Fig. 7.1
Configuration of (a) the adult larynx and (b) infant larynx (Reprinted with permission from Wheeler M, Coté CJ, Todres D. The Pediatric Airway. Chapter 5. In: Coté CJ, Todres ID, Goudsouzian NG, Ryan JF (editors). A Practice of Anesthesia for Infants and Children, 3rd edition. Philadelphia, PA: W. B. Saunders Company. 2001)
Fig. 7.2
Relative effect of circumferential edema on the infant and adult airway (Reprinted with permission from Wheeler M, Coté CJ, Todres D. The Pediatric Airway. Chapter 5. In: Coté CJ, Todres ID, Goudsouzian NG, Ryan JF (editors). A Practice of Anesthesia for Infants and Children, 3rd edition. Philadelphia, PA: W. B. Saunders Company. 2001)

Fig. 7.3
Child with post-intubation subglottic stenosis (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
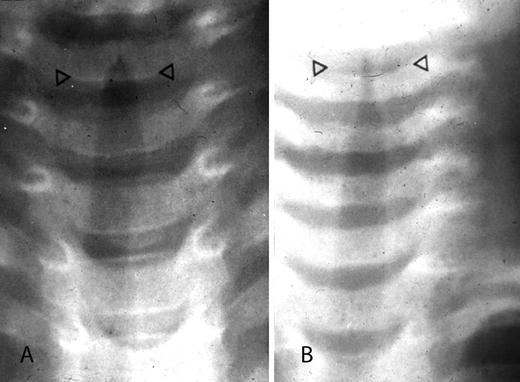
Fig. 7.4
Plain X-ray of the airway of a child with (a) severe croup and (b) mild croup. Note the subglottic narrowing and appearance of the characteristic “Chrysler Building” sign (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
The larynx of the infant and young child is higher than in the adult patient. The adult larynx is located at C6–7, whereas it is at C4 in the infant and descends to the adult location as growth occurs during childhood. The cephalad location of the infant larynx makes oral ventilation difficult, and as a result the infant is an obligate nasal breather for the first year of life [5]. The epiglottis projects vertically in the adult, but posteriorly in the infant. The infant epiglottis is also narrower and omega shaped, which makes it more prone to obstructing the laryngeal inlet [6] (Fig. 7.5). In the setting of nasal congestion, effective ventilation may be compromised in the unaltered state and worsened after sedation.
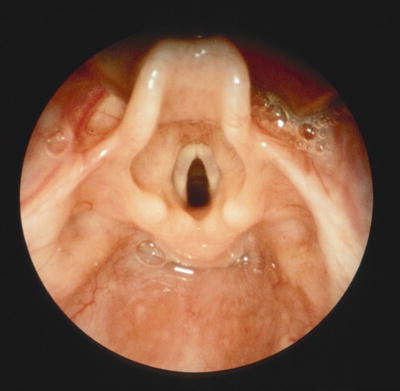
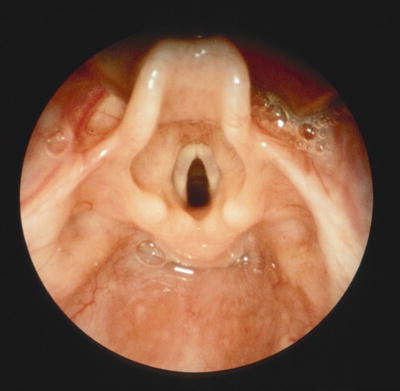
Fig. 7.5
Normal infant larynx. Note the omega-shaped epiglottis (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
The tongue of the infant is larger in relation to the oral cavity than that of the older child and adult. In neonates, the tongue is more anterior than the larynx so that the epiglottis can contact the soft palate and allow respirations and sucking simultaneously. This does, however, predispose the infant to airway obstruction more readily than the older child. At birth, the base of the tongue resides in the oral cavity and gradually descends with the larynx to a more caudad position by the fourth year of life. The ratio of soft tissue to bony structures is higher in the infant and thus predisposes this group of patients to a greater risk of mechanical oropharyngeal obstruction. The combination of small nares, large tongue, small mandible, excess soft tissue, and short neck also increases the infant’s susceptibility to airway obstruction [7]. The ribs of the infant and small child are more horizontal in orientation than those of the older child and adult, and more flexible, which therefore predisposes the child to ventilatory compromise. As previously noted, since the metabolic rate and oxygen consumption of infants is double than that of the adult and the functional residual capacity is smaller, the rapidity of desaturation in the infant and child is much greater. For this reason optimal surveillance of the airway and respiratory mechanics is essential if hypoxia is to be avoided [8].
Normal spontaneous breathing is accomplished by minimal work, and obstruction of either the upper or lower airway will result in increased work of breathing. To avoid this it is essential that airway obstruction and compromises in ventilation be recognized and corrected early. Infants and children may rapidly progress from normal breathing to obstruction, and compromised respiration to respiratory distress, and eventual cardiac arrest. Since oxygen consumption is higher in infants, decreases in oxygen delivery will result in more rapid compromise than is observed in older patient populations. The presence of apnea leading to inadequate alveolar ventilation may rapidly progress to hypoxemia, hypercarbia, and eventual tissue hypoxia.
Assessment of the Pediatric Airway for Sedation
Physical examination reveals the general condition of a patient and the degree of the airway compromise. Laboratory examination may include assessment of hemoglobin, a chest radiograph, and barium swallow, which can aid in identifying lesions that may be compressing the trachea. Other radiologic examinations such as magnetic resonance imaging (MRI) and computed tomography (CT) scan may be indicated in isolated instances but are not routinely ordered.
The physical examination of the airway in children begins with simple observation, since approaching an anxious child may cause inconsolable crying and distortion of the physical examination. Observation of the general appearance, noting color of the skin and the presence of pallor, cyanosis, rash, jaundice, unusual markings, birthmarks, and scars from previous operations should be documented.
The degree of mouth opening should be noted and full examination of the oropharyngeal area should be completed. The distance from the temporomandibular joint to the angle of the ramus is helpful in the assessment of the adequacy of the mouth opening. The distance between the angle of the ramus and the mentum is a good predictor of the ability of the mandibular bony structure to accommodate the oropharyngeal soft tissue. The presence of loose teeth should be documented. Special attention should be paid to the condition of the soft and hard palates, the dentition, and the size of the tongue. The relation of the tongue to the other oropharyngeal structures should be noted. For instance, a large thick tongue may pose minimal increased risk for airway obstruction in a child with an otherwise normal oropharynx but may cause severe risk in the child with a narrow oropharynx or a high arched palate (as may be present in children with craniofacial abnormalities and syndromes) where the tongue occupies a greater proportion of the bony structure volume. The amount of the posterior pharynx that can be visualized is important and correlates with the difficulty of intubation, and in sedated patients would correlate with the potential for airway obstruction. The Mallampati classification (Class I–IV) is based on the structures visualized with maximal mouth opening and tongue protrusion in the sitting position (Fig. 7.6) [9, 10]. The soft palate, fauces, uvula, and pillars are visualized in patients with a Class I airway. The soft palate, fauces, and portion of the uvula but no pillars are visualized in Class II. The soft palate and base of uvula are visualized in Class III and only the hard palate is visualized in Class IV [10]. Tonsil size should be evaluated since the tonsils of pediatric patients are frequently enlarged and may be the source of upper airway obstruction. A standardized system for evaluation of tonsils exists and is based on the percentage of pharyngeal area that is occupied by hypertrophied tonsils. Class 0 tonsils are completely limited to the tonsillar fossa. Class +1 tonsils take up less than 25 %, Class +2 tonsils take up between 25 and 50 %, and Class +3 tonsils take up 50–75 % of the pharyngeal area. Class +4 tonsils take up greater than 75 % of the oropharynx and are commonly referred to as “kissing tonsils” [11] (Fig. 7.7). Tonsillar hyperplasia may increase the risk of airway obstruction in the sedated patient when the tonsils occupy the oropharyngeal space outside of the tonsillar fossa as in Class +3 and Class +4 anatomy. Conversely, lesser degrees of hyperplasia as seen in Class +1 and Class +2 may result in airway obstruction in the sedated patient with craniofacial abnormalities such as Down syndrome.
Fig. 7.6
Mallampati classification of pharyngeal structures (Reprinted with permission from Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987 May;42(5):487–490)
Fig. 7.7
Classification of tonsillar hypertrophy (Reprinted with permission from Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clin North Am. 1989;36:1551–1569. WB Saunders)
Abnormal facies might be an indication of a syndrome or constellation of congenital abnormalities. One congenital anomaly often is associated with others. The neck should be examined primarily to determine if the trachea is midline and to evaluate tracheal length and soft tissue volume. In the child with a short neck and abundant soft tissue, the potential for oropharyngeal airway obstruction is greater.
The rate, depth, and quality of respirations should be evaluated. The pattern of breathing should be noted as well as the rate and depth of respiration. Use of accessory muscles may indicate an increased work of breathing due to an effort to overcome upper or lower airway obstruction. Nasal or upper respiratory obstruction is indicated by noisy or labored breathing. The color, viscosity, and quantity of nasal discharge should be documented. If the child is coughing, the origin of the cough (upper versus lower airway) and the quality (dry or wet) can be evaluated even before auscultation of the lungs. The presence of wheezing, audible stridor, or retractions should be noted. The airway should be evaluated for ease of intubation in the case of urgent intervention. If the child will not open his or her mouth, a manual estimation of the thyrohyoid distance should be made. Children with micrognathia, as in Pierre Robin syndrome or Goldenhar syndrome, may be especially difficult to intubate, especially in an unanticipated situation.
Risk Factors for Airway Compromise or Depression
During sedation, adequate oxygenation and ventilation must be maintained despite a relative decrease in rate and depth of respiration. Any condition that causes airway compromise should be thoroughly evaluated prior to administration of sedation agents to determine if alteration in respiratory parameters will result in impaired ventilation.
During normal breathing the flow of air is laminar. As previously mentioned the resistance is inversely proportional to the fourth power of the radius. Increased airway resistance occurs when the diameter of an airway is decreased under constant pressure. The radius of an airway may be decreased by circumferential edema, external compression, mucous, secretions, or bronchoconstriction. The work of breathing increases in patients with upper or lower airway disease. Increased airway resistance, decreased lung compliance, and altered central control of respiration will all affect the adequacy of respiration.
Adequacy of respiration may be based on respiratory rate, respiratory effort, tidal volume, chest auscultation, and pulse oximetry. The normal respiratory rate in infants under 1 year of age is up to 30 breaths per minute. The respiratory rate declines to 20 breaths per minute by age 8 years and equals the adult rate of 16–17 breaths per minute by age 18. Alterations in the respiratory rate can indicate underlying comorbidity such as fever, pain, acidosis, and sepsis in tachypneic patients and impending cardiovascular collapse in the bradypneic patient. Increased respiratory effort as recognized by nasal flaring, chest retractions, and uncoordinated chest excursions should alert the clinician that an increased work of breathing may increase if excessive sedation is administered.
Noisy breathing due to obstructed airflow is known as stridor. Inspiratory stridor results from upper airway obstruction; expiratory stridor results from lower airway obstruction; and biphasic stridor is present with midtracheal lesions. The evaluation of a patient with stridor begins with a thorough history. The age of onset suggests a cause since laryngotracheomalacia and vocal cord paralysis are usually present at or shortly after birth, whereas cysts or mass lesions develop later in life. Information indicating positions that make the stridor better or worse should be obtained, and placing a patient in a position that allows gravity to aid in reducing obstruction can be of benefit during anesthetic induction.
Patients at risk for airway compromise may have either anatomic or physiologic abnormalities that may predispose them. Anatomic abnormalities may cause the oropharyngeal or tracheobronchial airway to be compromised and ventilation to be impaired by small changes in position. The anatomic imbalance between the upper airway soft tissue volume and the craniofacial size contributes to pharyngeal airway obstruction. Pharyngeal size is determined by the soft tissue volume inside the bony enclosure of the mandible. The magnitude of pharyngeal muscle contraction is controlled by neural mechanisms and the interaction between the anatomical balance and neural mechanisms, which are suppressed in sedated patients, determines pharyngeal airway size and patient ability to maintain a patent airway. An anatomic imbalance between the upper airway soft tissue volume and craniofacial size will result in obstruction. Anatomic imbalance may be compensated for by enhanced neural mechanisms that regulate pharyngeal dilator muscles in patients during wakefulness. When neural mechanisms are suppressed during sleep or sedation, relaxation of pharyngeal dilator muscles occurs and the pharyngeal airway severely narrows [12]. Small changes in function in the setting of normal anatomy may similarly cause inadequate oxygenation. Increasing the distance between the mentum and cervical column will transiently relieve the obstruction. This is achieved by positioning the patient in the sniffing position. Similarly, the sitting position displaces excessive soft tissue outside the bony enclosure through the submandibular space.
Laryngomalacia is the most common cause of stridor in infants and is usually benign and self-limited. It occurs during inspiration and is most often due to a long epiglottis that prolapses posteriorly and prominent arytenoid cartilages with redundant aryepiglottic folds that fall into the glottis and obstruct the glottic opening during inspiration (Fig. 7.8). There is little obstruction during exhalation since the supraglottic structures are pushed out of the way during expiration. Intermittent low-pitched inspiratory stridor is the hallmark symptom, which appears during the first 2 weeks of life. Symptoms peak at 6 months of age when they are at their worst, then gradually resolve. Although most children are symptom-free by 18–24 months, the stridor can persist for years. The definitive diagnosis is obtained by direct laryngoscopy and rigid or flexible bronchoscopy. Preliminary examination is usually carried out in the surgeon’s office. A small, flexible fiberoptic bronchoscope is inserted through the nares into the oropharynx, and the movement of the vocal cords is observed [13]. Other etiologies include foreign body aspiration, infection such as croup or laryngotracheobronchitis, edema, or mass lesions such as cyst or tumor.
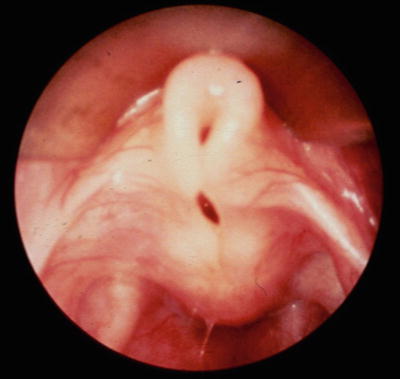
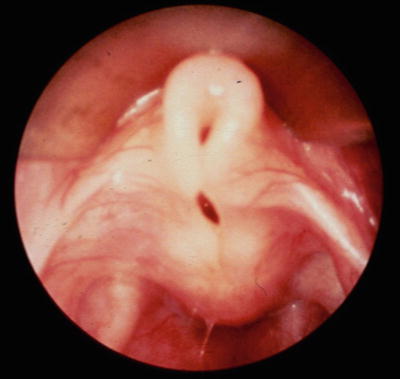
Fig. 7.8
Larynx of an infant with laryngomalacia (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
Grunting is a low-pitched sound that results when a patient exhales against a closed glottis and is heard on exhalation. Infants and children often grunt to keep the small airways and alveoli open in an attempt to optimize ventilation and oxygenation. The presence of grunting may be a sign of severe respiratory distress and impending respiratory failure. Underlying causes include pneumonia, acute respiratory distress syndrome, pulmonary edema, congestive heart failure, and abdominal splinting.
Wheezing during inspiration or exhalation, or both, indicates intrathoracic obstruction of small airways. It may be a result of intrinsic reactive airways, bronchospasm, or foreign body aspiration. Hypoxemia that is present in the wheezing patient may worsen during administration of sedation.
One of the most challenging decisions in caring for children is establishing criteria for cancelation of a procedure in the presence of an upper or lower respiratory infection. Children presenting with symptoms of uncomplicated upper respiratory infection who are afebrile, with clear secretions, and appear otherwise healthy should be able to safely undergo sedation. A history of nocturnal dry cough, wheezing during exercise, and wheezing more than three times in the recent 12 months, or a history of present or past eczema may be associated with an increased risk for bronchospasm, desaturation, or airway obstruction [14]. Nasal congestion, purulent sputum production, and a history of reactive airway disease are predictors of adverse respiratory events, and children with these advanced symptoms of upper and potential lower respiratory disease should not undergo sedation [15].
There are many syndromes that have anatomic components related to the airway. A large tongue is associated with Down, Hunter, Hurler, and Beckwith-Wiedemann syndromes. Congenital hypothyroidism and Pompe disease are also associated with a large tongue. Patients with Pierre Robin, Treacher Collins, and Goldenhar syndromes, as well as children with congenital hemifacial microsomia, have micrognathia, high arched palate, and a potential to have early airway obstruction when sedated. Children with tonsillar hypertrophy are at risk for mechanical airway obstruction due to large tonsils occupying a greater portion of the oropharyngeal airway than normal-sized tonsils.
Former premature infants are at risk for untoward respiratory events during sedation. There is a more gradual slope of the CO2 response curve in the preterm infant, which predisposes this group of patients to apnea. All neonates exhibit periodic breathing, which is manifested as interrupted ventilation by self-corrected short periods of apnea without desaturation or bradycardia [16]. This tendency diminishes by 45 weeks postconceptual age. Apnea of prematurity and postanesthetic apnea are predominantly central in origin, with about 10 % due to mechanical obstruction. The response to airway obstruction with apnea is common in infants with periodic breathing and decreases with increasing postnatal age. In the sedated neonate and former premature infant, benign periodic breathing may evolve into frank apnea, which must be managed by stimulation or assisted ventilation. To detect postanesthetic or post-sedation apneic events, it is suggested that infants whose age is under 56 weeks postconception be monitored for 24 h after the procedure [17].
Conditions that interfere with the integrity of the laryngeal inlet or upper larynx may impair effective ventilation as a result of partial or complete airway obstruction. Upper respiratory infections cause increased secretions, which may occlude the larynx in addition to the inflammatory response that can compromise the internal diameter of the laryngeal inlet. Laryngotracheobronchitis or croup also decreases the internal laryngeal diameter and produces the same clinical outcome. The incidence of epiglottitis has decreased dramatically in the past decade but may still be encountered. These patients have not only inflammation of the epiglottis but edema of the surrounding structures, which severely restricts the size of the larynx and encroaches on the area for ventilation to occur.
Patients who have sustained airway trauma or thermal injury should be considered in this category as well. Children who have experienced prolonged intubation may have decreased laryngeal inlet diameter as a result of fibrosis from congenital or acquired subglottic stenosis (Figs. 7.9 and 7.10). Any agent that will decrease the pharyngeal muscle tone and rate and depth of respiration in this setting should be given with extreme caution and warrants vigilance. Other conditions that restrict the laryngeal inlet are subglottic stenosis, laryngeal cysts, and papillomatosis.
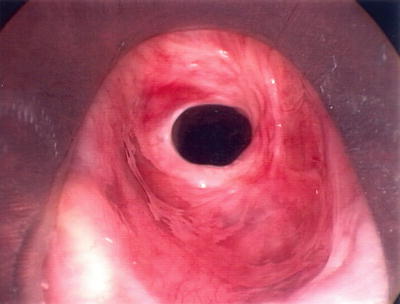
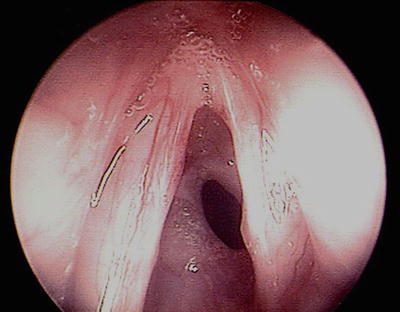
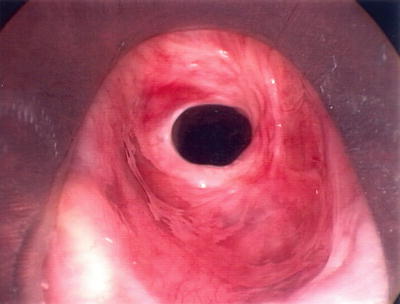
Fig. 7.9
Larynx of an infant with congenital subglottic stenosis (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
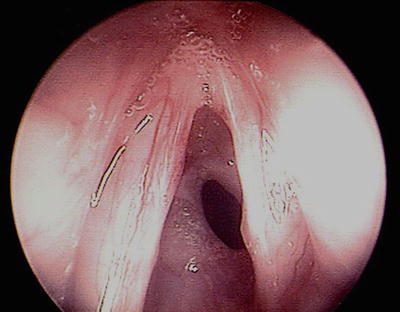
Fig. 7.10
Larynx of an infant with acquired post-intubation subglottic stenosis. (Photo courtesy of Reza Rahbar, DMD, MD, Children’s Hospital Boston)
There is a similar concern for narrowing and compromise of the larynx from external factors. Goiter or other tumors of the neck that are extrinsic to the larynx may cause compression and functional restriction to ventilation. Children with arthrogryposis or congenital abnormalities in which the neck is fused may have difficulty with positioning and subsequent ventilation when airway function is depressed during sedation.
Children with an anterior mediastinal mass are at significant risk for airway compromise during sedation due to compression of the intrathoracic larynx (Figs. 7.11 and 7.12). Although lymphomas constitute the largest group of masses that arise in the anterior mediastinum, other masses that may present in this location include teratomas, cystic hygromas, thymomas, hemangiomas, sarcomas, desmoid tumors, pericardial cysts, and diaphragmatic hernias of the Morgagni type.


Fig. 7.11




A 20-month-old male with a large anterior mediastinal mass
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


