Allergic
Eosinophilic colitis
Vascular
Necrotizing enterocolitis
Henoch-Schönlein purpura
Hemolytic uremic syndrome
Neuromuscular
Hirschsprung’s disease
Chronic pseudo-obstruction
Immunodeficiencies (congenital and acquired)
Infectious
Bacterial, parasitic, viral
Chronic idiopathic
Ulcerative colitis
Crohn’s disease
Lymphocytic colitis
Collagenous colitis
Autoimmune enterocolitis
Treatment related
Antibiotic-associated colitis
Changes induced by other drugs
Diversion colitis
Neutropenic colitis
Pouchitis
Graft vs. host disease
Fibrosing colonopathy
Preparation and Procedure-Induced Artifacts
Nondisease-related alterations in the colonic mucosa may be induced by certain enemas used in bowel preparation or by the procedure itself. For example, soap suds enemas may result in hyperemia and edema of the bowel, especially noted on endoscopy [1]. Oral sodium phosphate solutions (oral fleet) may cause aphthoid-like erosions endoscopically similar to Crohn’s disease [2]. These correspond histologically to large lymphoid aggregates, although edema, hemorrhages or mild acute inflammation have also been described (Fig. 21.1) [3]. Mucin depletion and increased cell proliferation can be noted in the crypts [4, 5]. Hypertonic saline and bisacodyl enemas can cause mucin depletion, focal disruption of surface epithelium, mild acute inflammation and edema, which usually resolve within 1 week [6]. Minor trauma to the mucosa may allow penetration of gas insufflated into the bowel during endoscopy, resulting in “pseudolipomatosis,” characterized by the formation of numerous clear spaces in the mucosa (Fig. 21.2) [7]. Cleansing solutions used to disinfect endoscopes, such as hydrogen peroxide, may produce adherent mucosal plaques, mucosal vacuolar changes, congestion, hemorrhage, and even pseudolipomatosis [8, 9].
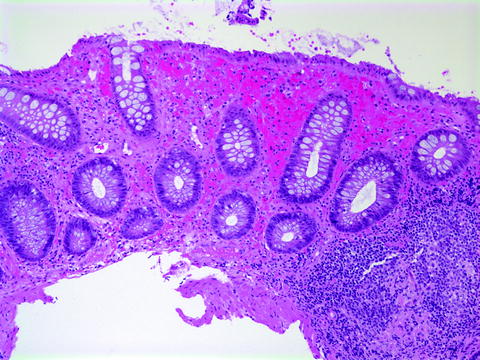
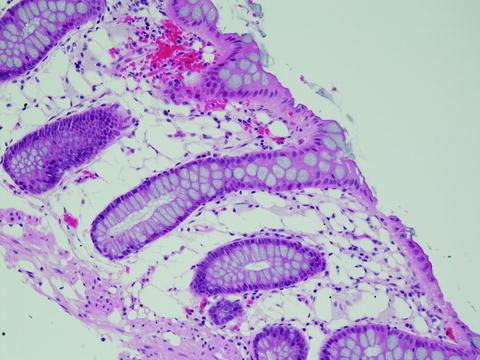
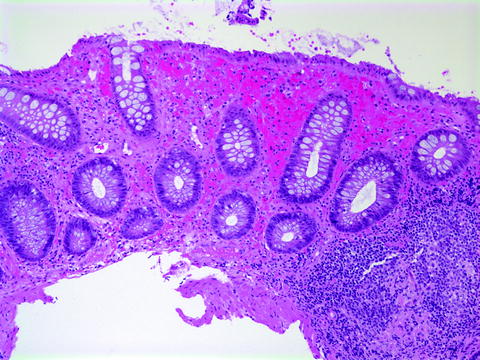
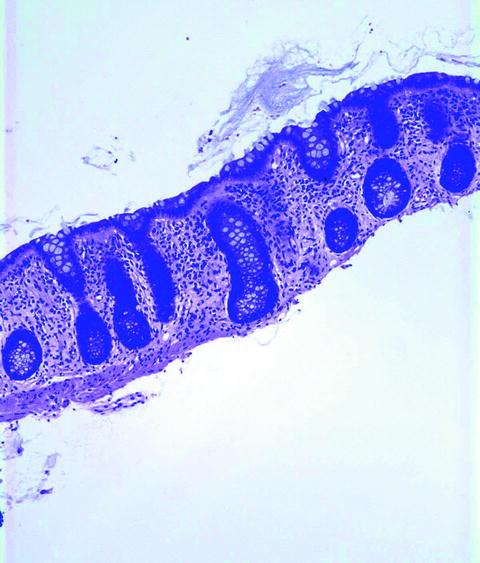
Fig. 21.1
Histological features of phosphate enema effect. Superficial mucosal hemorrhage and focal mucin depletion of the colonic surface epithelium are noted. There is no inflammation of the crypts (Hematoxylin-eosin (H + E), ×100)
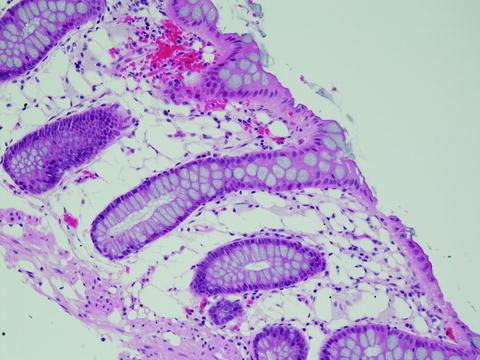
Fig. 21.2
Pseudolipomatosis. Numerous clear spaces in the lamina propria resulting from infiltration of the mucosa by insufflated gas during endoscopy suggests the presence of fat vacuoles (H + E, ×200)
Major Histologic Features Noted in Mucosal Specimens
Active colitis refers to the presence of neutrophils either in the lamina propria, in crypt epithelium (cryptitis) or within the lumen, forming small abscesses (crypt abscesses). Neutrophils confined to the lumen of mucosal vessels are not considered part of the process of active colitis. A predominantly neutrophilic infiltrate without significant architectural changes is generally a feature of diseases with a self-limiting course, such as infections and drug reactions. Neutrophils in these cases are frequently confined to the superficial portion of the mucosa, and may be associated with small erosions or ulcers (Fig. 21.3).
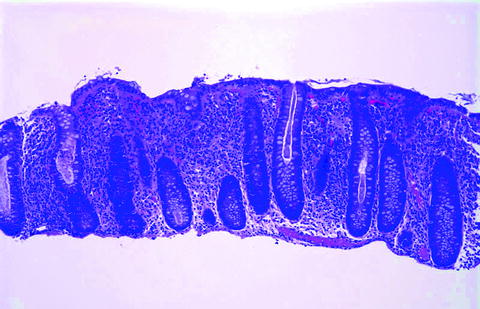
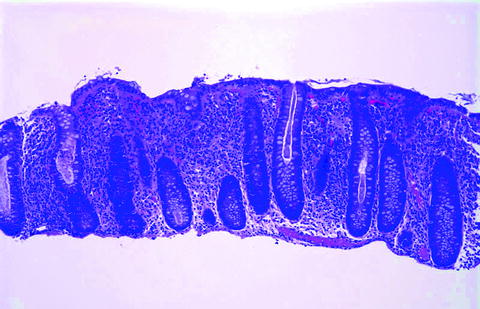
Fig. 21.3
Colitis in a 3-year-old due to Salmonella. There is a superficial, mild inflammatory infiltrate with small crypt microabscesses without significant crypt architectural changes, associated with superficial hemorrhages. Hematoxylin-eosin (H + E), ×100
Focal active colitis (FAC) is observed in acute self-limited colitis and can be an early manifestation of idiopathic IBD. In a recent report of 29 pediatric patients with FAC, 8 developed Crohn’s disease, whereas the other patients had either infectious colitis or remained idiopathic [10].
Eosinophilic colitis refers to a patchy or diffuse infiltrate dominated by eosinophils, usually with infiltration of the crypt or surface epithelium. Wide variations in the number of eosinophils in the normal colonic mucosa are due to differences in specimen site (greater numbers of eosinophils in the cecum as opposed to the rectum), age, and geography [11, 12]. In infants, the main consideration is milk allergy; parasitic infection and chronic IBD are also possible.
The features of chronic colitis are based on the recognition of architectural changes in the mucosa, such as a “villiform” aspect of the surface epithelium, crypt destruction and atrophy, and shortening of the crypts with irregular branching and loss of their regular outline. Shortening of the crypts is most often due to the presence of a basally situated chronic inflammatory infiltrate (basal plasmacytosis), which separates the base of the crypts from the muscularis mucosae (Fig. 21.3). The presence of an increased mononuclear inflammatory cell infiltrate, usually an integral part of the process, is the least useful histologic parameter given the wide range in numbers of lymphocytes and plasma cells in normal specimens. Though considered a hallmark of chronic idiopathic IBD, histologic features of chronicity may also be seen in other settings in pediatrics, such as immunodeficiency disorders, metabolic diseases such as glycogen storage disease type Ib, or result from mucosal injury due to ischemia or Hirschsprung’s disease. Chronic active colitis refers to the presence of a neutrophilic infiltrate superimposed on the above changes, and is usually seen during exacerbations of IBD.
Acute Self-Limited Colitis and its Distinction from IBD
Endoscopic features alone may not reliably distinguish acute self-limited colitis (ASLC) from IBD. Stool cultures and duration of diarrhea may help, as patients without an identifiable pathogen or in whom diarrhea lasts more than several weeks are more likely to have IBD. However, microbiologic investigations can reveal a colitis-causing pathogen such as Salmonella, Campylobacter, and Yersinia in up to 15% of patients with IBD [13]. ASLC is characterized by a predominantly neutrophilic infiltrate without significant crypt architectural changes. Neutrophils in these cases predominate in the superficial portion of the mucosa, and may be associated with small erosions or ulcers (Fig. 21.3) [14]. Neutrophils may also invade the crypt epithelium (cryptitis) or form small abscesses within the crypt lumen (crypt abscesses). Although numerous crypt abscesses suggest UC, they may be noted in CD as well as in infections and Clostridium difficile-related injury. The histologic diagnosis of IBD rests on the recognition of chronic mucosal damage, chronic colitis. Multiple biopsy studies of new onset IBD in adults have shown that histologic features can reliably distinguish IBD from self-limited colitis [14–17]. These include irregular branching of the crypts with loss of their regular outline, shortening of the crypts, and areas of crypt loss. Shortening of the crypts most often results from the presence of a basal chronic inflammatory infiltrate (basal plasmacytosis) between the base of the crypts and the muscularis mucosae (Fig. 21.4). The presence of an increased mononuclear inflammatory cell infiltrate alone is the least useful histologic marker given the variable numbers of lymphocytes and plasma cells in normal specimens.
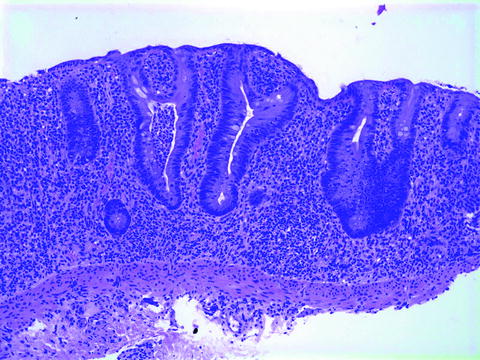
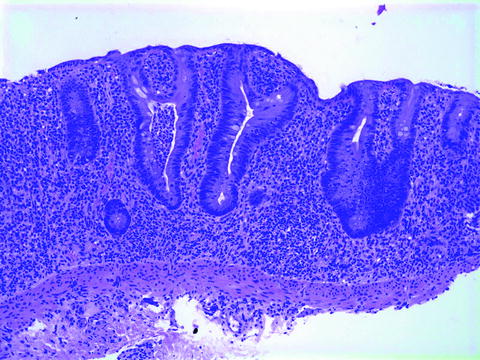
Fig. 21.4
Histological features of IBD. Chronic mucosal damage is characterized by irregular branching of the crypts, increased inter-cryptal distance and by shortening of the crypts, due to the presence of an inflammatory infiltrate in the deep mucosa separating the base of the crypts from the muscularis mucosa (basal plasmacytosis). In addition, there is goblet cell depletion and a micro-abscess. H + E, ×100
Histologic Features of Early-Onset IBD
Despite the importance of recognizing chronic mucosal changes in the biopsies of patients with IBD, it has been well-documented that initial colonic or rectal biopsies from 10 to 34% of pediatric patients ultimately shown to have UC-lacked architectural distortion or other histologic features of chronic colitis [18–23]. This is seen particularly in younger patients (<10 years), and may be due to shorter duration of symptoms or longer progression to chronicity in children (Fig. 21.5a,b) [24]. FAC may be a feature of self-limited colitis, but may also be an early manifestation of IBD [10]. Close follow-up and repeat biopsies may be necessary in these cases. Increased mucosal eosinophils may be seen in the earliest biopsies of children eventually proven to have IBD, prompting a diagnosis of food allergy. In a recent case series of IBD diagnosed in 16 children less than 2 years of age, 6 children had an initial diagnosis of allergy [25]. On the other hand, histologic features similar to IBD may be seen in patients with primary immunodeficiencies and autoimmune enteropathy [26]. These conditions should always merit consideration when clinical manifestations of IBD occur in younger children. Histologic features which may point to a correct diagnosis in these patients include lack or paucity of plasma cells in the inflammatory infiltrate (as in Common Variable Immunodeficiency or Severe Combined Immunodeficiency), extensive crypt apoptotic activity, or absence of goblet and Paneth cells (as in autoimmune enteropathy). Mutations in genes coding for cytokines, such as interleukin-10, have been demonstrated in patients with the onset of IBD in infancy [27].
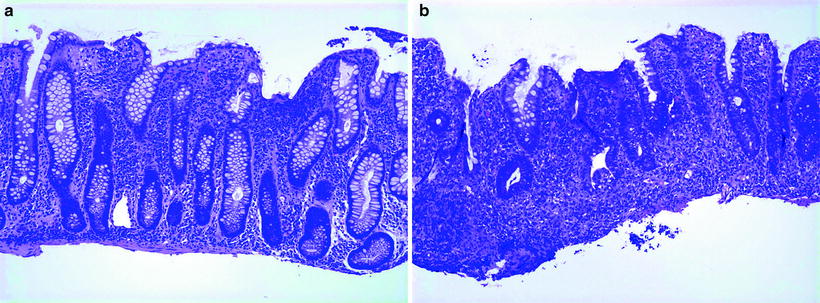
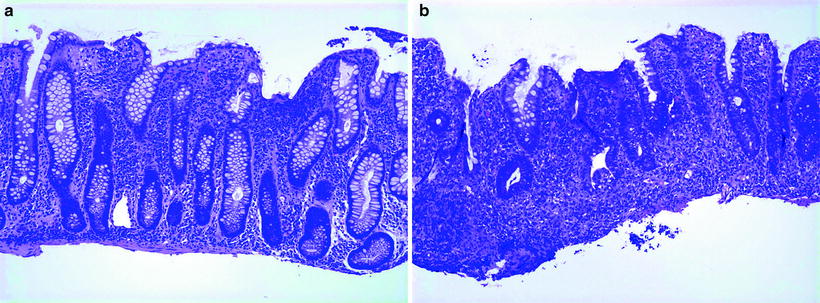
Fig. 21.5
(a) Colon biopsies of a 3-year-old girl with several months onset of diarrhea and abdominal pain. There is a lymphoplasmacytic inflammatory infiltrate with mild architectural distorsion manifested by a slight irregularity in the outline of the crypts. (b) Follow-up biopsies several months later show more advanced disease with crypt atrophy and basal plasmacytosis both H + E, ×100
Characteristic Features of Ulcerative Colitis and Crohn’s Disease
The macroscopic and microscopic features which distinguish UC and Crohn’s disease are, in most respects, similar in children and adults, and are outlined in Table 21.2. Biopsy features helpful in differentiating these two entities in mucosal biopsies are outlined in Table 21.3. It should be noted, however, that, especially in early stages of disease, biopsies, even in combination with clinical and radiologic features, may not allow distinction between these two entities. Absence of ileal involvement does not rule out CD, and appears to be more frequent in younger patients with CD than older children or adults [28]. Similarly, diffuse colitis may be a manifestation of both CD and UC in children.
Table 21.2
Distinguishing features of ulcerative colitis and Crohn’s disease
Ulcerative colitis | Crohn’s Disease | |
|---|---|---|
Macroscopic | ||
Rectal involvement | Yesa | Variable |
Distribution | Diffusea | Segmental or diffuse |
Terminal ileum | “Backwash” ileitis | Often thickened and stenosed |
Serosa | Usually normal | “Creeping fat” |
Bowel wall | Normal thickness | Frequently thickened |
Mucosa | Hemorrhagic | Cobblestone and ulcers linear |
Pseudopolyps | Frequent | Less common |
Strictures | No | Common |
Fistulas | No | Common |
Involvement of gut proximal to colon | Nob | Common |
Microscopic | ||
Inflammation | Confined to mucosa and superficial submucosa | Transmural |
Lymphoid hyperplasia | Infrequent | Common |
Crypt abscesses | Extensive | Focal |
Mucus depletion | Frequent | Infrequent |
Deeply situated sarcoid-like granulomas | No | Yes |
Fissures and sinuses | No | Yes |
Villous surface transformation | Common | Infrequent |
Submucosal fibrosis | Rare | Common |
Neuromatous hyperplasia | Rare | Common |
Table 21.3
Distinguishing features of ulcerative colitis and Crohn’s disease in biopsies
Ulcerative colitis | Crohn’s disease | |
|---|---|---|
Distribution of inflammation | Diffuse | Frequently focal |
Rectal involvement | Yesa | Variable |
Proximal > distal colonic involvement | Noa | Frequent |
Crypt abscesses | Diffuse | Variable, often focal |
Villous surface appearance | Common | Occasional |
Pyloric metaplasia | Infrequent | Typical |
Mucin depletion | Frequent | Infrequent |
Granulomas | Superficial; foreign body | Deep; sarcoid-like |
UC is classically defined as diffuse chronic mucosal inflammation limited to the colon, which invariably affects the rectum, and extends proximally in a symmetric uninterrupted pattern to involve part or all of the large intestine. The mucosa characteristically exhibits a diffuse hemorrhagic appearance (Fig. 21.6).


Fig. 21.6
Ulcerative colitis. Specimen from a total colectomy reveals a diffusely hemorrhagic granular mucosa from the rectum (on the right) to the ascending colon (on the left). The process is macrocospically continuous, without “skip” areas. Uninvolved appendix with a small amount of terminal ileum is also present
Microscopically, ulcerative colitis is characterized by inflammation limited to the mucosa and superficial submucosa (Fig. 21.7); deeper layers of the bowel are only exceptionally involved, as in toxic megacolon. Infiltration of the mucosa by neutrophils, with cryptitis, epithelial degeneration, goblet cell depletion and crypt abscesses are characteristic though relatively nonspecific microscopic features of active UC. Chronicity, as previously defined, is characterized by crypt architectural changes such as irregular branching and atrophy, usually accompanied by a mononuclear inflammatory infiltrate. Increased crypt epithelial turnover in UC results in goblet cell depletion and Paneth cell metaplasia [29], less frequently observed in CD. The latter must be interpreted with caution in pediatric cases, as Paneth cells can be present in the distal colon in normal young children. Crypt abscesses are not specific, but when diffuse are suggestive of UC, whereas they tend to be more isolated in Crohn’s disease [30]. Rupture of crypt abscesses into the lamina propria or erosions may result in collections of histiocytes which may simulate but should be distinguished from true granulomas (Fig. 21.8).
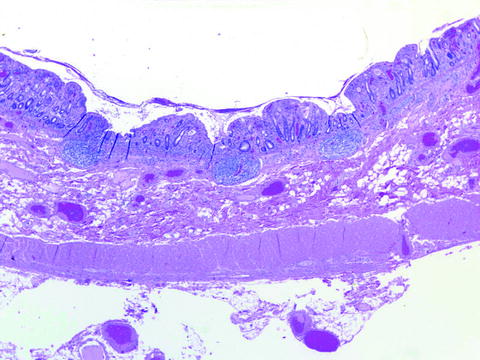
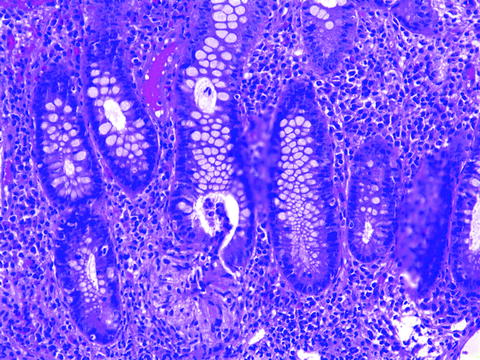
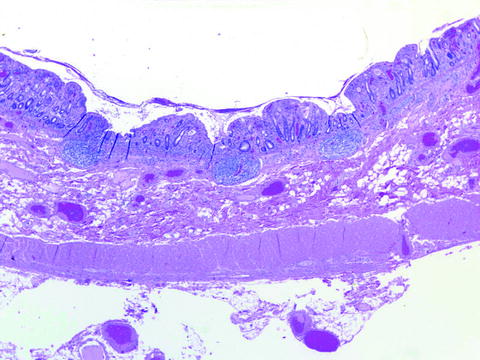
Fig. 21.7
Histologic section from the specimen in Fig. 21.6 is characterized by a diffuse inflammatory process limited to the mucosa and superficial portion of the submucosa. The colonic wall is of normal thickness
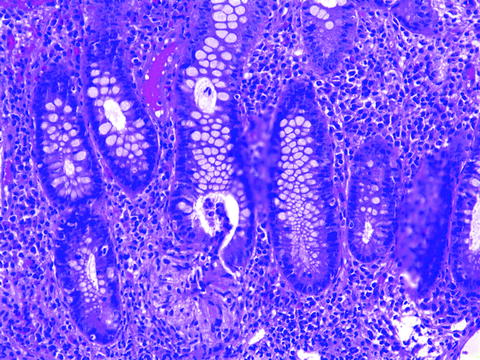
Fig. 21.8
Crypt microabscess with rupture resulting in a histiocytic reaction around the base of a crypt in a colonic biopsy from an 8-year-old girl with ulcerative colitis. H + E ×200
Pseudopolyps, more commonly found in UC than CD, are discrete areas resulting from surviving islands of mucosa or heaped-up granulation tissue. The latter are more accurately referred to as “inflammatory polyps.” Occasionally, regenerating mucosa within such an inflammatory polyp may form irregular, dilated glands, which bear a marked resemblance to retention or “juvenile” polyps [30]. In contrast to adenomas, pseudopolyps have a short stalk and are generally smooth-surfaced (Fig. 21.9). Extensive arborization and fusion of the polyps may result in mucosal bridging.
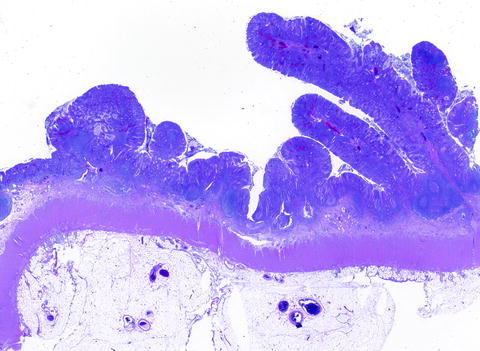
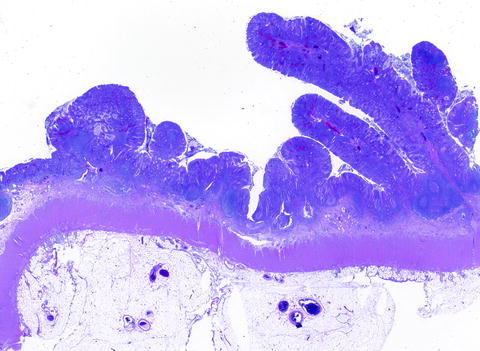
Fig. 21.9
Inflammatory “pseudopolyps” in a patient with ulcerative colitis. The base of the polyps are broad, and the polyps consist of heaped-up regenerating mucosa with an inflammatory infiltrate
In contrast to UC, CD features segmental intestinal involvement, with thickening of the bowel wall consequent to transmural inflammation and fibrosis, resulting in obstructive strictures, especially in the ileocecal area. The serosa is typically congested, with the presence of adhesions and fat wrapping, or “creeping fat.” Mucosal involvement can be patchy and discontinuous. Aphthous ulcers overlying lymphoid tissue are among the earliest lesions observed endoscopically, but are nonspecific and may be seen in other conditions. Uneven involvement of the mucosa results in a typical “cobblestone” appearance (Fig. 21.10). Transmural involvement in resected specimens and the presence of granulomas are the major histologic features which distinguish CD from UC and other colitides. Transmural disease in CD usually results from submucosal edema, fibrosis and inflammation, typically in the form of lymphoid aggregates, also involving the muscle layers and the serosa (Fig. 21.11). Intramural abscesses are also noted, with fistulae, perforations and adhesions, which can involve multiple loops of bowel and form a mass. The identification of pyloric metaplasia indicates chronic damage [31], and is seen more frequently with Crohn’s disease than with UC. Lymphangiectasia, neural hyperplasia, and vascular changes are frequently observed in CD and are almost never seen in UC.
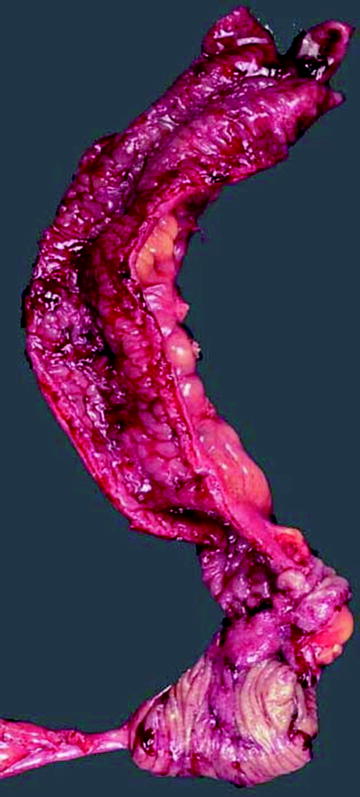
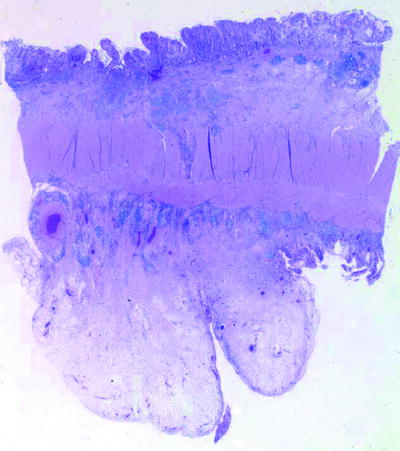
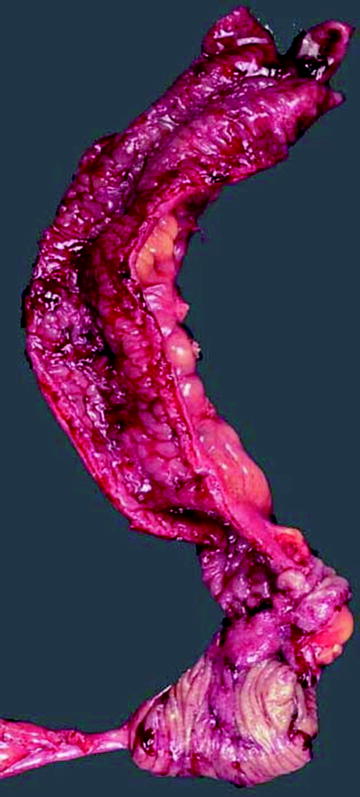
Fig. 21.10
Crohn’s disease. Ileo-cecectomy specimen is characterized by a stricture in the area of the ileo-cecal valve. The mucosa has a “cobblestone” appearance, and the wall appears thickened with prominent and extensively adherent serosal fat. Contrast with Fig. 21.6
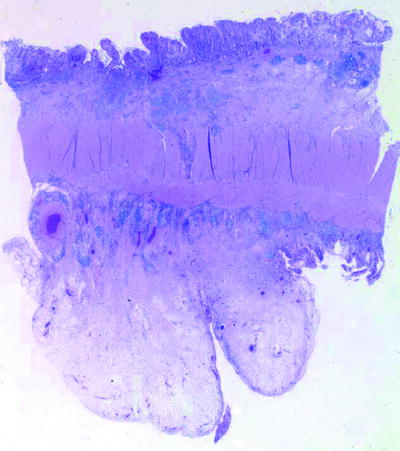
Fig. 21.11
Crohn’s disease. Low power microscopic section demonstrates transmural involvement. Inflammation, in the form of lymphoid aggregates, extends through the muscularis propria into thickened serosal fat. Contrast with Fig. 21.4. H + E, ×10
Granulomas are virtually diagnostic of CD when they are well-formed, non-necrotic, basally situated, and remote from areas of active inflammation (Fig. 21.12). Their presence in biopsies may predate radiologic evidence of disease, and prolonged follow-up is necessary when they are observed in the absence of grossly evident disease [32]. The likelihood of finding granulomas is clearly a function of the diligence with which they are sought, increasing with the number of biopsies and sections examined [33]. Granulomas appear to be more frequently observed in the pediatric age group. One large study in Germany found them in 26% of biopsy specimens from 42% of patients, twice as commonly as in adults [34]. Comparison of initial biopsies of children with and without rectosigmoid granulomas showed similar age of onset of disease in the two groups, though those with granulomas tended to have more extensive disease and perianal complications [35]. Shepherd and colleagues observed granulomas more frequently in their younger patients and those with a shorter clinical course, with an increased prevalence in the more distal portion of the gastrointestinal tract [36]. In a recent study at The Children’s Hospital of Philadelphia, granulomas were identified in 61% of pediatric CD patients undergoing upper and lower endoscopy and were more frequent in untreated patients [37]. In nearly half of those patients, granulomas were present in the upper GI tract, in the terminal ileum, or both, but not in the colon.
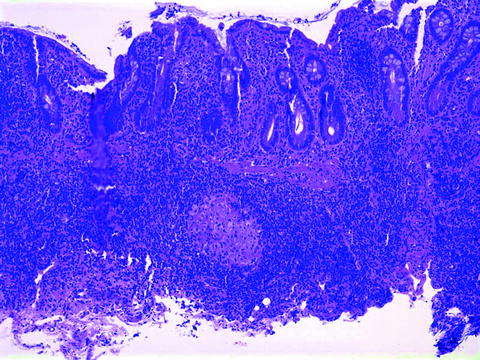
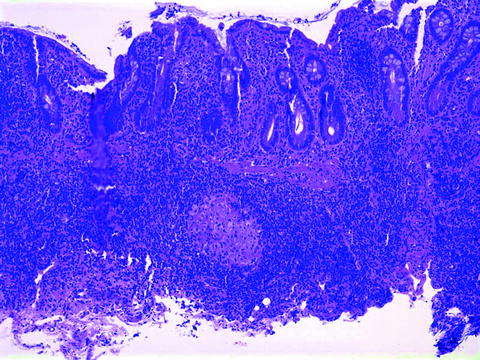
Fig. 21.12
Crohn’s disease, terminal ileum. A well-formed, non-necrotic granuloma is present in the superficial submucosa, away from any ruptured crypt. Contrast with Fig. 21.5. H + E, ×100
Granulomas can also be seen, however, in a number of other conditions (Table 21.4). The granulomas seen in tuberculous infections of the gastrointestinal tract are typically multiple, large and have caseous necrosis [38]. Those associated with yersiniosis are also necrotic, and frequently present in mesenteric lymph nodes [39]. Chronic granulomatous disease can present with a colitis similar to CD [40]. Numerous necrotizing granulomas may be observed; in noninflamed or quiescent cases, collections of pigmented macrophages may be noted in the mucosa (Fig. 21.13).
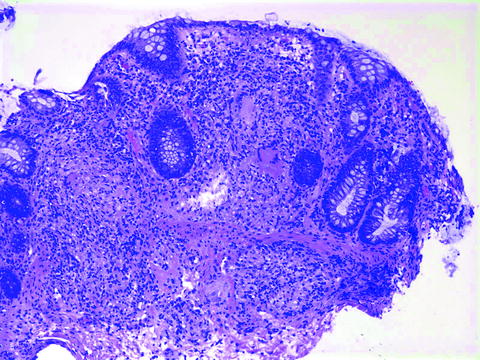
Table 21.4
Differential diagnosis of granulomas in colon specimens
Crohn’s disease |
Infections |
Salmonella (microgranulomas) |
Campylobacter (microgranulomas) |
Mycobacteria (tuberculosis and avium-intracellulare) |
Yersinia |
Brucellosa |
Tularemia |
Schistosomiasis |
Fungal infections |
Mucin and foreign body granulomas |
Chronic granulomatous disease |
Pneumatosis intestinalis |
Malakoplakia |
Sarcoidosis |
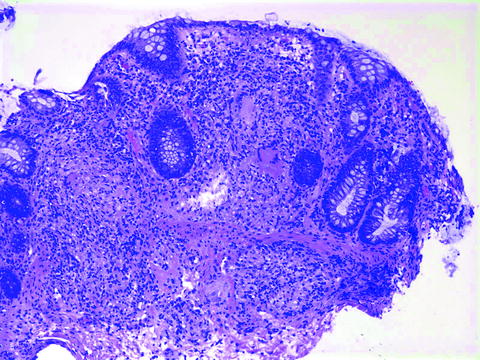
Fig. 21.13
Chronic granulomatous disease. Colon biopsy from a 5-year-old boy reveals numerous granulomas throughout the mucosa and submucosa. H + E ×100
Colonic malignancy is a well-recognized long-term complication of UC. Recent evidence suggests that patients with Crohn’s colitis incur a similar risk of colorectal cancer [41]. Duration of disease and pancolitis are well recognized as risk factors for the development of malignancy, with the risk of cancer increasing over that of the general population by 1% each year after 10 years of disease [42, 43]. Unfortunately, there is a paucity of prospective data describing long-term IBD with early onset ulcerative colitis and ultimate cancer risk in pediatric patients. Other less well characterized risk factors include concomitant sclerosing cholangitis, an excluded, defunctionalized or bypassed segment and depressed red blood cell folate levels [42]. Children who develop colitis before the age of 10 years should undergo colonoscopy screening during their adolescence, and dysplasia and adenocarcinoma have been documented in adolescents and young adults with long-standing colitis [44]. Dysplasia in colitics is generally plaque-like or nodular, frequently referred to as the DALM (dysplasia-associated lesion or mass) lesion (Fig. 21.14a, b) [45]. Epithelial dysplasia generally precedes carcinoma; therefore, yearly surveillance colonoscopy is recommended. Since reliability and patient compliance of serial colonoscopy to detect dysplasia is not perfect, prophylactic colectomy should be considered in any individual who developed ulcerative colitis during childhood.
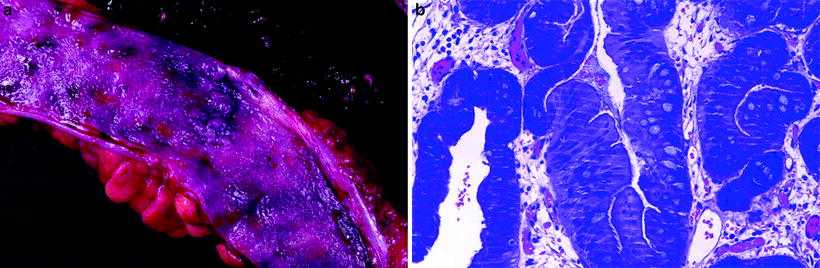
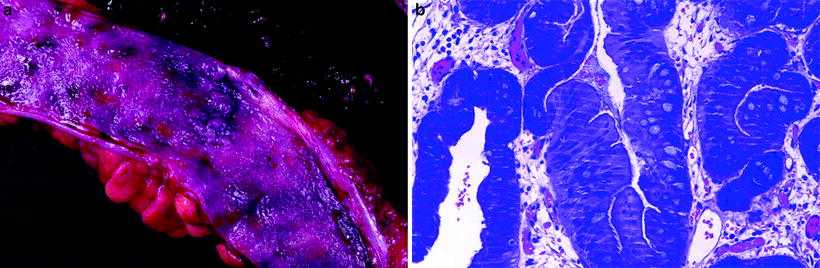
Fig. 21.14
Dysplasia in 16-year-old boy with 10 year history of ulcerative colitis. (a) Plaque-like lesions present in the colon. (b) Histologic section through area of dysplasia in crypt and surface epithelium shows piled-up enterocytes with hyperchromatic nuclei and loss of polarity
“Atypical” Features in the Diagnosis of Ulcerative Colitis Rectal Sparing and Patchiness
Although ulcerative colitis is traditionally considered to be a diffuse process that begins in the rectum and extends proximally in a continuous fashion, a number of studies suggest that initial rectal biopsies in children with UC may not demonstrate mucosal architectural changes as consistently as in adults or may even be “normal” (rectal sparing) (Fig. 21.15). An unequivocal diagnosis of IBD may be more difficult in these cases, as may be distinction between UC and CD.


Fig. 21.15
Rectal sparing in ulcerative colitis. Fifteen-year-old female with several years history of ulcerative colitis which became refractory to medical therapy. The colectomy specimen reveals a diffuse colitis, much milder in the rectum than proximally
Five of 12 children with untreated UC in one study were found to have mild patchy inflammation or normal histology in the rectum [21], whereas relative rectal sparing compared to adults was found in one study of 53 children [23]. In one study, “absolute” rectal sparing, in which evidence of both inflammation and chronicity is absent, is nonetheless infrequent in children with UC (4% of 73 pediatric cases), though “relative” rectal sparing, defined as the presence of inflammation without changes of chronicity, is more frequent, noted in 26% of cases [19]. Faubion et al. identified a 27% prevalence of rectal sparing in children with IBD and sclerosing cholangitis, suggesting the possibility that rectal sparing may be more common in this subset of patients [46]. Moreover, discontinuous involvement and rectal healing have been reported during the course of long-standing disease in adults, which likely results from treatment effect or natural variation in the course of disease and also reflects the current clinical practice of sampling multiple mucosal biopsies over time [47, 48]. Medical therapy can have a profound but variable effect on mucosal histology, ranging from decreased intensity of the inflammatory infiltrate to complete normalization of the mucosa, including discontinuity of mucosal disease in UC [49]. Quiescent colitis is characterized by mucosal atrophy and crypt architectural changes in the absence of the acute inflammation, ulceration, and mucus depletion seen in the active phase (Fig. 21.16).