Fig. 2.1
A 23-year-old patient with primary amenorrhea. Transrectal ultrasonography showing a hypoechoic structure behind bladder UT and BL, with the size of 2.0 × 0.8 cm
Infantile Uterus
In late pregnancy or at any time from after birth to puberty, the uterus stops growing. After puberty, the ratio of the uterine body and the cervix is still the same at 1:2 as in infants and young children.
Ultrasound features: All uterine diameters are significantly smaller than a normal uterus; the anterior-posterior diameter (i.e., the thickness) is <2.0 cm; the cervix is relatively longer (Fig. 2.2).
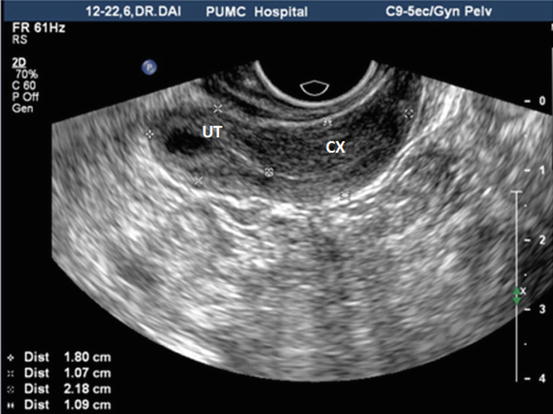
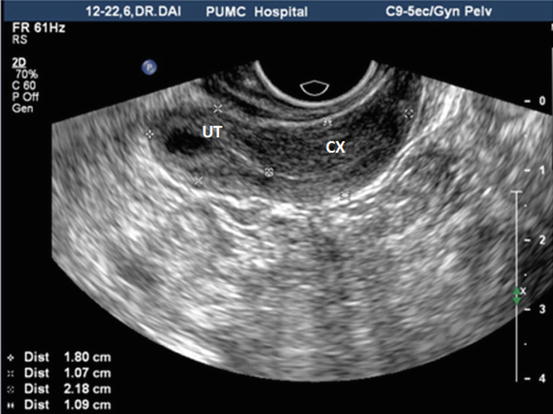
Fig. 2.2
Transvaginal ultrasound showing an infantile uterus. A 24-year-old patient presenting primary amenorrhea. All the uterine diameters are significantly smaller than normal with uterine body size: 1.8 × 1.5 × 1.1 cm, cervical length 2.2 cm, and body/cervix ratio <1
Uterus Didelphys
Both bilateral paramesonephric ducts develop normally but do not join together at midline, so each side has a set of fallopian tube and uterus.
Ultrasound Features
Uterus didelphys under ultrasonic examination would show two completely separate uteri, which are particularly clear on coronal observation. The two completely separate uterine bodies have a deep depression in between them. Both show uterine endometrial echoes (Fig. 2.3); they may be associated with double cervix; then the cervical diameter can be seen widened with two cervical echoes next to each other but completely separated (Fig. 2.4a, b).
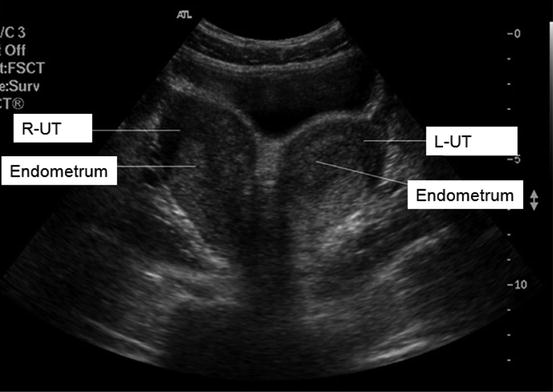
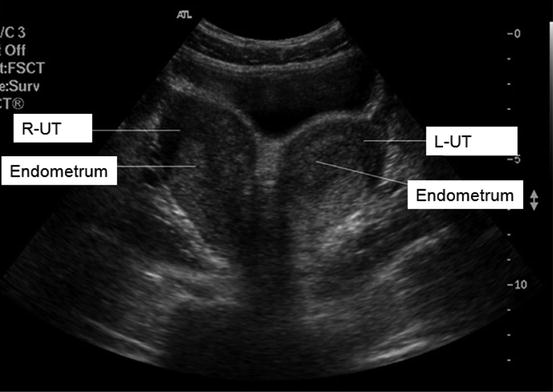
Fig. 2.3
Abdominal ultrasound showing double uterine abnormalities. It shows both the left and right uteri, with uterine body completely separated and two separate endometrial echoes
Fig. 2.4
Double uterine abnormalities (double uterus, double cervix): abdominal ultrasound showing cross-sectional images of two uteri and cervices. (a) Double uterus. (b) Double cervix
Bicornuate Uterus
The ends of the bilateral paramesonephric ducts joined, but not completely at the fundus of the uterus, resulting in a prominent horn on each side of the uterus.
Ultrasound Features
1.
Two-dimensional ultrasonography: Bicornuate uterus should be best observed at cross-sectional scanning. The uterus can be seen with a widened fundus with a “saddle-shaped” depression at the middle (Fig. 2.5) or “Y”-shaped fundus; the uterine endometrial echo is also “Y” shaped.


Fig. 2.5
Bicornuate uterus: an abdominal scan showing an abnormal uterine cross-sectional image, displaying a widened fundus with a saddle-shaped depression at the middle
2.
Three-dimensional ultrasonography: Bicornuate uterus has two separate uterine horns; the upper uterine segment is completely separated but the lower uterine segment is still partly fused. Therefore, the three-dimensional ultrasonography of the coronal section directly shows a depression at the uterine fundus with two uterine horns as butterfly-shaped or as two leaves, and sometimes the bladder revealed a “V”-shaped pressure trace; the uterine endometrium is like a “butterfly wing.”
Rudimentary Horn Uterus
The paramesonephric duct on one side developed normally, but the middle and lower segments of the contralateral paramesonephric duct have stopped growing, thus forming different degrees of rudimentary horn. According to presence or absence of endometrial cavity, it can be divided into either rudimentary horn with or without endometrium. The latter is further divided into either connected or not connected type of rudimentary horn according to whether its endometrial cavity is connected to the contralateral uterine cavity or not.
The symptoms of rudimentary horn uterus pregnancy and interstitial tubal pregnancy are similar. They are asymptomatic in early pregnancy, but due to the poor muscular wall of the rudimentary horn, it cannot accommodate the growing fetus by becoming hypertrophied. The wall will break and rupture, usually from three to 4 months of pregnancy, thus causing severe bleeding and shock, threatening the life of the pregnant woman.
Ultrasound Features
1.
Rudimentary horn may present as a normal uterus in the pelvis, but on one side, it shows a hypoechoic mass in which its echo is similar to that of the myometrium. It might look like a hypoechoic ribbon attached to the main body of the uterus (Fig. 2.6a, b). If it is not connected with the cervix, it can be easily confused as a subserous fibroid. A rudimentary uterine horn with uterine endometrium can be clearly visualized at the luteal phase of the menstrual cycle (Fig. 2.6c); if there are blood clots in the cavity, it may become an echo-free zone.
Fig. 2.6
Rudimentary uterine horn. (a) Abdominal ultrasound showing longitudinal uterine image. (b) Abdominal ultrasound showing a cross-sectional image of the uterus and rudimentary uterine horn with a hypoechoic ribbon connecting the horn with the main body of the uterus. (c) Transvaginal ultrasound showing rudimentary horn of the uterus and its endometrial echo (UT the body of the uterus palace, CX main uterine cervix, R-UT rudimentary horn of the uterus)
2.
Rudimentary horn pregnancy: It is a round mass beside the normal uterus, in which a gestational sac could be seen. Around the gestational sac are obvious muscle tissues, but the endometrial layer around the gestational sac is not connected with the normal cervical canal. On the other hand, the normal uterus can have a thick decidual echo in its uterine cavity or the echo of a false gestational sac.
Septate Uterus
After the fusion of both paramesonephric ducts, the intervening septum has not been absorbed; this divides the uterine cavity into two halves within a normal uterus; if the septum is only partly absorbed, it is an incomplete septate uterus.
Ultrasound Features
1.
Two-dimensional ultrasonography: The uterine appearance is normal, but the diameter of the uterine fundus is wider. Its cross-section shows two uterine endometrial echoes with a central echo of the septum (Fig. 2.7a, b). If the septum extends to the cervix, associated with two full endometrial echoes, it is a complete septate uterus; if the endometrial echoes from both sides merge in the middle or lower uterine cavity, it is an incomplete septate uterus.
Fig. 2.7
Septate uterus: (a) an abdominal ultrasound showing a cross-sectional image of two endometrial echoes (marked by arrows) separated by a septum at the middle of the uterus. (b) A central septum (marked by an arrow) in the middle of the uterus
2.
Three-dimensional ultrasonography: Two-dimensional ultrasound images are difficult to obtain a coronal imaging so it is more difficult to differentiate the types of septate uterus. Three-dimensional ultrasound scan can provide coronal uterine images, hence to obtain a direct visualization of the uterine endometrium. On a 3D coronal image, there is a clear low echo strip (septum) similar to the uterine muscular wall. The septum extends from the fundus of the uterus to the cervix, either reaching it (a complete septate uterus) or not reaching it (an incomplete septate uterus).
The two endometria of the incomplete septate uterus merge at the lower uterine segment at an acute angle <90° as a “Y”-shaped image (Fig. 2.8); for a complete septate uterus, the septum reaches the cervix, and the uterine endometria image present as a “V”-shaped image (Fig. 2.9a, b).


Fig. 2.8
Incomplete septate uterus: transvaginal 3D ultrasound showing endometrial echo as a “Y”-shaped image. The uterine cavity is separated in its upper half and shows a midline echo from its middle downward
Fig. 2.9
Complete septate uterus: transvaginal 3D ultrasound showing endometrial echo as a “V”-shaped image; the uterine cavity with a hypoechoic middle septum. (a) 3D multiplanar images for 3D reconstruction 1,2,3. (b) Displaying a 3D image
Three-dimensional ultrasound scan can clearly show the septum in the uterine cavity of a septate uterus, its length, and its identification as a complete or incomplete septate uterus. Furthermore, it can also show the shape of the septum (Fig. 2.10a, b), its thickness at different levels of the uterus, etc. (Fig. 2.11a, b).
Fig. 2.10
3D transvaginal ultrasound of an incomplete septate uterus showing different shapes. (a) shows a wider septum. (b) shows a narrower and longer septum than the septum in (a)
Fig. 2.11
3D transvaginal ultrasound showing a different morphology of septate uterus. (a) shows a septum extending from the fundus to the cervix with gradually narrowing septum. (b) shows a wider upper 1/3 septum and narrower lower 2/3 septum
The clinical application of 3D ultrasonography gives a more accurate diagnosis of septate uterus and it is a direct visualization method. It also provides reliable information for the subsequent surgical treatment. The combination use of 3D ultrasound and saline hysterography (3D-HSG) further enhances the 3D ultrasound diagnosis. This will be easier to observe the morphology of the uterine septum and its relationship with the cervix and to determine the type of septate uterus. At the same time, it permits a timely diagnosis of any other associated uterine diseases such as endometrial polyps.
Arcuate Uterus
It is a minor uterine anomaly in which the intervening septum at the uterine fundus is not fully absorbed after fusion. It has a localized muscular hypertrophy in the central part of the fundus and slightly protrudes into the uterine cavity from the fundus.
Ultrasound features: The cross section showed muscular thickening at the central part of the uterine fundus, slightly protruding into the uterine cavity. This feature is shown more clearly on the coronal plane in the 3D image (Fig. 2.12). The endometrium at the uterine fundus is shown as a curved concave, the angle between the two endometria > 90°; the shape and contour of the uterus are normal.
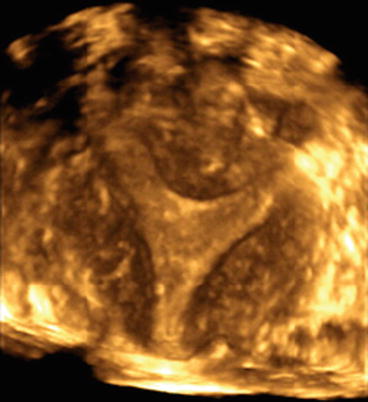
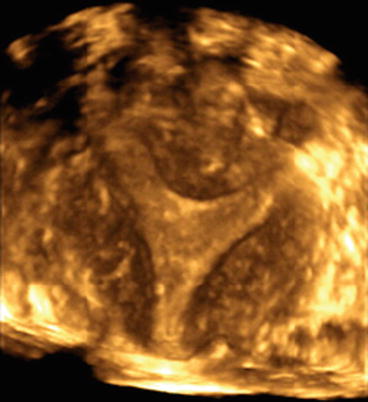
Fig. 2.12
Arcuate uterus: transvaginal 3D ultrasound image showing muscular thickening at the central part of the uterine fundus, slightly protruding into the uterine cavity, with a concave curved endometrium.
Other Ultrasound Features of Uterine Anomalies
1.
Uterus didelphys may be misdiagnosed as uterine fibroids. Uterine fibroid sticks out from a uterus and may also change the shape of the uterus and be mistaken as a uterus didelphys. The key points for identification of uterine fibroid are the absence of endometrial echoes in uterine fibroid and the lower echo levels compared to the normal uterine myometrium.
2.
Uterus didelphys is easier to diagnose, but the diagnosis of a septate uterus may be missed due to absence of changes in the uterine shape and contour. For this, a cross-sectional ultrasound observation may be particularly important to find whether there are two adjacent uterine endometrial echoes.
3.
Identification of bicornuate uterus and uterus didelphys: The former has two complete uterine horns at an acute angle, and sometimes the bladder can show a “V”-shaped indentation, while the latter has two full uterine bodies, in between which may commonly show intestinal echoes.
4.
Rudimentary horn may be misdiagnosed as a uterine fibroid or adnexal mass. The echo level should be carefully observed for presence of any uterine endometrial echoes. Rudimentary horn pregnancy is a dangerous problem which should attract great attention.
5.
Transvaginal ultrasound probe has a higher frequency. As it is also closer to the uterus, it is of better value to observe bicornuate uterus, rudimentary horn, septate uterus, and a number of complex uterine anomalies; an abdominal ultrasound can show a complete uterine shape and contour, so its observation on the shape of a bicornuate uterus will be more comprehensive. Therefore, a combination of both ultrasound approaches can improve the diagnostic accuracy of detecting uterine anomalies, and avoid unnecessary false-negative diagnosis or misdiagnosed.
2.2.2 Ultrasound Features of Congenital Oblique Vaginal Septum Syndrome
Oblique vaginal septum syndrome is a congenital genital anomaly including uterus didelphys, double cervix, and a septum attaching to the vaginal wall extending obliquely from one side of the cervix; this often affects the patency of the ipsilateral cervix. An oblique vaginal septum is often associated with ipsilateral renal agenesis.
The clinical manifestations include painful menarche, lower abdominal pain or discomfort, excessive vaginal discharge with smell, or prolonged menstrual periods. In recent years, ultrasound examination has become the diagnostic method of choice, because of its advantages of being accurate, fast, real time, and noninvasive. Ultrasound examination shows not only the uterus and the cervix but also their number and shape and retention of blood in the vagina and the adnexa. It also gives an accurate diagnosis of renal agenesis.
Get Clinical Tree app for offline access

Ultrasound Features
1.
The uterus didelphys (with or without, particularly at the right side with retention of blood clots): The cross-sectional scan shows a fused cervix, with two separate uterine echoes which can be symmetrical or of different sizes; uterine endometrial echoes can be seen from both uterine cavities, with one of the uterine cavities often accompanied by retention of fluid (Fig. 2.13a–e).