29 Systemic Lupus Erythematosus
Clinical Presentation
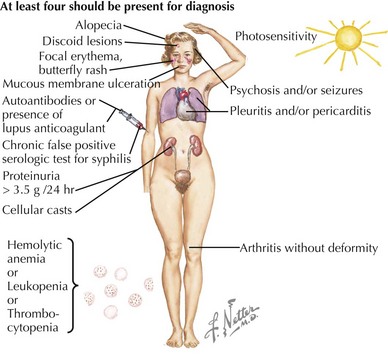
SLE is rare in children younger than age 5 years and is uncommon before adolescence. In childhood, girls are affected approximately four times more often than boys. The presenting symptoms are widely variable. Constitutional signs and symptoms, including fever, fatigue, lymphadenopathy, hepatosplenomegaly, and weight loss, are commonly seen. The most frequently involved specific sites affected by SLE are the skin, joints, and kidneys. Symptoms often precede the diagnosis by several months and may be insidious or acute in onset. The American College of Rheumatology provides criteria which are used clinically to aid in the diagnosis of SLE (Table 29-1, Figure 29-1). The diagnosis of SLE is made if at least four of the criteria are present or have been present in the past without another diagnosis that explains the findings. The antinuclear antibody (ANA), one of the criteria for diagnosis of SLE, is not a useful general screening test for rheumatologic disease and should not be sent routinely in the absence of other criteria for SLE.
Table 29-1 American College of Rheumatology 1997 Revised Classification Criteria for Systemic Lupus Erythematosus
| Criterion | Description |
|---|---|
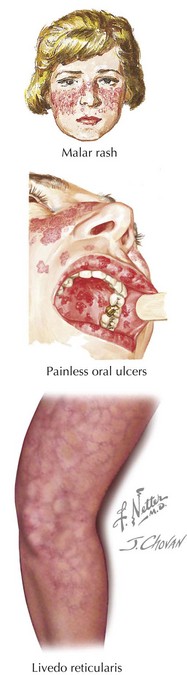
| Malar rash | “Butterfly” erythematous rash over malar eminences; spares nasolabial folds (see Figure 29-2) |
| Discoid rash | Raised erythematous patches with scaling and follicular plugging on the face, scalp, and extremities; may lead to scarring |
| Photosensitivity | Any rash that occurs as an unusual reaction to sunlight |
| Oral or nasal ulcerations | Painless ulcerations of the oral or nasal mucosa (see Figure 29-2) |
| Arthritis | Nonerosive arthritis of two or more peripheral joints |
| Nephritis | Persistent proteinuria >0.5 g/d or cellular casts (red blood cell, hemoglobin, granular, tubular, or mixed) |
| Serositis | Pleuritis or pericarditis |
| Neurologic disorder | Seizures or psychosis (in the absence of offending drugs or metabolic disturbances) |
| Cytopenia | Hemolytic anemia with reticulocytosis or leukopenia (<4000/mm3) or lymphopenia (<1500/mm3) or thrombocytopenia (<100,000/mm3) |
| Positive immunoserology | Antibodies to dsDNA or antibodies to Sm nuclear antigen or anticardiolipin antibodies or presence of lupus anticoagulant or false-positive serologic test for syphilis (known to be positive for ≥6 months and confirmed by Treponema pallidum immobilization or fluorescent treponemal antibody absorption test) |
| Positive antinuclear antibody | Abnormal titer of antinuclear antibodies at any point in time |
Adapted from Hochberg MC: Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725, 1997.
Skin and Mucus Membrane Manifestations
There are four skin and mucocutaneous criteria: malar rash, discoid rash, oral or nasal ulcers, and photosensitivity. The malar rash, or classic “butterfly rash,” is typically maculopapular and photosensitive. Additionally, it classically extends across the nasal bridge, spares the nasolabial folds, and is nonscarring (Figure 29-2). Depending on the race of the child, it may be either hyper- or hypopigmented. A discoid rash is less common. These inflammatory lesions are coin shaped, raised, and erythematous. They are most commonly located on the face (especially the ears), scalp, and extremities. These lesions are scarring and lead to permanent alopecia when they occur on the scalp. The oral and nasal ulcers associated with SLE are usually painless; oral ulcers are classically located on the hard palate (see Figure 29-2). Other common skin manifestations include livedo reticularis (see Figure 29-2), alopecia, Raynaud’s phenomenon (see Figure 27-2), and digital ulcerations.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree