79 Stroke
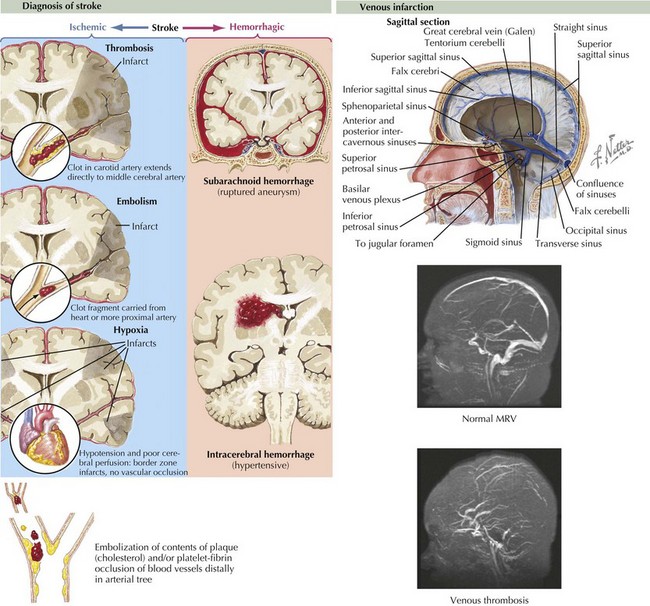
Stroke refers to acute vascular events involving the brain or brainstem. Childhood stroke occurs at a rate approximating that of childhood brain tumors. It is among the top 10 causes of death in children and is a significant cause of morbidity among survivors. Pediatric stroke can be subdivided into perinatal stroke, occurring from 28 weeks of gestation to 1 month of age, and childhood stroke, occurring from 1 month to 18 years. Important subtypes of stroke include arterial ischemic stroke (AIS), watershed infarction, intracerebral hemorrhage (ICH), and cerebral sinus venous thrombosis (CSVT). AIS is usually defined as an acute neurologic deficit of any duration consistent with focal brain ischemia conforming to an arterial distribution. Transient ischemic attacks (TIAs) are defined as focal deficits in a vascular territory lasting less than 24 hours, with some authors including the caveat that there must be no magnetic resonance imaging (MRI) evidence of infarction (Figure 79-1).
Etiology and Pathogenesis
Unlike adults, in whom hypertension, diabetes, and atherosclerosis predominate as risk factors for ischemic stroke, children presenting with AIS have much more varied etiologies. Approximately 50% of children presenting with stroke have an obvious underlying cause at the time of presentation, with arteriopathy, congenital heart disease, and sickle cell anemia representing some of the most common causes. In an additional 20% to 40%, an underlying cause can be found with further investigation. Somewhere between 10% and 30% are cryptogenic. Factors associated with pediatric AIS include inherited or acquired prothrombotic states, cardiac disease, arteriopathies or vasculopathies, trauma, and infections (Box 79-1). In older teenagers, traditional risk factors for adults, such as hypertension, diabetes, high cholesterol, and smoking, may also play a role. Cocaine or sympathomimetic medications are additional risk factors. Watershed strokes can be seen after cardiac arrest or other causes of shock, near drowning, and cardiac surgery.
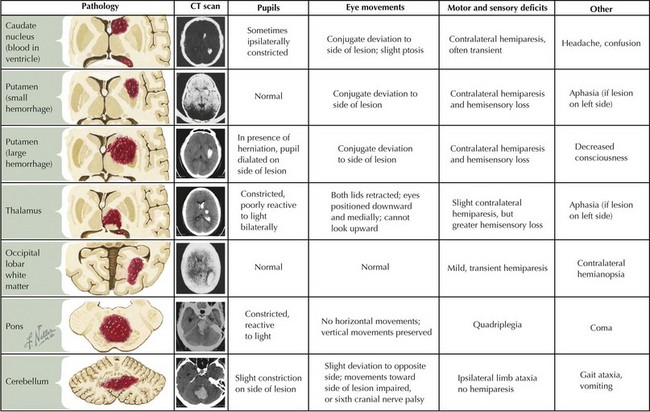
ICH in children is also etiologically distinct from ICH in adults. Unlike adults, in whom hypertension and amyloid angiopathy are the most common causes, childhood ICH is most commonly caused by ruptured vascular malformations (e.g., arteriovenous malformations, cavernomas, and aneurysms), hematologic abnormalities, and brain tumors (Box 79-2 and Figure 79-2).
Clinical Presentation
Intraparenchymal hemorrhage classically presents with focal neurologic signs or seizures accompanied by severe headache, emesis, and loss of consciousness but may be impossible to distinguish from AIS based on clinical features alone because presentations vary (see Figure 79-2). Children with CSVT may present acutely with headaches, emesis, seizures, altered mental status, or focal neurologic signs but can also present more insidiously with symptoms of increased ICP such as chronic headache, blurry vision, or diplopia secondary to sixth cranial nerve palsies.