STOMACH
Low hemoglobin makes oxygen transport to tissue impossible. The heart cannot distinguish between hypoxia, stenosis, carbon monoxide poisoning, and anemia. All are “felt” by the heart as decreased oxygen delivery to tissues.
What is the best next step in the management of this patient?
a. Intravenous (IV) normal saline bolus
b. Wait for hematocrit (Hct)
c. Upper endoscopy
d. Abdominal ultrasonography
e. IV omeprazole
Answer a. Intravenous (IV) normal saline bolus
The most critical part of the initial evaluation of any patient who presents with upper GI bleeding is to assess blood volume replacement and the airway. This patient has no evidence of breathing difficulty but does demonstrate significant circulatory compromise in the form of hemorrhagic shock. The evidence for this is tachycardia, hypotension, and orthostatic hypotension. This patient should immediately have two large-bore IV lines placed and receive normal saline boluses followed by PRBCs. Waiting for the Hct could prove fatal. The first hematocrit is nearly useless if it is normal because it will take hours to see what the real hematocrit is. Volume resuscitation must be done immediately as based on vital signs. This patient has likely lost 35% of his blood volume. You must lose 15% to 20% to become orthostatic. The patient has a pulse higher than 100 beats/min and systolic blood pressure less than 100 mm Hg, which means a 30% volume loss. Starting IV omeprazole is appropriate but is not the best next step in management because hemodynamic stability trumps all other choices. The patient is not stable enough for upper endoscopy, and ultrasonography has no role in upper GI bleeding.
What is the demarcation point between upper and lower GI bleeding?
a. Esophagus
b. Stomach
c. First and second parts of duodenum
d. Ligament of Treitz
Answer d. Ligament of Treitz
Upper GI bleeding is defined as any bleeding that occurs proximal to ligament of Treitz, which delineates the crossover point between the duodenum and jejunum.
Systolic blood pressure <100 mm Hg and heart rate >100 beats/min = ≥30% blood volume loss.
“Orthostatic” means a systolic blood pressure drop of 20 mm Hg and diastolic drop of 10 mm Hg or heart rate increase of 10 beats/min.
It’s all in the stool!
• Red blood demonstrates lower GI bleeding or very high-volume upper GI bleeding
• Coffee-ground emesis: 5 to 10 mL of blood loss proximal to the ligament of Treitz
• Black stool: upper GI bleeding from 100 mL of blood loss
• Heme-positive stool: brown from 5 to 10 mL of blood loss
High BUN with GI bleeding = Renal hypoperfusion + Blood in gut = High BUN
Which is a mechanism of high BUN-to-creatinine ratio in prerenal azotemia from decreased renal perfusion?
a. Increased filtration of protein at the glomerulus
b. Decrease in antidiuretic hormone (ADH) effect at the proximal tubule
c. Afferent arteriolar dilation
d. ADH increases urea reabsorption at the collecting duct
Answer d. ADH increases urea reabsorption at the collecting duct
ADH places aquaporins into the collecting duct at the kidney. This increases water reabsorption from the collecting duct and into the renal medullary interstitium. This would dilute the concentrating ability of the kidney. ADH also puts “urea transporters” directly into the collecting duct and causes direct urea reabsorption in the collecting duct.
Hct <30 + Old = PRBCs
Hct <25 + Young = PRBCs
International normalized ratio (INR) >1.5 = fresh-frozen plasma (FFP) and vitamin K
Platelets <50,000 with active bleeding = transfuse
What is best next step in the management of this patient?
a. Endoscopy
b. Angiography
c. Bleeding scan
d. IV omeprazole
e. IV ranitidine
Answer d. IV omeprazole
IV proton pump inhibitor (PPI) therapy is the best next step in management and should be initiated in all patients with suspected upper GI bleeding before endoscopy as part of the initial set of orders. PPI therapy has been shown to reduce rebleeding, downgrade the severity of the lesions, and promote healing of the stomach lining caused by increased pH. PPI therapy also promotes clot stabilization and therefore improves outcomes. Endoscopy should be done concurrently, but PPIs are tried first. Angiography is only for failed endoscopic hemostatic control with endoscopy, and the bleeding is massive. Bleeding scans are only for lower GI bleeds when you think there is blood loss likely happening but you do not know for sure. Nuclear bleeding scans are quite nonspecific. Ranitidine does not adequately raise stomach PH above 4 and is not nearly as useful in upper GI bleeding as a PPI.
H2 blockers (eg, ranitidine)
• Do not raise stomach PH adequately
Tachyphylaxis
• IV H2 therapy does not reduce morality rates but only promotes healing of the ulcers.
Three stimulants of acid/H+ from gastric parietal cells:
• Histamine
• Acetylcholine/vagal stimulation
• Gastrin
What is the best next step in the management of this patient?
a. Endoscopy
b. Angiography
c. Surgery
d. Nasogastric tube
Answer a. Endoscopy
After adequate volume resuscitation, correcting for anemia, and coagulopathy, the best next step is upper endoscopy known as esophagogastroduodenoscopy (EGD). EGD allows for diagnosis and intervention of the bleeding site. Endoscopy is the best initial diagnostic and therapeutic procedure. A nasogastric tube is wrong because it does not change management. If you are going to do an upper endoscopy, placing a nasogastric tube does not matter. There is nothing you can do therapeutically through a nasogastric tube. Lavage or decompression is not meaningful.
PPI + Endoscopy: All patients
Nuclear (technetium) bleeding scan: suspected GI bleed; source not found with scope
Angiography: localizes source of bleeding to guide surgery
• Peptic ulcer: secondary to Helicobacter pylori or nonsteroidal antiinflammatory drug abuse
• Variceal bleeding: cirrhosis
• Mallory Weiss tear: preceded by forceful vomitus
• Arteriovenous malformation: seen commonly in aortic stenosis
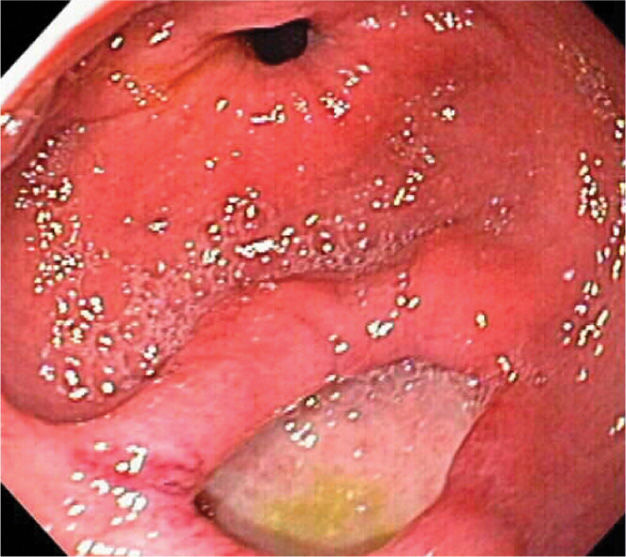
Figure 8-1. Gastric antral ulcer. (Reproduced, with permission, from Wong Kee Song L, Topazian M. Gastrointestinal endoscopy. In: Longo DL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.)
H. pylori
• Microaerophilic helix shaped
• Gram-negative bacterium
• Produces oxidase, catalase, and urease
Smoking and alcohol only impair ulcer healing. They do not cause ulcers.
Forrest classification of endoscopic findings. As you progress down the list, the rate of rebleeding decreases.
• Class Ia: Spurting hemorrhage
• Class Ib: Oozing hemorrhage
• Class IIa: Nonbleeding visible vessel
• Class IIb: Adherent clot
• Class IIc: Flat pigmented spot
• Class III: Clean ulcer base
GI bleeding stops spontaneously in 80% of patients.
What is the best next step in the management of this patient?
a. Endoscopy
b. Angiography
c. Surgery
Answer b. Angiography
After a failed endoscopy, the best next step to control bleeding is angiography with coil embolization of the vessel. Success rates for patients with acute peptic ulcer bleeding can reach 98%, with recurrent bleeding rates up to 20%. Patients should have a serum creatinine less than 1.5 mg/dL and an INR less than 1.5 and a platelet count greater than 50,000.
Nasogastric tube
• No therapeutic role
• Will not stop the bleeding
What is the best next step in the management of this patient?
a. Endoscopy
b. Angiography
c. Surgery
d. Add an H2 blocker to the PPI
e. Add sucralfate to the PPI
Answer c. Surgery
Surgery is the best next step in the management of complicated peptic ulcer disease (PUD) with persistent or massive recurrent GI bleeding. Additionally, if a patient presents with hemodynamic instability despite vigorous resuscitation, or shock with recurrent hemorrhage, surgery is indicated. Surgical treatments for PUD include oversewing of the artery with truncal vagotomy, or antrectomy with gastrojejunostomy (Billroth II procedure).



