48 Syncope
Etiology And Pathogenesis
Syncope occurs when cerebral blood flow decreases below 30% to 50% of baseline. This decrease may be the result of systemic vasodilation, decreased cardiac output, or both. This results in transient ischemia, causing temporary loss of consciousness and motor tone. Syncope may also be accompanied by brief autonomic movements. Syncope should be distinguished from presyncope (dizziness or lightheadedness without loss of consciousness), vertigo (the sensation of spinning), and syncopal-like events (e.g., seizures, migraines, or conversion disorder). The causes of syncope can be divided into three major categories: neurally mediated, cardiac, and metabolic (Box 48-1). Syncopal-like events are discussed briefly in the following section.
Box 48-1 Differential Diagnosis of Presentation for “Syncope”
Neurally Mediated Syncope
Cardiac Syncope
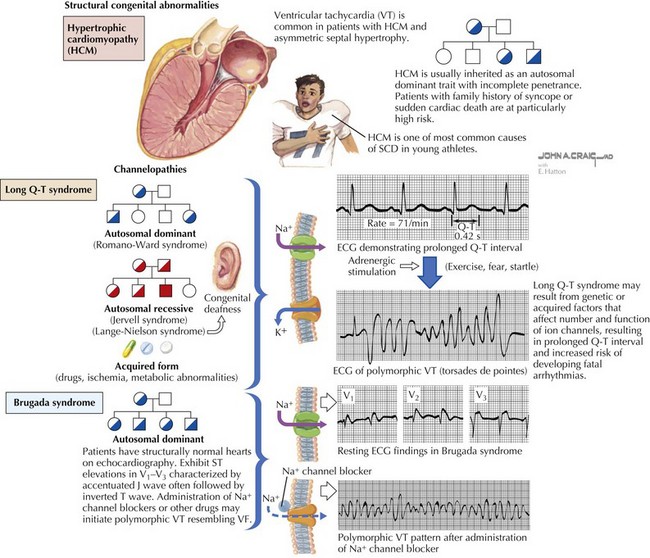
Although a cardiac cause is found in fewer than 2% of previously healthy children with syncope, it is important to recognize because it can be associated with an increased risk of sudden death. Cardiac syncope results from abrupt decline in cardiac output as the result of obstructive lesions (aortic stenosis, hypertrophic cardiomyopathy [HCM]), myocardial dysfunction (ischemia, cardiomyopathy), or primary arrhythmias (Figure 48-1). Many of these conditions can be asymptomatic until syncope or sudden death occurs. Arrhythmias can also occur secondary to structural heart disease, to myocardial dysfunction, or to postoperative changes in association with congenital heart disease. Any concern for a cardiac syncope warrants a referral to a pediatric cardiologist. Sudden cardiac death (SCD) in the young is estimated to affect between one in 50,000 and one in 200,000 children.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree