CHAPTER 23 Sporadic and recurrent miscarriage
Introduction and Definitions
Threatened miscarriage is defined as uterine bleeding prior to 24 weeks of pregnancy. Inevitable miscarriage can be subdivided into complete or incomplete, depending on whether or not all fetal and placental tissues have been expelled from the uterus. Early embryonic or fetal demise is where failure of the pregnancy is identified before expulsion of the fetal and placental tissues (usually by repeated ultrasound examination). Recurrent miscarriage is defined as three or more consecutive miscarriages (Stirrat 1990). This can be further subdivided into primary recurrent miscarriage, where there have been no previous live births, and secondary recurrent miscarriage, where at least one successful pregnancy has occurred previously.
Sporadic Miscarriage
Epidemiology
Problems of definition and ascertainment
Problems of definition arise very early in pregnancy, where reliable detection of pregnancy is only possible with biochemical testing using urinary or serum β-human chorionic gonadotrophin (β-hCG), and also in late pregnancy, where the distinction between a late mid-trimester miscarriage and a stillbirth can be difficult (Chard 1991). The ideal research model for determining rates of miscarriage is a prospective longitudinal study of a representative cross-section of the population which is capable of recognizing all conceptions immediately, takes account of termination of pregnancy and follows women through the first 20 weeks of pregnancy (Regan et al 1989, Alberman 1992).
Early histological work from the 1950s (Hertig et al 1959), in which fertilized ova were directly observed in 107 hysterectomy specimens from women who had intercourse around the time of expected ovulation prior to their operation, suggests a postimplantation pregnancy rate of 58% (21 of 36 possible conceptions). In a mathematical model, total pregnancy loss rates have been estimated at 78% (Roberts and Lowe 1975).
Rate of miscarriage
Following critical review of the literature, a reasonably coherent picture is emerging (Figure 23.1). Estimates of early reproductive loss rates in the peri-implantation period of approximately 50–70% still rest largely on the early work of Hertig, although data derived from in-vitro fertilization (IVF) studies support losses of this order of magnitude (Chard 1991).
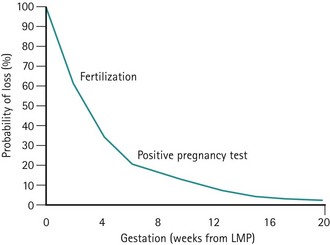
Figure 23.1 Fetal loss by gestational age.
Adapted from Kline J, Stein Z, Susser M 1989 Conception to birth — epidemiology of prenatal development. In: Kline J (ed) Monographs in Epidemiology and Biostatistics, Vol. 14. Oxford University Press, Oxford.
Postimplantation and biochemical pregnancy loss rates appear to be of the order of 30%, whereas recognized pregnancy losses after clinical recognition of pregnancy remain consistent in most studies as 10–15% (Table 23.1).
Table 23.1 Preclinical and clinical miscarriage rates
| Authors | Preclinical loss rate (%) | Clinical loss rate (%) |
|---|---|---|
| French and Bierman (1962) | – | 22 |
| Miller et al (1980) | 33 | 14 |
| Edmonds et al (1982) | 58 | 12 |
| Wilcox et al (1988) | 22 | 12 |
| Regan et al (1989) | – | 12 |
| Brambati (1990) | – | 14 |
| Nybo Andersen et al (2000) | – | 13 |
Aetiology
Chromosomal abnormalities
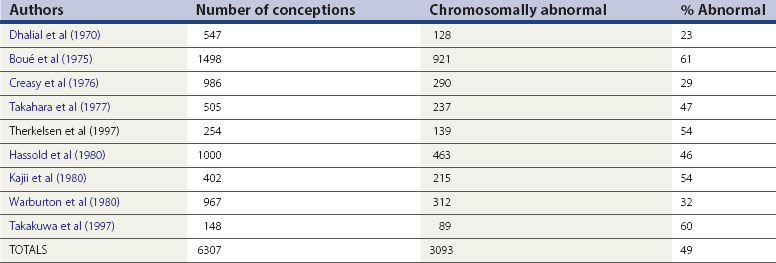
Miscarriage is a heterogeneous condition, but the single largest cause of sporadic miscarriage is fetal chromosomal abnormalities, accounting for approximately 50% of all cases (Table 23.2).
It is difficult to establish the precise contribution made by fetal chromosomal abnormalities. The figures in Table 23.2 are probably an underestimate, since miscarriages occurring as a result of fetal chromosomal anomalies are maximal at the earliest and least well-documented stages of pregnancy. Evidence from preimplantation genetic diagnosis studies of embryos created as a result of IVF suggests that at least 65% of all embryos are chromosomally abnormal (Gianaroli et al 2000). However, extrapolation of these results to miscarriage in the general population must be cautious, given the high degree of selectivity of these patients and a different microenvironment at fertilization.
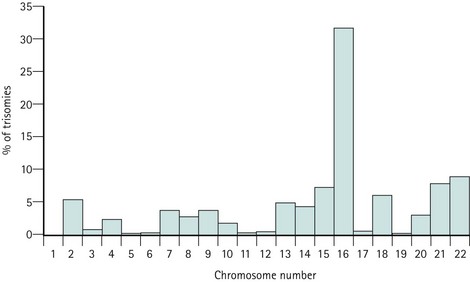
Trisomies for all chromosomes have been described, with the exception of chromosomes 1 and Y, although the relative frequencies are vastly different. Chromosome 16 and, to a lesser extent, chromosomes 2, 13, 15, 18, 21 and 22, account for the majority of trisomic abnormalities (Figure 23.2). Most trisomies are believed to be a consequence of non-disjunction during maternal meiosis. Trisomy 16 gives rise to only the most rudimentary embryonic growth with an empty sac (Edmonds 1992), and other trisomies often result in early embryonic demise.
Monosomy X (45XO) is thought to result from paternal sex chromosome loss (which can be either X or Y). It is usually associated with the presence of a fetus, although focal abnormalities, such as encephalocoele or hygromata, may occur (Edmonds 1992).
There appears to be a difference in the gestational age of pregnancy loss between different types of chromosomal abnormality, with trisomic and monosomic pregnancies miscarrying at a modal peak of 9 weeks and triploid pregnancy losses spanning 5–16 weeks of gestation (Alberman 1992).
Fetal malformations other than those caused by chromosomal anomaly
There is little doubt that the risk of miscarriage is increased with fetal malformation (Alberman 1992). However, since there has been no systematic search for malformations in fetal loss and since, in some cases, the malformation is secondary to a chromosomal anomaly, it is very difficult to assess the size of the increased risk. A single published study (Shephard et al 1989) has demonstrated an increased neural tube defect rate (3.6%) and an increased facial cleft rate (2.7%) amongst spontaneous miscarriages. Overall, the proportion of miscarriages as a result of fetal abnormalities without any associated chromosomal anomaly is small.
Placental abnormalities
Histological analysis of placental tissue from sporadic miscarriages has revealed several different patterns (Rushton 1995). These either point towards early fetal or embryonic demise with essentially normal placentation, or they have shown abnormal placental villous development with marked villous hypoplasia, reduced vascularization, enlarged intravillous spaces, often with clots and lacking significant extravillous trophoblastic infiltration, or with acute necrotic changes in the villi and associated clots which can be either patchy or global. Other reported placental changes have included inflammatory changes or a mixture of the above changes.
Amongst sporadic miscarriages, abnormalities of villous development have been reported fairly consistently at 30–40% (Hustin and Jauniaux 1997). However, the causes leading to the majority of these cases of abnormal placentation and therefore subsequent miscarriage remain unknown. Although autoimmune and infective causes can be associated with abnormal villous development, most inherently abnormal embryos probably also have abnormal placentation.
Infection
Infection has been cited as a cause of late pregnancy loss and also early pregnancy loss for the past century. However, the precise role of infection as a cause of sporadic miscarriage is poorly and inconsistently reported (Simpson et al 1996). In many cases, whether infection has actually preceded any fetal demise or merely arose afterwards remains satisfactorily unanswered.
Several organisms have been associated with miscarriage (Box 23.1). Listeria, toxoplasmosis, herpes varicella zoster and malaria (Plasmodium falciparum) appear to be the most clinically important pathogens in women with early miscarriage.
Rubella infection, although a cause of first-trimester miscarriage, is now rare. The role of cytomegalovirus is unclear, although primary infection may cause miscarriage. The role of chlamydia infection, whether via an acute primary infection or a resultant chronic endometritis, also remains unclear. An association between herpes simplex virus infection and early pregnancy loss was first reported in the 1970s (Nahmias et al 1971), although later prospective studies have failed to show any association with sporadic or recurrent miscarriage even when primary infection occurred in the first trimester (Stray-Pedersen 1993). It remains unknown whether human immunodeficiency virus (HIV) is an important cause of early pregnancy loss. Some studies have demonstrated an increased rate of early pregnancy loss with HIV (d’Ubaldo et al 1998), while others have not (Bakas et al 1996). Whether any increased risk of miscarriage is the result of the virus, the mother’s general health or her immunocompromised status remains unclear.
Syphilis (Treponema pallidum) and parvovirus B19 are more commonly a cause of late second-trimester miscarriage and stillbirth, whilst group B streptococcus has been implicated in late miscarriage and preterm labour. Bacterial vaginosis (Trichomonas vaginalis) is also associated with late second-trimester miscarriage and preterm labour, but the use of metronidazole or other antibiotics in women with demonstrable bacterial vaginosis infection does not reduce late miscarriage or preterm delivery rates (Carey et al 2000).
Fetal sex, multiple pregnancy, maternal age and parity
Most studies have reported an excess of males in miscarriages and pregnancies complicated by varying degrees of placental dysfunction (Kellokumpu-Lethtinen and Pelliniemi 1984, Edwards et al 2000). However, the sex ratio of most early conceptions still remains unknown.
Multiple pregnancy is associated with an increased risk of fetal loss, either via early resorption, postimplantation loss or second-trimester miscarriage. In early pregnancy, the risk of miscarriage is twice that of singleton pregnancies (Sebire et al 1997a). The rate of late pregnancy loss is also increased, particularly in monochorionic twin pregnancies, where late miscarriage rates can approach 12% (Sebire et al 1997b).
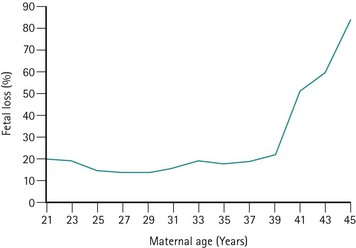
The risk of miscarriage rises with parity; however, the rise is a result of reproductive compensation (Alberman 1987). The risk of miscarriage in first pregnancies is low in young women (Regan et al 1989), but rises significantly after the age of 39 years (Figure 23.3). This rise is not only found in association with trisomic pregnancies (which rise with maternal age) but also in chromosomally normal pregnancies.
Maternal health
Virtually every maternal medical disorder has been associated with sporadic miscarriage. Women with severe medical disease rarely become pregnant, but if they do, their disease may deteriorate during pregnancy. Various mechanisms, including endocrinological, immunological or infective, have been suggested. Poorly controlled diabetes is associated with an increased risk of miscarriage (Mills et al 1988), whereas well-controlled and subclinical diabetes can rarely be considered a cause. Overall, only a small fraction of all early pregnancy losses can be considered to be attributable to severe maternal disease.
Cigarette smoking has been positively correlated with miscarriage, and a review of the effects of nicotine on ovarian, uterine and placental function suggests that cigarette smoking has an adverse effect on trophoblast invasion (Schiverick and Salafia 1999). Cocaine use has also been reported to increase the risk of miscarriage (Ness et al 1999). Alcohol consumption has been shown to be higher in women whose pregnancies ended in miscarriage compared with pregnancies which proceeded beyond 28 weeks of gestation (Harlap and Shapiro 1980, Kline et al 1980), although other studies have not confirmed this observation (Halmesmäki et al 1989, Parazzini et al 1990). There is some evidence to suggest that even moderate maternal alcohol consumption is associated with an increased risk of miscarriage (Windham et al 1997). Many studies have shown a relationship between coffee/caffeine intake and spontaneous miscarriage, although these have not controlled for other confounding variables. Only high levels of caffeine metabolites in maternal serum are associated with miscarriage, so it would appear that moderate consumption of caffeine is unlikely to increase the risk of miscarriage (Klebanoff et al 1999).
Some chemical agents including lead, ethylene oxide, solvents, pesticides, vinyl chloride and anaesthetic gases have been shown to have some association with fetal loss (Cohen et al 1971, Mur et al 1992, Rowland et al 1996, McDonald et al 1988). Although many environmental toxicologists accept these agents as proven, the evidence for low levels of exposure remains far from convincing.
Radiotherapy and chemotherapeutic agents are accepted causes of miscarriage (Zemlickis et al 1992), although they are only administered during pregnancy in seriously ill women. Although significant ionizing radiation for diagnostic purposes can lead to fetal malformation and miscarriage, a dose of more than 25 rads is associated with a 0.1% risk of abnormality (1 rad is the equivalent of eight to 10 abdominal/pelvic X-ray films).
There is a small increase in the risk of spontaneous miscarriage with general anaesthesia and incidental surgery during the first and second trimesters, although this is higher with gynaecological surgery (Duncan et al 1986).
It has been claimed that impaired psychological well-being predisposes to fetal loss (Stray-Pedersen and Stray-Pedersen 1984), although it has been difficult to exclude other confounding variables. Despite problems with recall bias, there are an increased number of negative life events in women with chromosomally normal as compared with chromosomally abnormal miscarriages (Neugebauer et al 1996), but no differences in hormonal markers of stress have been determined.
Pathophysiology
The exact pathophysiology resulting in the uterine expulsion of early pregnancy remains unknown. Abnormal placentation (either primary or itself secondary to early fetal demise) can either lead to reduced or shallow uterine invasion by the trophoblast, or can itself be caused by reduced invasion. In this situation, the usual reduction in maternal vascular tone cannot occur. It is presumed that this blood flow enters the intervillous space and dislodges the conceptus, thereby leading to embryonic demise if this has not already occurred (Rushton 1995). Nevertheless, even quite large intrauterine haematomata visualized by ultrasound have not prevented live births at term (Pedersen and Mantoni 1990), and the presence of haematomata per se does not increase the risk of miscarriage (Tower and Regan 2001).
Presentation
Threatened miscarriage
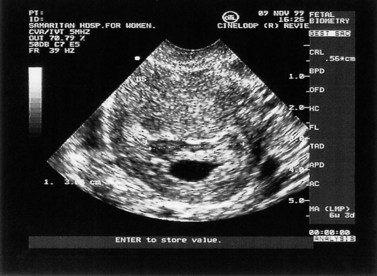
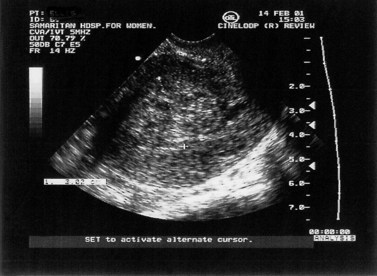
This can be defined as uterine bleeding before 24 weeks of pregnancy (the time of presumed fetal viability) with no evidence of any fetal or embryonic demise. It is usually painless. Characteristically, the bleeding is initially bright red, followed by a reducing brown loss. This can affect up to 25% of all pregnancies and is one of the most common indications for emergency early pregnancy referral. Clinical examination reveals a soft, non-tender uterus, usually of the appropriate gestational size, and a closed cervix. Transvaginal or transabdominal ultrasound scan confirms an ongoing pregnancy (Figure 23.4).
The non-specific nature of abdominal pain, vaginal bleeding and pelvic tenderness precludes their use as predictors of ultimate outcome in women with threatened miscarriage. However, continued vomiting (rather than nausea alone) in early pregnancy is associated with an increased chance of live birth (Weigel and Weigel 1989), presumably because it indicates continued placental hormone production.
Inevitable miscarriage
Miscarriage is a process rather than a single event. Of all women presenting with bleeding in early pregnancy, approximately 50% will ultimately miscarry (Stabile et al 1987). Whilst the cervix remains closed, any pain and bleeding may subside and the pregnancy may continue otherwise normally to term. However, once the cervix opens, miscarriage is inevitable.
Complete and incomplete miscarriage
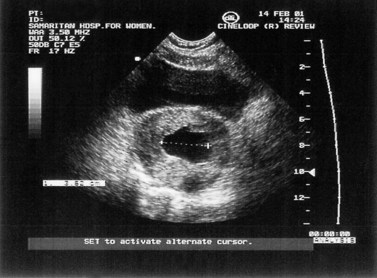
Inevitable miscarriage is either complete or incomplete depending on whether or not all fetal and placental tissues have been expelled from the uterus. The typical features of incomplete miscarriage are heavy bleeding (which may be intermittent) and abdominal cramps. The finding of a dilated cervix on examination in the presence of continued pain and bleeding is usually diagnostic. Ultrasound scan will confirm the presence of retained products of conception (Figure 23.5).
If the symptoms of incomplete miscarriage resolve spontaneously, complete miscarriage may have occurred. Nevertheless, following abdominal and pelvic examination, ultrasound may need to be perfomed to confirm that the uterus is indeed empty. Occasionally, the cervix may close despite the presence of retained products. The number of complete miscarriages is unknown. Many such early miscarriages may go unreported. Early studies of women with threatened miscarriage showed complete miscarriage rates of less than 1% (Stabile et al 1987), although more recent evidence suggests that approximately 20–30% of miscarriages are complete (Chung et al 1994, Mansur 1992). Similarly, expectant management of early fetal demise has demonstrated that, with time, up to 25% of women go on to have a complete miscarriage (Jurkovic et al 1998).
Early fetal demise (missed abortion/miscarriage)
Early fetal demise is where failure of pregnancy is identified before any expulsion of the products of conception occurs. The woman may report a disappearance of the symptoms and signs of early pregnancy, such as nausea and vomiting or breast tenderness. A brown vaginal loss may also be reported. The diagnosis may also be made in otherwise asymptomatic women at routine obstetric/dating ultrasound examination. The diagnosis is made by the lack of fetal heart activity in a pregnancy with a crown–rump length of over 5 mm (Pennell et al 1991), or when two ultrasound examinations 1 or 2 weeks apart have shown no growth and no fetal heart activity. In cases of doubt, a repeat ultrasound is always indicated. Occasionally, a collapsing gestational sac or a failed pregnancy surrounded by clot in utero may be seen (Figure 23.6). Abdominal and pelvic examination often reveals a uterus smaller than expected for the gestational age and a closed cervical os.
Sepsis
This occurs when infection complicates miscarriage or termination of pregnancy. Intrauterine sepsis rarely follows incomplete miscarriage, although the incidence is considerably higher at approximately 3.6% following termination of pregnancy (Frank 1985). The most common infecting organisms are Escherichia coli, Bacteroides, streptococci (both anaerobic and occasionally aerobic) and Clostridium welchii. Occasionally, a history of intrauterine instrumentation may be withheld. The woman usually presents with suprapubic pain, malaise, fever and, occasionally, vaginal bleeding. Findings on examination include abdominal rigidity, uterine and adnexal tenderness, and a closed cervical os. Rarely, septicaemia may ensue, leading to bacteraemic endotoxic shock and possibly maternal death.
Trophoblastic tumours
Trophoblastic tumours include complete and partial hydatidiform moles, choriocarcinoma and placental site tumours. These occasionally present as threatened miscarriage, and suggestive features are noted at ultrasound examination. Trophoblastic tumours are discussed in Chapter 43.
Investigations
The measurement of other fetoplacental hormones and proteins, such as α-fetoprotein, Schwangerschaft protein 1, human placental lactogen, pregnancy-associated plasma protein, oestrogen and progesterone, have all been reported as diagnostic tests in early pregnancy. In rare cases, they may improve the prediction of both early fetal demise and ectopic pregnancy (Grudzinskas and Chard 1992), but their routine use is not indicated.
Treatment
Threatened miscarriage
Early studies demonstrated that the presence of fetal heart activity at ultrasound examination in women who present with a history of bleeding in early pregnancy was associated with a high chance (97–98%) of a live birth (Stabile et al 1987). More recent evidence confirms livebirth rates of 90–95% for younger women, but for women over 40 years of age, miscarriage rates of 15–30% are reported even after the identification of fetal heart activity (Deaton et al 1997, Schmidt-Sarosi et al 1998). Nevertheless, for most women, reassurance and continued medical and emotional support are all that is required.
Bed rest and avoiding penetrative intercourse have historically been advised. If the vascular hypothesis for the pathophysiology of miscarriage is accepted (Hustin and Jauniaux 1997), bed rest may improve pressure variation and flow changes, and therefore improve the outcome. However, there is a paucity of clinical evidence to support this hypothesis. Initial presentation is usually in primary care and, currently, over 96% of general practitioners still advise bed rest and the avoidance of intercourse, although many believe that it does not improve the eventual outcome.
Progesterone supplementation in early pregnancy has been prescribed for over 30 years for women presenting with threatened (and also recurrent) miscarriage. The historical rationale was that a progesterone deficiency would lead to miscarriage. Obviously, the converse may also be true; a failed pregnancy may lead to a progesterone deficiency. There is a wealth of published data, mostly from uncontrolled treatment trials. However, several meta-analyses (Daya 1989, Goldstein et al 1989) have been unable to demonstrate a beneficial effect for progesterone treatment. The routine use of progesterone in threatened miscarriage cannot be justified.
Incomplete miscarriage
Surgical evacuation of the uterus after cervical dilatation, if necessary, has remained the cornerstone of management of incomplete miscarriage in the industrialized world since the 1940s (Hertig and Livingstone 1944). Evacuation and curettage have been regarded as essential to ensure that the uterine cavity is empty, otherwise haemorrhage, infection and later complications such as Asherman’s syndrome may result. Early studies showed a maternal mortality rate of 1.6% in women who did not undergo surgical treatment (Russell 1947). In cases of haemodynamic compromise of cervical shock, appropriate resuscitation and urgent surgical evacuation are indicated. Most cases are performed under general anaesthesia, although effective outpatient curettage has been reported (Fawcus et al 1997). Suction evacuation is generally regarded as a safer technique than sharp curettage, with lower rates of perforation, blood loss and subsequent intrauterine adhesion formation (Edmonds 1992, Verkuyl and Crowther 1993).
The routine use of syntocinon or ergometrine has shown no benefit in reducing blood loss during the surgical treatment of first-trimester incomplete miscarriage (Beeby and Morgan Hughes 1984). Due to the risk of ascending infection and its sequelae, whenever uterine instrumentation is performed, screening for chlamydia infection is recommended, although the use of prophylactic doxycycline is only likely to be of benefit in areas of relatively high prevalence (Prieto et al 1995).
Although a minor procedure, surgical evacuation is associated with rare but serious morbidity. Complications include tearing or lacerations to the cervix, perforation of the uterus, which may also lead to bowel perforation, bladder perforation, damage to the broad ligament, infection, Asherman’s syndrome (intrauterine adhesions) and haemorrhage (Ratnam and Prasad 1990). The incidence of serious morbidity has been estimated at 2.1% (Lawson et al 1994, Royal College of General Practitioners/Royal College of Obstetricians and Gynaecologists 1985), of which the most common problem is infection. This can lead to later sequelae including secondary infertility, ectopic pregnancy and Asherman’s syndrome. The incidence of mortality associated with surgical evacuation of the uterus has been estimated at 0.5 per 100,000 (Lawson et al 1994).
Recent studies demonstrated the efficacy of expectant management or ‘observation alone’ in women with incomplete miscarriage (Nielsen and Hahlin 1995, Hurd et al 1997). In cases where there was no haemodynamic compromise or maternal anaemia, spontaneous resolution occurred within 3 days in up to 80% of cases with minimal retained products (15–50 ml). Therefore, in women with minimal intrauterine tissue (after ectopic pregnancy has been excluded), expectant management is safe. However, large volumes of retained products are associated with an increase in complications, primarily infection and prolonged bleeding (Hurd et al 1997). There is no evidence that future fertility is impaired following expectant management (Kaplan et al 1996).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree