
ST-36
SP-4,
SP-6
CV-4,
CV-6,
CV-15
Ear point: 55 shen men
Tip
According to TCM teachings, restlessness, anxiety, and mental/emotional imbalance are caused by qi disorders in the water and fire elements. A vacuity condition in the water element leads to a loss of control over the fire element, which causes restlessness of shen (spirit). The kidneys have to be strengthened through moxibustion of KI-3—a tonifying technique.
Duration of session: 20 minutes. Daily, initially; after the onset of therapeutic success, taper off frequency of therapy sessions.
Sleep Disorders
In the case of sleep disorders, the points for general mental/emotional regulation are typically used. Particularly well-established points are:
Main points: First category
 • GV-20 • KI-6 • BL-62
• GV-20 • KI-6 • BL-62
Further Recommended Acupuncture Points
HT-7, PC-6, ST-36
BL-23
The points may be needled daily, one hour before going to bed, for 20 minutes. Taper off daily treatments according to treatment success.
| Nutritional recommendation: See page 200 |
Anxiety and Tension
Anxiety is associated with the water phase, which puts emphasis on points of the kidney and bladder channels. Tension (particularly if muscles are involved) is associated with the wood phase, which emphasizes LR-3 and GB-34. An important principal point is GV-20.
Main points: First category
 • GV-20 • KI-3 • LR-3 • GB-34
• GV-20 • KI-3 • LR-3 • GB-34
Further Recommended Acupuncture Points
HT-7, PC-6
BL-67
Duration and frequency of treatment: see the “Tip” box.
 Hyperemesis Gravidarum
Hyperemesis Gravidarum
Emesis gravidarum occurs frequently; approximately two-thirds of all pregnant women complain of nausea and vomiting of varying severity during the first 12–16 weeks of pregnancy. Hormonal changes, an increase in metabolic activity, introduction of trophoblastic tissue into the female system, and added mental/emotional stress are presumed to be the causes. In less severe cases, nutritional changes are recommended (more frequent, smaller meals, supplements, primarily vitamin B complex). If the pregnant woman loses weight due to vomiting this is defined as hyperemesis.
In the Traditional Chinese Medicine (TCM) view, hyperemesis is a weakness of the middle (stomach and spleen). In TCM, the middle is regarded as the place of assimilation of spiritual and physical nutrition. If this assimilation capacity is inadequate counterflow qi (rebellious qi), which causes nausea and vomiting, occurs. TCM recommendations for patients:
• Rest, avoid stress and aggravation
• Drink a cup of warm tea before getting out of bed
• Eat small amounts several times in the course of the day
• Rub fresh ginger roots on the tongue before eating or taking medication.
Regarding nutrition, the pregnant woman should consider the following:
• Do not eat or drink anything cold
• Do not drink coffee, no sour, spicy or fatty foods
• Drink warm water, warm beverages made of ginger and coriander, fennel or green tea
• Eat soft foods, especially rice, chicken, and noodle soup, mashed potatoes, and stewed vegetables (carrots and potatoes strengthen the middle).
The patient must be hospitalized in severe cases of hyperemesis gravidarum: no food and fluid intake, acidosis, vitamin B vacuity, muscle weakness, increased bilirubin count, and increasing dehydration.
The success rate of acupuncture in cases of hyperemesis gravidarum is considerable. An attempt to apply this treatment form should always be made. Within a short period of time, complaints can diminish or even completely disappear.
The injection of vitamin B1 at the ear point 55 shen men also has shown good results.
Main point: First category
 • PC-6
• PC-6
Further Recommended Acupuncture Points
GV-20
HT-7
CV-12, CV-15, CV-17
ST-36
LR-3
SP-9
Ear points: 22 endocrine system, 55 shen men
Tip
Initially, treat the main point of the first category (PC-6) daily. If the disorder is connected with considerable mental/emotional aspects, add the point GV-20.
Duration of treatment: 20 minutes, technique: tonifying at point PC-6.
Before the first session, the pregnant patient should be informed of the possibility of an initial aggravation of the condition. Should this occur (indicating a positive reaction of the body), the therapy needs to be continued! An improvement of the condition can generally be expected after a few sessions. Once the therapy shows signs of success, taper off the sessions.
Chinese herbal therapy: Fresh ginger and coriander tea is recommended.
Simmer 10 g coriander and 6 g fresh ginger root in 1 L of water for 15–20 minutes. Drink this tea at lukewarm temperature throughout the day.
Also:
| Nutritional recommendation: See page 209 |
 Heartburn and Vomiting
Heartburn and Vomiting
TCM distinguishes between nausea and the vomiting and heartburn which occur frequently during the last trimester.
Nausea is considered the reversal of the flow of qi (the regular direction of nutritive qi is from top to bottom). Heartburn and vomiting are repletion conditions that need to be calmed and drained.
• Nausea = qi stagnation (first stage)
• Heartburn = counterflow qi (second stage)
• Vomiting = severe counterflow qi (third stage).
Main point: First category
 • ST-36 (European master point for heartburn and vomiting)
• ST-36 (European master point for heartburn and vomiting)
Further Recommended Acupuncture Points
ST-44
CV-12, CV-15, CV-17
PC-6
GV-20
Ear points: 87 stomach, 55 shen men
Tip
PC-6 is the master point for nausea. ST-36 is the master point for vomiting and heartburn.
Vomiting and heartburn are repletion conditions that are treated through carefully sedating, better yet “neutral” techniques at ST-36.
Heartburn is treated daily (duration of treatment: 20 minutes) until an improvement of the condition takes place after a few sessions. The treatment frequency tapers off afterward.
In the case of acute vomiting, treatment needs to take place once or twice a day. Afterward, the treatment follows the same approach as for heartburn. Pregnant women who undergo acupuncture therapy in preparation for birth (see p. 97) suffer less frequently from heartburn because ST-36 is part of this therapy program. If the weekly therapy sessions for childbirth preparation are insufficient to alleviate the heartburn, one or two sessions treating only ST-36 have to be added.
 Early Labor and Impending Premature Delivery
Early Labor and Impending Premature Delivery
Early labor can be caused by various reasons. General causes include physical and mental/emotional exhaustion, infection, retardation, and placental insufficiency. Multiple pregnancy, hydramnios, and cervical tears can be additional causes. Approximately 70% of early labor cases are due to infections, placental insufficiency, or retardation of the child. In these cases, acupuncture may support conventional medicine. In other cases, acupuncture can be the sole therapy form and frequently replaces oral tocolysis.
The intravenous administration of tocolytic substances has physical and mental/emotional side effects. Physical symptoms can generally be counteracted with medications such as beta-blockers, and seem to decrease during the course of the therapy. Mental/emotional symptoms in long-term patients, on the other hand, are of serious consequence. These concomitant psychological complaints are reason enough to try acupuncture therapy. With acupuncture as a supporting therapy, fewer tocolytic side effects appear. Improvement of the following conditions can be expected: Hot flushes, tremor, constriction of the chest, irritability, headache, and pelvic complaints. The nonspecific sensation of pressure on the pelvic floor, which is frequently reported by pregnant women, is likely to decrease after only a few acupuncture sessions because of the relation of the du mai channel to the pelvic floor. Patients also seem to benefit from the sedating and uplifting effects of acupuncture therapy due to endorphin secretion. The homeostatic effect is beneficial for this indication.
Main point: First category
 • GV-20
• GV-20
Further Recommended Acupuncture Points
HT-3, HT-7
PC-6
ST-36
GB-34
LR-3
SP-6
Ear points: 55 shen men, 51 autonomic nervous system
Tip
Before initiating acupuncture, establish the cause of early labor activity thoroughly using conventional medicine diagnostics.
Duration of session: 20 minutes, initially once per day.
Treatment frequency can taper off once improvement sets in, usually after a few sessions.
Acupuncture treatment of early labor has to be closely monitored.
| Nutritional recommendation: See page 211 |
 Infections During Pregnancy
Infections During Pregnancy
In all cases of infection during pregnancy, acupuncture is merely a complementary form of treatment that may only follow a thorough differential diagnosis by a conventional medical practitioner! The immunostimulating effects of acupuncture are useful in cases of infection and fever. Acupuncture acts in a balancing, calming, and fever-reducing way. This may at times replace the use of medications.
Main points: First category
 • LI-4 • LI-11
• LI-4 • LI-11
Further Recommended Acupuncture Points
GV-14
ST-36
Tip
During the acute phase of an infection, acupuncture treatment is given once or twice daily.
Duration of session: 20 minutes.
In the case of fever: Use “sedating” techniques carefully, better yet, use “neutral” techniques. Close supervision!
 Treatment of Addictions During Pregnancy
Treatment of Addictions During Pregnancy
Giving pregnant women with addictions acupuncture treatment provides an additional therapy option in obstetrics. Acupuncture has been proved to be an effective means for treating pregnant women with addictions: It alleviates withdrawal symptoms, reduces the desire for drugs, and improves physical and mental/emotional well-being. In half of the cases of pregnant women with addictions, acupuncture can help the newborns to avoid withdrawal symptoms, hospitalization, and drug therapy. Following the so-called NADA protocol (National Acupuncture Detoxification Association), acupuncture acts independently of substances, which makes it suitable for all forms of dependency.
In the case of nicotine withdrawal symptoms, various body acupuncture points are indicated. In spite of good intentions, many women are unable to quit smoking on their own; if sufficiently motivated, they can reach this goal with the aid of acupuncture. Acupuncture produces reactions ranging from a decreased desire to smoke a cigarette to a strong aversion to smelling the smoke. Pregnant women often perceive this change as an internal changeover process, which is supported by their own willpower. The pregnant woman has to be alerted to the fact that acupuncture by itself without personal willpower will not cause abandonment of the addictive substance.
More than 600 institutions in the United States and more than 400 institutions worldwide follow the NADA concept that was developed in 1975 by the American physician and psychiatrist M. Smith. Today, there is no doubt about the effectiveness of acupuncture in the context of addictions and drug rehabilitation.
Through acupuncture in cases of addiction, many pregnant women experience a decrease in autonomic withdrawal symptoms (perspiration, inner restlessness, anxiety), cravings as their feelings clear up. Even particularly nervous pregnant women report an increase in physical balance, and improved, refreshing sleep. In addition, there is a decrease in typical complaints during pregnancy, such as nausea and heartburn. Patients report considerable improvement of general well-being.
Main points: First category
 NADA protocol: (Ear points: 55 shen men, 51 autonomic nervous system, 95 kidneys, 97 liver, 101 lungs)
NADA protocol: (Ear points: 55 shen men, 51 autonomic nervous system, 95 kidneys, 97 liver, 101 lungs)
 • GV-20 • PC-6 • HT-7 • LI-4 • ST-36
• GV-20 • PC-6 • HT-7 • LI-4 • ST-36
Further Recommended Acupuncture Points
CV-12, CV-14, CV-17
LU-9
LR-3
SP-6
Tip
Drug rehabilitation
According to the NADA protocol, drug rehabilitation treatment initially takes place on a daily basis.
Duration of session: 30 minutes.
After approximately two to three weeks, slowly taper off therapy sessions. Attending a support group is recommended.
Tip
Nicotine addiction
The following approach has proved successful for treating nicotine addiction: The pregnant woman must stop smoking for five to seven days. After this period, the body’s biochemical adaptation to the nicotine withdrawal begins. Only at this point should acupuncture therapy be started! If the acupuncture begins simultaneously with the smoking cessation, many patients believe that the needle by itself will eliminate the addiction and applying one’s own will power is not necessary. With the “delayed” approach, the success rate is clearly higher and the relapse rate is lower.
During the initial week, treatment takes place daily.
Duration of session: 20 minutes.
After the first week, taper off sessions.
 Breech Presentation
Breech Presentation
Approximately 5% of all infants are born in breech presentation. There is no simple, undisputedly effective, and at the same time risk-free, method for prenatal version from the breech presentation. External cephalic version involves the risk of umbilical cord complications, premature detachment of the placenta, and acute intrauterine asphyxia, and should therefore only be performed if preparations for an emergency cesarean section have been made. There ist a percentage of babies who will undergo a spontaneous reversion to a breech presentation following successful version. Vaginal birth with breech presentation is considered too risky by many obstetricians, particularly in the case of a first-born. As a consequence, in Germany, the cesarean rate for first-borns in breech presentation is rather high. The mother carries an increased morbidity risk.
Alternative methods for this condition have been presented for many years. The “Indian bridge” and moxibustion at acupuncture point BL-67 are frequently used. Chinese medicine reports a success rate of over 90%. The rate of spontaneous versions from breech presentation into a cephalic position has not been extensively researched. This rate decreases considerably in the course of the pregnancy. Between the 36th and 40th weeks it is clearly lower than between the 32nd and 35th weeks. In the case of primipars, the chance of a baby in breech presentation undergoing spontaneous version into cephalic position is only 25% after the 33rd week. This chance decreases to 6% after the 37th week. For multipars, the rate is usually higher (Table 27).
Table 27 Rate of spontaneous version in breech presentation
First child | Second child | |
|---|---|---|
After the 33rd week of pregnancy | ≤25% | ≤54% |
After the 37th week of pregnancy | ≤6% | ≤15% |
A research study carried out by the Gynecological University Hospital in Mannheim, Germany, showed an increase of spontaneous version through moxibustion of acupuncture point BL-67 by up to 50.4%. Premature rupture of fetal membranes, pathological CTG (cardiotocography) patterns, and other complications did not occur with this treatment. When comparing test groups, the beginning of the treatment, the fetal weight, the amount of amniotic fluid, and the placenta location had no effect on the frequency of version.
Approximately 80% of the pregnant test persons reported increased motion of the baby, which generally started during the moxibustion treatment and continued up to several hours (24 hours is the longest reported duration) after the completion of the treatment.
Contrary to the external version, this method is risk-free because it does not produce umbilical cord complications. In the case of a collision with the umbilical cord, the baby returns to the initial position.
In China, the high success rate documented in the literature can be explained by the early treatment onset (29th to 30th week).
Caution: In the case of early labor, moxa therapy is absolutely contraindicated because it can cause an acceleration of the premature labor!
Main point: First category
 • BL-67 (moxibustion)
• BL-67 (moxibustion)
Tip
Moxibustion of acupuncture point BL-67 (tonifying point of the BL-channel, water phase → uterus) is superior to needle acupuncture by itself. Therapy plan:
• Start of therapy: Not before the 33rd week.
• End of therapy: Caution: at the latest by the end of the 36th week, no moxa treatment of BL-67 after that time!
• Four treatment sessions are sufficient.
• Time between treatments: Two days.
• Duration of treatment: 20 minutes per session (10 minutes right side, 10 minutes left side, or 20 minutes alternating sides).
• Position: Knee-elbow position; no “Indian bridge”—it is not liked by pregnant women—it is less effective!
• Caution: Do not use in the case of early labor—due to the risk of accelerating labor!
• Do not perform in the case of high-risk pregnancies.
Increasing the recommended number of four treatment sessions will not improve therapy results.
The pregnant women have to be informed that increased fetal movement for up to 24 hours after the treatment is to be expected. This is a positive sign and not an indication that the baby is in danger. The allegation that moxibustion causes early labor activity, premature rupture of fetal membranes, and pathological CTG patterns (due to umbilical cord complications) has been refuted by research. If performed properly, moxibustion is risk-free. So far, complications due to moxibustion up to the 36th week have not been reported. Cases with pathological outcome are known if this technique is used immediately before delivery. This outcome might have been due to decreased amniotic fluid and increased fetal weight.
The rate of spontaneous version before the 33rd week for primipara is noted at over 70 %. Therefore, an earlier start of moxibustion does not seem suitable.
Procedure: A burning moxa cigar is carefully brought close to acupuncture point BL-67 until the pregnant woman experiences a strong sensation of warmth but not pain. The moxa cigar is withdrawn when the patient begins to experience the heat as unpleasant. After a short break, the moxa cigar is again brought close to BL-67. After this process has been repeated several times on one side (approx. 10 minutes) it is applied to the other side. This treatment may cause slight contractions that can be observed via tocography but have no effect on the dilation of the cervix. These contractions may be visible until a few hours after the treatment. After proper instruction, it is possible for the pregnant woman’s partner to perform the moxa treatment at home. It is recommended, however, that it is left to the midwife/physician to perform the treatment. This allows the therapist to monitor unusual reactions and avoids unnecessary worry by the patient.
Moxibustion is a therapeutic application and should therefore only be performed by medical professionals.
 Gestosis
Gestosis
Acupuncture can be very effective when treating mild forms of EPH gestosis (pre-eclampsia) or pregnancy-induced hypertension. At the same time, established treatment forms should not be neglected. Mother and child have to be carefully monitored for placental insufficiency or worsening of the gestosis and their harmful consequences. The use of acupuncture focuses on the treatment of edemas and hypertension.
Treatment of Edemas
Main points: First category
 • ST-36 • SP-6
• ST-36 • SP-6
Further Recommended Acupuncture Points
SP-4, SP-9
LU-7
LI-4, LI-11
CV-12
BL-23
KI-3, KI-6
| Nutritional recommendation: See page 206 |
Hypertention
Main point: First category
 • LR-3
• LR-3
Further Recommended Acupuncture Points
PC-6
HT-7
LU-9
ST-36
SP-6
GV-20
Ear points: 55 shen men, 100 heart, 59 hypertension, 105 blood pressure-reducing groove
Tip
For the treatment of gestosis, acupuncture is only indicated as a supportive therapy. In mild gestosis cases, acupuncture can be used to achieve remarkable results in lowering blood pressure and reducing edemas. Hypertension and edemas are initially treated once a day for 20 minutes. If the therapy is successful, treatment is slowly tapered off.
 Pain Conditions During Pregnancy
Pain Conditions During Pregnancy
Pain is one of the main indications for acupuncture treatment. Due to its strong analgesic effects and complete lack of side effects, acupuncture is useful in all pain conditions during pregnancy. Thoroughly probing the complaints is always a must. It needs to be remembered, however, that the common forceful manipulation of points that act on the uterus (especially locally acting points of the sacrolumbar area), and are generally used in the case of pain (repletion condition), has to be omitted (a contraindicated technique during pregnancy!). Previous experience has shown that neutral needle stimulation is sufficient to alleviate the complaints.
Main points: First category
 • LI-4 • LI-10 • Local points
• LI-4 • LI-10 • Local points
General Pain Points
GV-20
ST-36,
ST-44
SP-6
Extra points: nei ma, wai ma
A-shi points
Tip
Initially, daily treatment for 20 minutes. After the treatment shows success, taper off treatment. Generally, only a few sessions are required.
Do not stimulate forcefully (contraindicated during pregnancy), not even in the case of typical repletion conditions!
Use a neutral technique!
Back Pain (Sciatic Back Pain)
This is an established indication that excludes nearly all drug therapies during pregnancy. TCM differentiates two forms of sciatic pain, namely bladder channel ischialgia (bladder sciatica) and gallbladder channel ischialgia (gallbladder sciatica).
Further Recommended Acupuncture Points
Bladder sciatica:
— Local points: BL-23-BL-32
— Distal points: BL-36, BL-40 (BL-54 Bi), BL-60, BL-62
Gallbladder sciatica:
— Local points: BL-23-BL-32
— Distal points: GB-30, GB-34, GB-41, LR-3
General points: LI-4, SI-3, KI-3, KI-6, ST-36, SP-6, GV-3, GV-4, GV-14, GV-20 (ascending)
Ear points: 54 lumbago, 55 shen men
Tip
Initially, daily needle treatment for 20 minutes.
Duration of session: 20 minutes.
After onset of therapeutic success, taper off treatment. Generally, only a few sessions are necessary. Do not stimulate forcefully (contraindicated during pregnancy), not even in the case of repletion conditions!
Use a neutral technique!
| Nutritional recommendation: See page 203 |
Headache and Migraine
Headache and migraine are some of the best indications for acupuncture. The selection of points depends on the exact assessment of the headache. Selection depends on the location of pain, affected channels, and modalities. Therapy can only be successful under consideration of these specifications. Local and distal points of the affected channel have to be combined.
TCM lists several headache patterns including stomach, gallbladder, liver, and bladder channel headaches (migraines). According to the traditional concept, headache and migraine are caused by a superficial blockage of qi in the yang channels of the head. After proper channel diagnosis, pressure-sensitive points and affected pain areas are located by palpation. Needling takes place along the channel pathway. Use needles sparingly! Select only important points!
Further Recommended Acupuncture Points
GV-14, GV-20
SI-3
LU-7, PC-6
LI-4 (LI-11)
ST-36, ST-44
SP-6
GB-14, GB-20, GB-21, GB-34, GB-41
LR-2, LR-3
BL-2, BL-10, BL-23, BL-60, BL-62, BL-67
KI-3, KI-6
Extra points: tai yang, yin tang, si shen cong
Tip
Especially for the diagnosis of headache (migraine), the selection of the proper acupuncture points depends entirely on the examination of the individual, specific symptoms, and on palpation.
Acute headaches that have started recently. Initially, daily treatment.
Duration of session: 20 minutes.
After onset of therapeutic success, taper off treatment.
Chronic headaches that have persisted over a longer period of time: One to two therapy sessions per week, over a longer period of time (10–12 weeks). Individual treatment following TCM rules is required!
Duration of session: 20 minutes. Treatment is interrupted after 10–12 sessions and repeated if necessary.
| Nutritional recommendation: See page 209 |
Carpal Tunnel Syndrome
Due to water retention in the carpal tunnel caused by hormones, the tissue pressure on the median nerve may increase toward the end of the pregnancy, and carpal tunnel syndrome may occur. The symptoms are numbness, decreased sense of touch, and pain. This syndrome is almost always resistant to conventional treatment. Acupuncture, however, has a high success rate within a short period of time. The complaints can be eliminated or considerably alleviated after only a few sessions.
Chinese pattern: Spleen qi vacuity with dampness.
Main points: First category
 • PC-6
• PC-6
Further Recommended Acupuncture Points
PC-7
LI-4
Tip
Before the first treatment session, the pregnant woman has to be informed of the possibility of an initial worsening of symptoms (probability of < 15%, no reason to terminate the treatment, as this is a sign of the effectiveness of the treatment). Initially, daily treatment is required.
Duration of session: 20 minutes.
In severe cases, cautiously applying electrostimulation at PC-6 and PC-7, or PC-6 and LI-4 (one side at a time, do not cross the heart axis) is recommended. Generally, the pregnant woman can get relief from the symptoms if only PC-6 is needled for a few days.
| Nutritional recommendation: See page 203 |
 Childbirth Preparation using Römer’s Scheme (Mannheim Model)
Childbirth Preparation using Römer’s Scheme (Mannheim Model)
Morphological Birth Preparation
The length of labor is decreased through birth preparation with acupuncture. Previously common models have focused on the “mentally/emotionally balancing” and pain-reducing effects of acupuncture (e. g., the points GV-20, PC-6, HT-7, and LI-4). Research including 1000 pregnant women conducted by the Gynecological University Hospital in Mannheim proved that acupuncture birth preparation decreases the length of labor because of improved cervical ripening. Thus, it is called “morphological acupuncture” (Fig. 34a–c).
In normal pregnancy, weekly acupuncture treatment using points which, according to Chinese medical theory, facilitate labor, should begin in the 36th week and continue up to the time of delivery.
In a study we conducted, the test group was treated with the above-mentioned “mentally/emotionally balancing” birth preparation model weekly, beginning at the 36th week.
All acupuncture points that were selected were needled using tonifying techniques. The duration of each session was 20 minutes. At the beginning and at the end of the treatment series, all pregnant women were examined. The specifying parameters were:
• Length of labor beginning with labor activity that affects the cervix
• Relative change in the Bishop score
• Vaginal ultrasound showing changes in cervical length
• Vaginal ultrasound of the funnel formation (definition of funnel: opening of the isthmus of the uterus > 0.5 cm).
Indications for a primary section, such as placenta previa, cephalopelvic disproportion, breech presentation in cases of primipara (without spontaneous vaginal delivery), and known bleeding disorders of the mother, are contraindications for the acupuncture therapy. The control group included pregnant women who had not received acupuncture treatment and delivered during the time of the study in the clinic.
The median length of labor in women with morphological acupuncture treatment (experimental group) was 470 minutes, while in women with mentally/emotionally balancing acupuncture (control group) it was 536 minutes, and in women who were not treated with acupuncture (comparative group) it was 594 minutes. This shows that the length of labor was two hours shorter if the pregnant woman was treated with morphological acupuncture therapy, and one hour shorter if she was treated with the mentally/emotionally balancing model. The relative Bishop score shows a significantly increased cervical ripening with 5.9 points for the experimental group, 4.0 points for the control group, and only 3.6 points for the comparative group. The differences in cervical length corresponded in the same way: experimental group 15.9 mm, control group 9.8 mm, untreated comparative group 8.9 mm. In addition, the morphological acupuncture therapy produced a significant funnel formation in the area of the isthmus of the uterus, which had not been detected before (experimental group 82%, control group 30%, comparative group 29%). The cesarean section rate was considerably reduced in the group treated with morphological acupuncture.
These results confirm the effectiveness of acupuncture birth preparation. The mechanisms which affect the cervix have not yet been established. Three factors seem to play an important part: The catabolism of collagen molecules, the activation of catabolic enzymes that degrade collagen, and the disintegration of collagen bundles. Before the onset of labor, the cervix softens through the buildup of fluid; the original holding function is relinquished and the process of opening for the delivery begins.
A further effect of the morphological acupuncture model was a significant improvement in contraction coordination. Secondary uterine inertia, dysfunctional labor, and the need for oxytocics, such as intravenous oxytocin drip infusion, were 61% lower than in the control and comparative group.
There was no significant difference between groups in regard to the time of labor onset and the total number of prolonged gestations. The acupuncture therapy neither induced early delivery nor reduced the number of prolonged gestations. This shows, contrary to common belief, that the acupuncture effects that shorten the length of labor begin only after the onset of natural delivery-inducing mechanisms, and that the ripening of the cervix is not a factor which influences delivery induction. The ripening process of the cervix and the time of delivery onset that is naturally induced by the body are two separate parameters that have no reciprocal relationship and which can be individually affected.
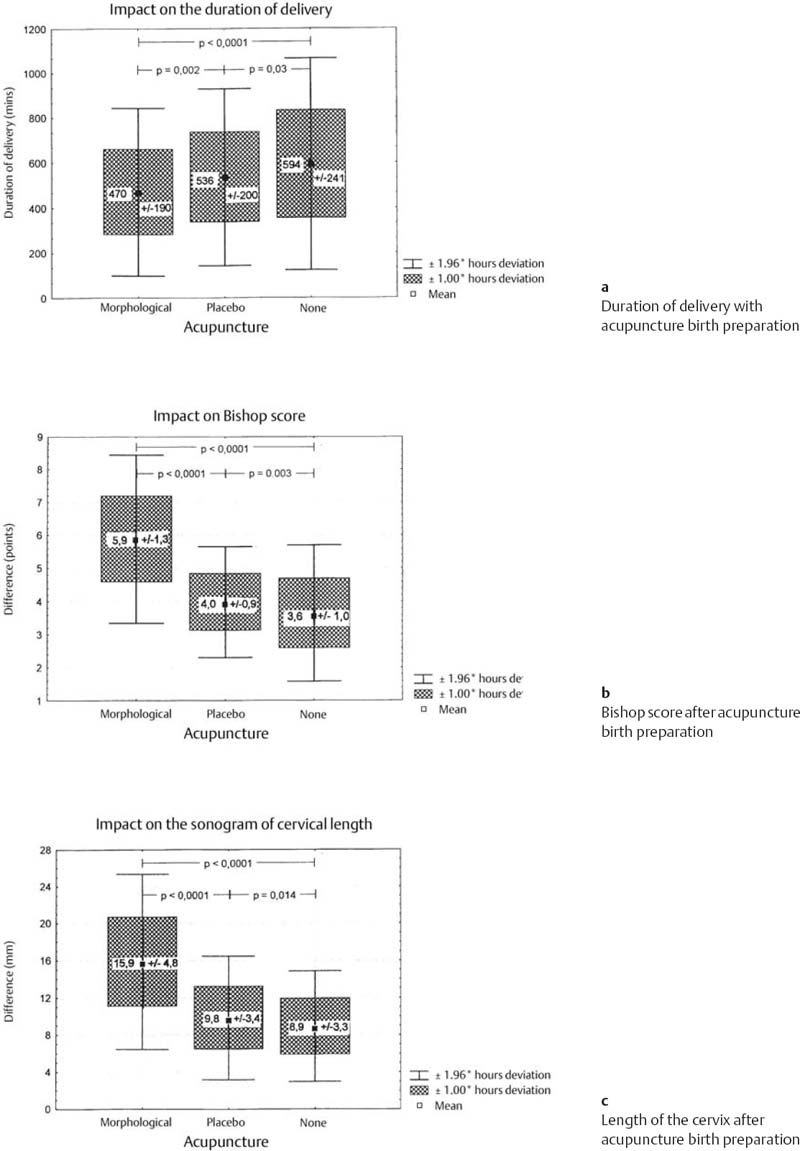
Fig. 34a–c Morphological acupuncture
According to present research results, morphological acupuncture therapy is a well-accepted, riskfree, and evidently an effective form of birth preparation. In the case of pregnancies without complications, morphological acupuncture should be recommended to all pregnant women as a complementary treatment in addition to the conventional, established forms of birth preparation.
The acupuncture birth preparation model is based on a balanced therapeutic concept (which is not immediately apparent) that corresponds to the rules of yin and yang. The points GB-34, ST-36, and BL-67 correspond to yang, and the point SP-6 corresponds to yin. This seems to constitute an imbalance of three yang points versus one yin point. SP-6, the intersection point of three yin channels on the leg, represents three yin channels (spleen, liver, kidney), and provides a balanced yin-yang relation.
The point GB-34, the meeting point for the muscles (affects the uterus muscles), is crucial in achieving results.
BL-67 is the tonification point of the bladder channel that belongs to the water phase. The uterus is associated with the water phase, and BL-67 has a strong effect on the urogenital area (and the uterus), and promotes labor.
Tip
This therapy model is indicated for all pregnant women without pregnancy complications. Before the first session, the pregnant woman needs to be informed that she might experience increased fetal movement during and after the session, which is a response to the acupuncture treatment and a positive sign.
Pregnant women should discuss in a detailed consultation with their midwife which forms of birth preparation are particularly beneficial to them. It does not necessarily improve the course of a delivery if a pregnant woman chooses several forms of birth preparation at once.
Note: Birth preparation through acupuncture causes a much shorter period of dilation due to a favorable ripening of the cervix. The following stage of expulsion appears prolonged in comparison, even though it is of normal duration. This relative prolongation has to be recognized as such to avoid unnecessary intervention (if otherwise medically not required) in the natural course of delivery, and, if necessary, use supplementary means to stimulate contractions.
Generally, after the use of acupuncture birth preparation, the results of cervical examination of primiparae are more likely to be similar to the examination results of multiparae. A high rate of primiparae arrives at the hospital with a cervix that has dilated several centimeters, and without having increased or painful labor activity.
Peripartal
 Induction of Labor
Induction of Labor
The effects of acupuncture with regard to the induction of labor reveal the physiological and regulating aspect of acupuncture therapy. Acupuncture cannot produce any effects that the body could not produce or regulate naturally! Accordingly, acupuncture is only effective for the induction of labor if a general labor readiness is present (detectable by tocograph) that has not yet led to cervix dilation.
Acupuncture can increase a latent readiness for labor that has not yet produced the desired onset of labor, and it can lead to a regular first stage of labor. If there are no signs that indicate uterine contractions (e. g., when labor decreases instantly after an oxytocin sensitivity test), acupuncture is expected to only be mildly effective or not effective at all.
Acupuncture can always be justified, by itself or as a complement to other treatments, even in the abscence of signs of readiness for labor, as in the case of premature rupture of membranes without contractions.
Acupuncture points LI-4, and BL-67 are considered important points for stimulating a latent readiness for labor into true labor. The effectiveness of LI-4 is partly due to its regulation of intestinal activity, similar to the action of enemas. According to the Chinese organ theory, the uterus corresponds to the water phase (see also the effects of BL-67 with respect to version for breech presentation and during birth preparation). Increased uterine contractions can be observed through the application of moxibustion to achieve a version for breech presentation. In the 33rd to 36th weeks, this does not act on the cervix nor does it induce labor. On the due date, the natural uterine contractions are increased to the point that they allow acupuncture to promote labor.
Main points: First category
 • LI-4 • BL-67 • SP-6 • (GB-34)
• LI-4 • BL-67 • SP-6 • (GB-34)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









