Chapter 89 Status Epilepticus (Case 47)
Patient Care
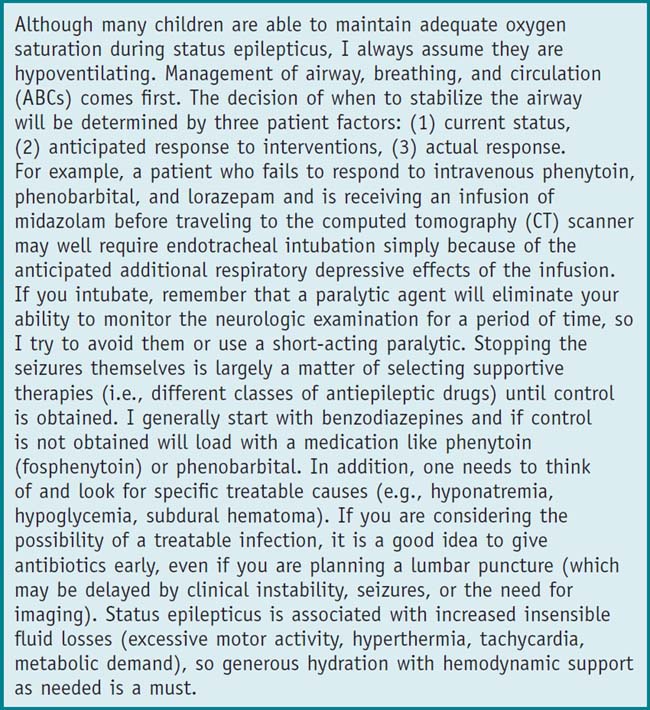
Clinical Thinking
• The longer the patient seizes, the more dangerous it becomes to the brain. Use agents with the most rapid onset first. The rectal, intranasal, or intramuscular route may be your first choice if the patient does not yet have an IV or intraosseous (IO) line.
History
• If febrile, is this a simple febrile seizure or a CNS infection? Fevers also lower seizure thresholds in children with epilepsy.
• Trauma can either be the causative agent of seizures or occur as a direct result (e.g., the child who collapses and hits her head).
Physical Examination
• Vital signs: Most actively seizing children are tachycardic and hypertensive, with irregular and/or ineffective respirations.
• Look for stigmata of an underlying neurodevelopmental disorder (e.g., microcephaly, contractures, dysmorphic features).
Tests for Consideration
• Electrolytes: Hyponatremia, hypocalcemia, and hypomagnesemia are all treatable causes of seizures $115
Imaging Considerations
→ Head CT: To rule out mass lesions $1000
→ Magnetic resonance imaging (MRI): To delineate small structural abnormalities $1800
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree