• CNS involvement (pontine micturition center) – afferent signal through spinothalamic tracts & dorsal columns → intensity of signal reaches threshold of consciousness triggering void when socially acceptable → efferent signal through reticulospinal & corticospinal tracts
PHYSIOLOGY AND MECHANISMS OF DEFECATION
Anatomy
• EAS – striated muscle innervated by hemorrhoidal branch of pudendal nerve, voluntary squeeze
• IAS – continuation of smooth circular muscle of rectum under autonomic control, constant contraction contributes 70–80% of resting anal tone
• Levator ani complex – defines prox border of anal canal – PR muscle – striated musc sling originating from pubic bone supporting the rectum, innervated via direct branches from S3, S4, & pudendal nerve, constant tone at rest creates the anorectal angle (~90∞)
Mechanism of Normal Defecation
• Rectum acts as reservoir → receptors in PR sense distention → IAS reflexively relaxes to sample contents & then contracts RAIR → voluntary relaxation of pelvic floor (PR) & EAS straightens anorectal angle by >15° & allows passage of contents
PELVIC ORGAN PROLAPSE (POP)
Definitions
• Loss of support of the anter, apical, or post compartments of the vagina that result in protrusion of pelvic organs into or out of the vaginal canal (bladder, rectum, small bowel, sigmoid, colon, or uterus/cervix).
• Anter: Cystocele: Prolapse of bladder into the vagina
• Apical: Uterine prolapse: Prolapse of uterus & cervix into the vagina or vaginal vault prolapse: Prolapse of the vaginal vault or cuff after hysterectomy
• Post: Rectocele: Prolapse of rectum into the vagina
Epidemiology (Obstet Gynecol 1997;89:501)
• Risk of POP requiring Surg by the age of 80 is ∼11%
• POP is the 3rd most common indication for hysterectomy following leiomyomata & endometriosis
Pathophysiology (Cochrane Database Syst Rev 2010;4:3)
• Risk factors – Preg, childbirth, congen or Acq connective tissue abnormalities, denervation or weakness of the pelvic floor, aging, hysterectomy, menopause & factors a/w chronically raised intra-abdominal pres, & race (Black & Asian w/ lowest risk, Hispanic w/ highest risk)
• 3 levels of support of the vagina (Am J Obstet Gynecol 1992;166:1717)
Level I: Apical & uterine support comprised of cardinal & uterosacral ligament attachment to the cervix & upper vagina → defects in this support complex may lead to apical prolapse
Level II: Lateral support of the vagina including paravaginal attachments (pubocervical fascia & arcus tendineus fasciae pelvis) contiguous w/ the cardinal/uterosacral complex at the ischial spine → defects in this support may lead to lateral, paravaginal, & anter wall prolapse
Level III: Support of distal 3rd of the vagina comprised of perineal body, superficial & deep perineal muscles, & fibromuscular connective tissue → defects in this support may lead to anter & post vaginal wall prolapse, gaping introitus, & perineal descent
Clinical Manifestations
• Assoc sx (Note: Many women may be asymptomatic):
Bulge, pelvic heaviness, backache, urinary incontinence, frequency or urgency, difficulty in initiating & maintaining urinary flow, incomplete emptying, sexual dysfxn, incontinence of stool or flatus, constip, or need for splinting
• Physical exam:
Perform a full physical exam to determine pathology outside of the pelvis
Vaginal exam:
Routine external & bimanual exam while in lithotomy position
Elicit bulbocavernosus reflex & anal wink reflex to determine if sacral pathways are nml
Ask the pt to Valsalva while gently spreading the labia to determine overall prolapse
Inspect each compartment of the vagina separately w/ the pt performing max Valsalva. Use 1 blade of the speculum to assist in visualizing the anter or post compartment individually. During assessment determine the location & degree of prolapse relative to the hymenal ring.
Perform a rectovaginal exam to assess post wall defects, enterocele, & determine anal sphincter strength
A PVR by catheterized specimen will help determine adequate emptying. Will also provide opportunity for urinalysis.
Pelvic Organ Prolapse Quantification (POP-Q)
• Provides an objective site-specific system for determining location & staging of POP w/ the hymen as the fixed point of reference
• Negative numbers indicate support above the hymen where a positive value indicates prolapse beyond the hymen
Figure 7.1 A (diagram on left): POP-Q. There are site points labeled Aa, Ba, C, D, Bp, and Ap that correspond to points above or below the hymenal remnants and are stated in centimeters above (negative) or below (positive) that point. The genital hiatus (gh), perineal body (pb), and total vaginal length (tvl) are also listed as lengths in centimeters. They are used to quantify pelvic organ support anatomy. B (grid on right): Grid for recording quantitative description of pelvic organ support (From Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 1996;175:10)

Stages of Prolapse
• Stage 0: No prolapse is demonstrated
• Stage I: Most dependent portion of prolapse is >1 cm above the hymen
• Stage II: Most dependent portion of prolapse is ≤1 cm prox or distal to the hymen
• Stage III: Most dependent portion of prolapse is >1 cm below the hymen but extends no further than 2 cm ≤TVL – 2 cm
• Stage IV: >TVL – 2 cm
Diagnostic Workup/Studies
• Physical exam is generally suff to determine type & stage of prolapse
• Urodynamic studies may be useful to determine occult urinary incontinence
Treatment: Nonsurgical Management
• Assurance & observation
• Pelvic floor muscle exercises (Kegel exercises)
Minimal risk & low cost, but no high-quality evid supporting prevention or rx of prolapse
• Pessary
Indications – poor operative candidate, desire to avoid Surg, used as diagnostic tool to determine if urinary incontinence resolves w/ restoration of anatomy
Continuation rate 50–80% after 1 y of use (Int Urogynecol J 2011;22:637)
Treatment: Surgical Management
• Apical support (uterine or vault prolapse):
Sacrocolpopexy: Mesh (typically polypropylene) suspension of the vagina or uterus to the anter longitudinal ligament of sacrum via abdominal, laparoscopic, or robotic-assisted approach
Risks: Mesh erosion 2–11% (Obstet Gynecol 2004;104:805), GI complications including SBO, other abdominal surgical complications, de novo stress incontinence, thus need to consider concomitant anti-incontinence procedure (NEJM 2006;354:1557)
Sacrocolpoperineopexy: Same technique as above, w/ addition of post arm of mesh extending to the perineal body
Uterosacral ligament suspension: Suspension of the vaginal cuff after hysterectomy to the bilateral uterosacral ligaments at the level of the ischial spines
Risks: Ureteral obst up to 11% (cystoscopy recommended)
Sacrospinous ligament fixation: Suspension of the vaginal apex to the sacrospinous ligament either unilaterally or bilaterally, typically using an extraperitoneal approach
Risks: Anter prolapse rate 6–28%, pudendal & inferior gluteal vessels & nerves lie behind the sacrospinous ligament & may be injured during procedure causing hemorrhage or postop gluteal pain
Iliococcygeal suspension: Attaches the vaginal apex to the fascia of the iliococcygeus muscles bilaterally
Risks: No randomized trials that support the use of this procedure & may shorten vagina
• Anter compartment defect:
Anter colporrhaphy: Midline plication of endopelvic fibromuscularis of the anter vagina w/ removal of excess vaginal mucosa, ± graft reinforcement
Benefits: Easy to perform
Risks: Only 50% anatomic cure
Paravaginal repair: Same as above w/ addition of lateral dissection to the arcus tendineus or obturator fascia w/ reinforcement sutures placed in these structures. Can be performed by laparoscopic, vaginal, or abdominal approaches.
• Post compartment defect:
Post colporrhaphy: Midline plication of the rectovaginal fibromuscularis in the post vagina w/ removal of excess vaginal mucosa
Benefits: Cure rate is 76–96%
Risks: Excessive removal of vaginal mucosa can result in vaginal narrowing & dyspareunia, 25% rate of postsurgical dyspareunia alone
Site-specific repair: Identification of isolated defects in the rectovaginal fibromuscularis & subseq repair
• Obliterative procedures in nonsexually active individuals:
Complete colpocleisis – removal of vaginal epithelium w/ suturing of the anter & post vaginal walls together, thus obliterating the vaginal lumen & effectively closing the vagina.
LeFort colpocleisis – partial excision of the anter & post vagina w/ closure of the vaginal lumen distal to the cervix (uterus in situ), lateral tracts left patent to allow for egress of cervical & vaginal mucus or discharge
• Mesh augmentation & mesh kit procedures:
Biologic: Autologous (self), allograft (donor), or xenograft (porcine/bovine)
Synthetic: Types I–IV based on pore size, type I monofilament most used due to large pore size & decreased rates of infxn
Mesh kits: Various types of kits: There is an FDA warning about the increased risk of complications including mesh erosion, GI involvement, pain, & need for reoperation. ACOG recommends vaginal mesh be reserved for high-risk pts including those w/ recurrent prolapse &/or medical comorbidities precluding a lengthier Surg (Obstet Gynecol 2011;118:1459–1464).
URINARY INCONTINENCE
Definition
• Involuntary leakage of urine:
Stress urinary incontinence (SUI): Complaints of involuntary leakage of urine w/ cough, sneezing, or exertional maneuvers that ↑ abdominal pres
Urge urinary incontinence (UUI): Complaints of involuntary leakage of urine w/ sensation of urgency, often referred to as OAB
Mixed urinary incontinence (MUI): Combination of both SUI & UUI
Continuous urinary incontinence: Complaint of continuous leakage
Overflow incontinence: Complaint of involuntary loss of urine preceded by an inability to empty the bladder (a/w overdistention & urinary retention due to obst or neurologic causes)
Epidemiology
• Prevalence of 25–55% in Western countries
• May be as high as 50% in nursing home pts & 40% in postmenopausal women
• Many women will not address this issue w/ their physicians due to embarrassment. May lead to signif impairment in QOL
Etiology
• Age, childbearing, obesity, medical diagnoses (diabetes, stroke, spinal cord injury)
• Hysterectomy & menopause w/ inconsistent results
Pathophysiology (N Engl J Med 1985;313:800; Obstet Gynecol 2005;105:1533)
• Impairment in the physiologic voiding mech
• Functional incontinence – incontinence occurring b/c of factors unrelated to the physiologic voiding mech
Remember mnemonic DIAPPERS (Delirium, Infxn, Atrophic urethritis & vaginitis, Pharmacologic [diuretics, sedatives, anticholinergics, CCB, α blockers], Psychologic [depression], Endocrine [calcium, gluc], Restricted mobility, Stool impaction)
• Genitourinary etiologies include filling & storage disorders (SUI, UUI, MUI), fistulae (vesicovaginal, ureterovaginal, or urethrovaginal), congen (ectopic ureter, epispadias)
Clinical Manifestations
• Hx: Provides the most insight to cause, type, & rx. Include the following: Voiding frequency, noctural voiding frequency, number of episodes of incontinence & vol a/w episodes, number of pads used, bowel incontinence, bulge sx, diet (including caffeine & EtOH intake), medical & surgical hx, obstetrical & gynecologic hx, neurologic conditions (diabetes, multi sclerosis, disk dz, & stroke), pulm conditions, smoking, & meds
• Consider having the pt keep a voiding diary over 3–7 d
• Physical exam: Complete full physical exam including gynecologic, rectal, & genital/lower neurologic exam. Include POP-Q (see POP section)
• Urethral mobility: May be assessed w/ the Q-tip test & helps aid in the dx of stress incontinence
A Q-tip is placed in the urethra to the level of the vesical neck & assessment of the change of axis is performed while asking the pt to Valsalva.
An angle of >30° is indicative of urethral hypermobility
• Cough stress test
• PVR to determine if urinary retention an issue <50 mL adequate bladder emptying, >200 mL considered inadeq.
Initial Workup
• Lab test: Clean midstream or catheterized urine sample for urinalysis & culture prn. Bld testing including BUN, Cr, gluc, & calcium
Subsequent Workup
• Urodynamic testing: A test that evaluates stress incontinence, detrusor instability, 1st sensation, desire to void, bladder compliance, & bladder capacity
Recommended in the following circumstances: (1) dx unclear, (2) Surg being considered, (3) marked POP present which may have underlying de novo incontinence, or (4) a neurologic condition exists.
Measurements:
Uroflowmetry: Assesses ability to empty bladder, meter assesses flow rate
Filling cystometry: Measures detrusor fxn including sensation, compliance, capacity, & evid of uninhibited detrusor contractions Pres catheters are placed in the bladder & vagina or rectum while the bladder is retrofilled. Detrusor activity is determined by Pves (pres in bladder) – Pabd (pres in abd, measured by vaginal/rectal catheter). Individual measurements are recorded throughout the tracing including LPP, 1st desire & maximal bladder capacity → ISD – Valsalva LPP <60 cm H2O
Urethral pres profile: Evaluate for ISD, dual sensor catheter is used to determine MUCP & functional urethral length → ISD – MUCP is 20 cm H2O or less
• Cystourethroscopy: May be req for eval of microscopic hematuria, irritative voiding sx w/o evid of infxn & persistent hematuria in women >50 yo, or suspicion of suburethral mass
Treatment
• Behavioral approaches:
Lifestyle modification: Weight loss, caffeine, EtOH, or fluid intake reduction, decreased weight bearing, smoking cessation, & constip relief, “bladder diet”
Bladder training: May aid in UUI & MUI
Kegel exercises: Strengthen the voluntary periurethral & perivaginal muscles, may be augmented w/ biofeedback training or electrostimulation via a pelvic floor physical therapist
• Medical management:
Estrogen may ↑ urethral bld flow, α-adrenergic receptor sens, & build collagen but is not proven to help in incontinence & some trials suggest incontinence may be worsened
Antichol medication is often used for UUI or MUI
• Nonsurgical rx:
Incontinence pessary: Help w/ SUI during exercise-need fitting
Urethral plugs: Help w/ SUI during exercise-need fitting
• Surgical rx:
See sections under stress & detrusor instability
OVERACTIVE BLADDER AND URGE INCONTINENCE
Treatment
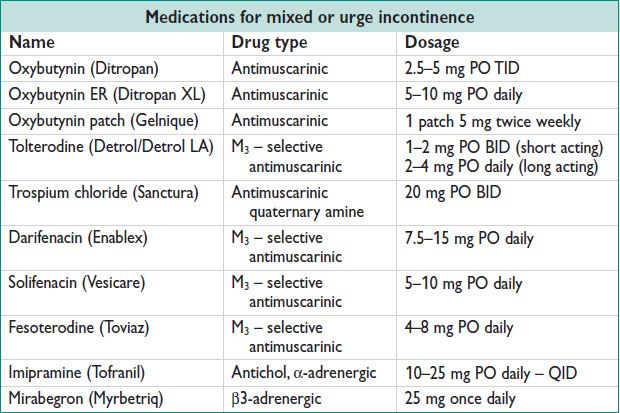
• Medical management generally involves antichol or antimuscarinic meds
Antichol may be best for MUI
Side effects of anticholinergics include dry mouth, constip, blurry vision (contraindicated in pts w/ narrow-angle glaucoma)
• Surgical management:
Used for refrac urge incontinence
Botulinum toxin type A (Botox) injection:
Act to inhibit periph cholinergic nerve endings by inhibiting ACh release from the presynaptic terminal. Intradetrusor injections typically done by cystoscopy prevent the detrusor muscle from being stimulated thus preventing bladder contractions
May cause postinjection urinary retention requiring self-catheterization
May have up to a 73% continence rate (Eur Urol 2004;45:510)
Sacral nerve stimulation:
Performed in two phases: (1) Percutaneous nerve eval to determine resp w/ placement of implantation electrode adj to the 3rd sacral nerve root. Trial of 3 w is typical to determine resp. (2) If >50% resp a permanent electrode is placed attached to a generator.
Up to 80% resp, but 30% removal or revision rate due to pain or complications at the implant or generator site (J Urol 1999;162:352)
STRESS INCONTINENCE
Treatment
• Medical management not generally useful
Pessary or urethral plugs can be attempted
• Surgical management:
Retropubic colposuspension (Burch & MMK):
Previously considered the gold std for SUI
Involves suspension of the pubocervical fibromuscularis to pubic symphysis periosteum (MMK) or Cooper’s ligament (Burch)
Retropubic sling:
Has largely replaced colposuspension & thought to be as effective
Objective cure rates 63–5% for the TVT procedure compared to Burch colposuspension 51–87% (AJOG 2004;190:324)
Polypropylene mesh (most common material) is placed under the midurethra w/ minimal tension through the retropubic space
Operative risks include bladder, ureteral, urethral, bowel or bld vessel injury thus mandating cystoscopy postplacement
Transobturator sling:
Directed bilaterally through the obturator foramen & underneath the midurethra
Compared to TVT w/ 80.8% cure rate TOT had a 77.7% objective cure rate. Voiding dysfxn was improved in the TOT group. Nerve & musc pain in the leg is more common in the TOT compared to TVT (NEJM 2010;362:2066)
Designed to reduce complications of retropubic trochar placement
Operative risks of bladder, ureteral, & bld vessel injuries are less than the retropubic sling approach; however, pts may experience more groin pain
Minislings (single-incision slings):
Newer slings which include 1 transvaginal incision & either placed into an H position or a U (retropubic position)
Facial bladder neck slings:
Utilizing fascia from the rectus muscle or elsewhere to perform a retropubic bladder neck sling → preserved for complicated cases
OVERFLOW INCONTINENCE
Definition and Etiology
• Involuntary loss of urine due to inability to adequately empty the bladder
AKA chronic retention of urine, neurogenic bladder
Neuromuscular disorders – interfere w/ nml bladder reflexes
Multi sclerosis, diabetic neuropathy, CNS trauma, CNS tumors, etc.
Obstructive disorders – urethral obst leads to retention & overdistension
POP, anti-incontinence procedures, malig, fecal impaction
Meds – anticholinergics, antimuscarinics
Clinical Manifestations
• Inability to void or fully empty bladder voluntarily
• Loss of small amounts of urine w/o sensation of emptying
• Medication hx important to exclude causes of urinary retention
Physical Exam and Workup/Studies
• Nonpainful bladder that is palpable after voiding
• Signif PVR (typically >300 mL)
• Urodynamics
Treatment
• Therapy directed at treating the underlying cause
• CIC or indwelling catheter to ↓ overdistention
• Sacral nerve stimulation – see OAB section, above
• α blockers are not FDA approved for use in women, but have been useful in BPH in males
BYPASS INCONTINENCE AND UROGENITAL FISTULAE
Definition and Etiology
• Leakage of urine from extraurethral sources
AKA extraurethral incontinence
Urogenital fistulae –VVF, ureterovaginal fistula: Most common cause in developed countries is gynecologic Surg (0.1% of all hysterectomies), other causes include radiation, trauma, malig, complications of parturition. Most common cause in developing countries is obstetric trauma (pres necrosis)
Ectopic ureter
Urethral diverticulum
Clinical Manifestations
• Continuous leakage of urine common in urogenital fistula
• Pts w/ urethral diverticula may complain of pre- or postvoid “dribbling”
• May present with recurrent UTIs, vaginal candidiasis, perineal irritation
Diagnostic Workup/Studies (Female Pelvic Med Reconstr Surg 2012;18:71)
• Urinalysis, urine culture
• Voiding cystourethrogram – 1st-line imaging
• Cystourethroscopy – helpful to determine location in bladder
• Intravenous pyelogram may be performed if there is a suspicion for ureteral fistula
• CT/MRI may be used to further characterize size & location
Treatment
• Surgical rx to correct the anatomic abnormality
• May consider conservative management of small VVF w/ prolonged bladder drainage
• Genitourinary fistulas can be repaired vaginally, laparoscopically, or abdominally depending on size, location, & surgeon skill set
Vaginal repair preferred for uncomp VVF
Latzko procedure – partial colpocleisis w/o excision of fistulous tract
Layered closure – surrounding tissues mobilized, fistulous tract excised, multi layers closed w/ absorbable interrupted sutures
Martius flap – transposition of labial fat pad, useful for large VVF w/o adequate vaginal tissue
Abdominal or laparoscopic repair may be needed for prox, complex VVF & ureterovaginal fistulae
INTERSTITIAL CYSTITIS
Definition
• Syn characterized by chronic pelvic pain, urinary urgency & frequency, dyspareunia, nocturia
Epidemiology
• Prevalence 10–67/100000 women in US (Obstet Gynecol 2002;100:337)
• Up to ~40% women w/ chronic pelvic pain
Pathophysiology
• Poorly understood, potential theories include mast cell activation, upregulation of sensory nerves, altered bladder wall permeability
Diagnostic Workup/Studies
• Rule out UTI & other causes of chronic pelvic pain
• Bladder diary may show frequent small voids
• Cystourethroscopy w/ hydrodistention ± bx
• Bladder filled to near capacity, emptied, & then inspected for petechial hemorrhages, Hunner ulcers (diagnostic), glomerulations (not diagnostic)
• Potassium sens test – instillation of nml saline into bladder followed by KCl solution, positive if pain present w/ KCl instillation (low spec)
Treatment
• Avoidance of spicy foods, coffee, tea, carbonated beverages, tomatoes
• Hydrodistention can improve sx by 20–30%
• DMSO bladder instillation – anti-inflammatory, bladder anesthetic, decreases mast cell activation, relaxes muscle
• Pentosan polysulfate sodium – heparin analog, 100 mg PO TID, only FDA approved oral drug for IC
• Tricyclic antidepressants – inhibit pain fiber activation, amitriptyline 10–75 mg nightly has shown improv in 2/3 of women
ANAL INCONTINENCE
Definition and Epidemiology
• Involuntary passage of flatus or stool
• Fecal incontinence – inability to prevent passage of stool until socially acceptable
• Prevalence 2–17% general pop, up to 50% of nursing home residents (NEJM 2007;356:1648)
• Risk factors: Female sex, pelvic radiation, obstetric trauma, neurologic d/o, prev anorectal Surg, chronic diarrhea (IBD, IBS, celiac sprue), fecal impaction, urinary incontinence, nursing home placement, smoking, obesity
Etiology
• Chronic constip is very common in women & can lead to overflow incontinence & pelvic floor dysfxn if untreated
• Etiology is commonly multifactorial
• Most common cause in otherwise healthy women is damage to anal sphincter at time of vaginal deliv
• Pseudoincontinence – fecal soiling only (rectovaginal fistula, external hemorrhoids, incomplete rectal emptying)
Clinical Manifestations
• Direct questioning or written questionnaires are important
• Detailed hx including onset, frequency, severity, consistency of stool, presence of bld, pus, or mucus, pad use, effect on QOL, bloating, fecal urgency, straining, insensible loss of stool, fecal soiling
• Thorough medication hx important (laxatives, meds causing constip [anticholinergics, iron, narcotics, etc.] can lead to overflow incontinence)
Physical Exam
• Inspection of perineum & anus – external hemorrhoids, dermatitis, nml perineal skin creases, rectal prolapse, scars from prev lacerations or episiotomies, patulous anus (indicative of denervation), fissures
• Dovetail sign – loss of anter perineal creases (disruption of EAS)
• Inspection w/ squeeze to evaluate symmetry of folds & mvmt of perineum
• Inspection w/ bearing down to evaluate excessive perineal descent (>3 cm)
• Perineal sensation – dull & pinprick sensation should be tested in S2–4 dermatomes
• Bulbocavernosus reflex – cotton swab touched over bulbocavernosus muscles should elicit contraction of EAS
• Digital rectal exam – evaluates resting tone, contraction of EAS & PR, areas of tenderness, fecal impaction, masses
Diagnostic Workup/Studies
• Daily stool diary, validated questionnaires
• Rule out systemic & metabolic causes (infectious, autoimmune, malig, endocrine)
• Colonoscopy: Indicated for any pt >50 yo or w/ concerning sx (weight loss, melena/hematochezia, chronic diarrhea), family h/o colon cancer, HNPCC or Lynch syn, evaluate for IBD, celiac sprue
• Endoanal US: Useful when there is clinical suspicion for anal sphincter injury, evaluates structure only (best 1st-line test for poor anal squeeze)
• Anal manometry: Useful study in pts w/ nml anal tone who reports abn sensation to defecate, evaluates rectal sensation, compliance, & RAIR, evaluates fxn only
• Other studies: Electromyography (mapping EAS defects), pudendal nerve conduction studies, defecography (evaluates perineal descent, anorectal angle, rectocele, etc.), dynamic pelvic MRI, colonic transit studies
Treatment (NEJM 2007;356:1648)
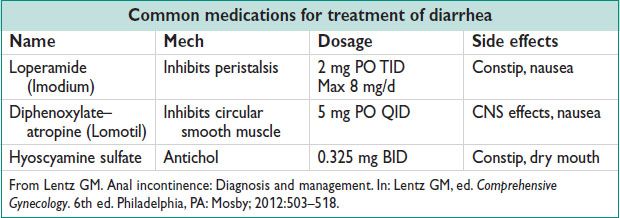
• Management directed at primary cause
• Behavioral modifications
Pelvic floor exercises (Kegel)
Biofeedback: Improves perception of rectal sensation & sphincter contraction
• Medical management
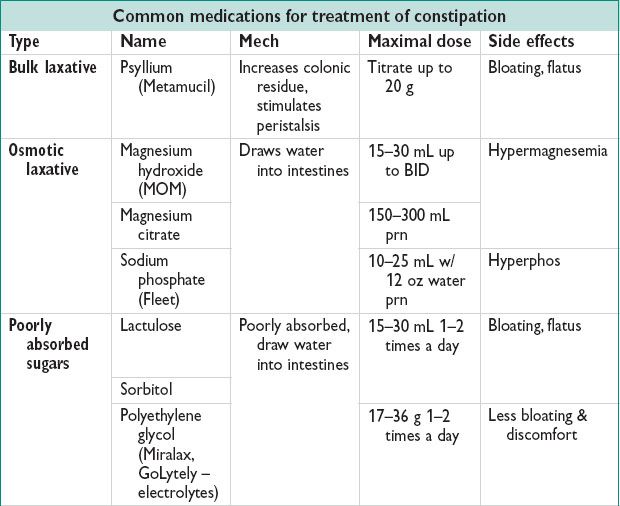
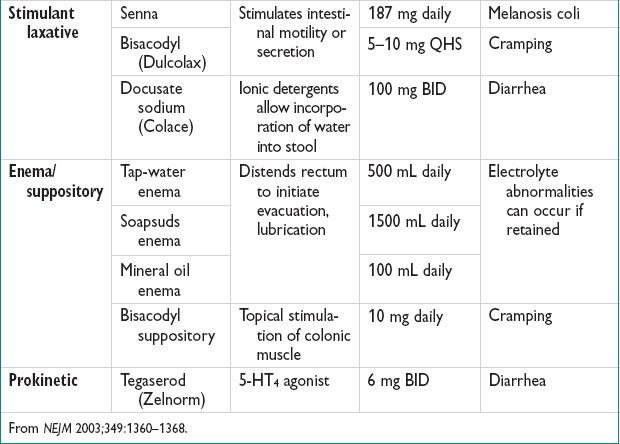
• Modification of stool consistency & deliv
Increased fiber intake increases solid stool bulk & may facilitate emptying (may worsen diarrhea in some pts) (Gastroenterology 1980;79:1272)
• Surgical management:
Generally surgical rx is the last resort & usually not effective
Overlapping anal sphincteroplasty – 85% short-term improv, 50% at 5 y
Note: Studies have not shown a difference in outcomes btw end-to-end vs. overlapping sphincteroplasty for perineal laceration repair after vaginal delive
Rectal prolapse repair – transrectal, transabdominal, or laparoscopic rectopexy
Sacral nerve stimulation – see OAB section, above, 37–74% continence rate at 24 mo (NEJM 1993;329:1905)
< div class='tao-gold-member'>



