80 Spinal Cord Disorders
Etiology and Pathogenesis
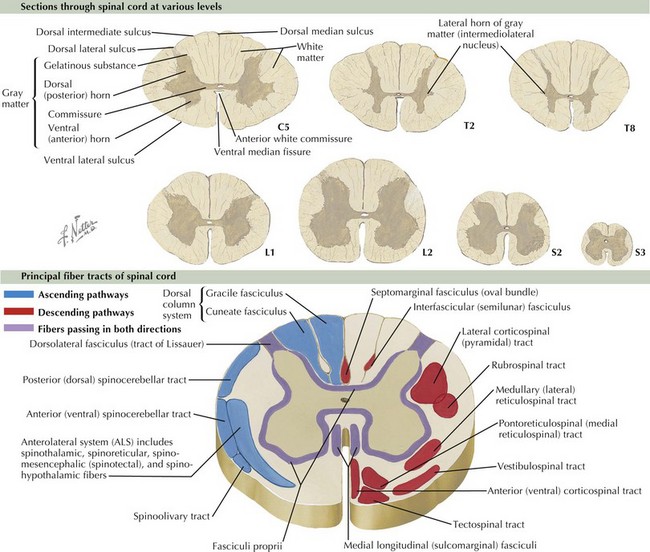
According to the Centers for Disease Control and Prevention, spina bifida, the most common neural tube defect, occurs at a rate of two in 10,000 live births and results in varying degrees of disability from clinically normal to paraplegia. Traumatic spinal cord injury occurs at a rate of about 40 cases per million people per year and annually costs $9.7 billion in health care costs. Of these cases, it is estimated that up to half occur in adolescence and young adulthood. To diagnose and treat the disorders of the spinal cord, an understanding of its anatomy and how to examine for dysfunction of the spinal cord is imperative. The spinal cord is divided into four sections: cervical, thoracic, lumbar, and sacral (C, T, L, and S). It terminates at vertebral body level L2–L3 in infants, and in grown children and adults, it terminates at level L1–L2, where the cauda equina, the collection of nerves exiting the cord, begins. The spinal cord itself is sectioned in to a central H-shaped region of gray matter and surrounding white matter tracts (Figure 80-1).
Clinical Presentation and Differential Diagnosis
There are common patterns of motor and sensory involvement depending on the localization of disease within the spinal cord. Table 80-1 describes the features of some typical patterns or spinal cord disease and their common causes (Figure 80-2).
Table 80-1 Features of Typical Patterns or Spinal Cord Disease and Common Causes
| Localization | Common Pattern of Weakness and Sensory Loss | Common Causes in Pediatric Patients |
|---|---|---|
| Cervical spinal cord | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|