Chapter 14 The Healthy Newborn
What Happens at Birth?
Birth is a dramatic test of transitional physiology. The newborn must rapidly adapt cardiovascular flow and function, establish lung-based oxygenation, develop endocrine control of body metabolism, adapt neurologic responses to new stimuli, and begin to develop an immunologic defense. Unique features seen only during this transitional time can help identify many potential newborn problems. Specific problems are discussed in Chapter 67.
What Infectious Diseases Pose Risks to the Newborn?
Maternal infections may cause fetal or neonatal diseases, many of which can be treated or prevented by immunizations or prophylaxis (Table 14-1). HIV testing is now recommended for all pregnant women. Factors related to the risk of newborn infection include prematurity, prolonged rupture of membranes, maternal fever during labor, and chorioamnionitis. The mother’s group B streptococcus (GBS) status is important: To prevent transmission of GBS from a colonized mother to the newborn, National Institutes of Health (NIH) guidelines recommend that penicillin be administered to the mother at least 4 hours before birth. It is also important to note whether the mother received any other antibiotics during labor and why. For example, antibiotic prophylaxis may be given in labor for mitral valve prolapse.
Table 14-1 Maternal Infections That Can Affect the Newborn
| Organism | Key Historical Information |
|---|---|
| Varicella-zoster | Maternal and sibling history of disease or immunization. Active varicella in mother near term? Recent exposure by any nonimmune family members? |
| Herpes simplex I and II | Genital herpes: frequency and treatment. Active lesions at the start of labor? |
| Rubella, measles, mumps | Maternal immunization history or result of antibody screen |
| Hepatitis B | History of maternal disease and mode of disease acquisition (IV drugs, multiple sexual partners). Current status of disease (active, carrier). Family tested, immunized? |
| HIV | High-risk behaviors? Results of HIV testing, if done |
| Listeria | Consumption of cold cuts, hot dogs, or unpasteurized cheese |
| Tuberculosis | Immigrant from endemic country? BCG? History of contact or active disease? PPD status of mother and family members |
| Chlamydia | High-risk behaviors. Other STDs? |
| Gonococcus | High-risk behaviors. Other STDs? |
| Syphilis | High-risk behaviors. RPR or VDRL status? Other STDs? |
| Toxoplasmosis | History of exposure (cats, consumption or handling of raw meat or garden products)? Test results? |
| Group B streptococci | Is mother colonized? Results of screening tests? Treatment history? |
BCG, Bacille Calmette-Guérin; HIV, human immunodeficiency virus; IV, intravenous; PPD, purified protein derivative; RPR, rapid plasma reagin; STD, sexually transmitted disease; VDRL, Venereal Disease Research Laboratory.
What Is the Apgar Score?
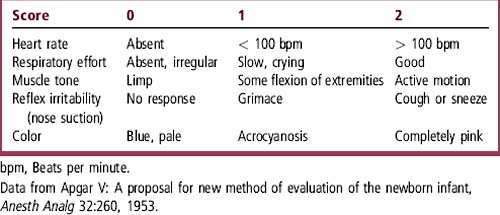
The Apgar score assesses heart rate, respiratory rate, skin color, muscle tone, and response to stimuli at 1 minute and 5 minutes after birth, a physiologically dynamic time when the newborn must make the transition from fetal to extrauterine life (Table 14-2). Each component of the Apgar score may receive 0, 1, or 2 points. A perfectly healthy baby would have an Apgar score of 10.
What Transitional Issues Must I Consider?
Circulation
During the transition period, blood flow is “rerouted” to the lungs as pulmonary vascular resistance falls and the foramen ovale and ductus arteriosus close. Central cyanosis indicates problems such as persistence of the fetal circulatory pattern caused by elevated pulmonary vascular resistance or persistence of right-to-left shunts at the foramen ovale and ductus arteriosus. Congenital heart disease may manifest as central cyanosis that does not respond to oxygen (see Chapter 56).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree