■ ACUTE STABILIZATION
The acute management of the child with a suspected spinal cord emergency hinges on immobilization and stabilization of the spine in cases of trauma or suspected trauma and on monitoring of autonomic function. Careful examination must be done to evaluate for respiratory compromise needing intubation, blood pressure instability, arrhythmias, and bladder retention. The two major causes of death in SCI are shock and aspiration. Therefore it is crucial to monitor airway and respiratory status as well for blood pressure instability and arrhythmias by using continuous cardiorespiratory monitors. Patients should be constantly evaluated for adequate oxygenation (Fio2) and adequate ventilation. For children who are not intubated, vital capacity and negative inspiratory force should be followed to assess for respiratory deterioration. Cautious intubation may be required if the C-spine is not yet cleared. A neurologic examination and general examination must be performed since other major injuries may be masked below the level of the SCI. Patients with SCI may have disruption of their bowel and bladder circuits, therefore a urinary catheter is usually required. A nasogastric tube (to low suction) may also be needed to prevent aspiration and to decompress a paralytic ileus that is common in this population.
■ ACUTE IMAGING
Emergent diagnostic neuroimaging, including spine MRI to examine the cord itself and ligaments should be performed so that the pathologic process can be identified and treated immediately. In most cases, sagittal “scout” films of the entire spine should be performed since the full extent of injury may not be evident on the clinical examination. If that is not possible, several levels above and below the clinical level of injury should at least be studied. In many cases, a 1.5 Tesla MRI scanner images the spinal cord with more clarity than the stronger 3 Tesla scanner. If a tumor, infection, demyelinating process, or vascular malformation is suspected, an MRI performed with and without gadolinium should be performed.
■ TRAUMA
Traumatic SCI in pediatric patients is an uncommon event, but can be devastating when it occurs. Fortunately, the incidence of traumatic SCI is less than 10% of all patients who have an SCI. Over 60% of SCIs in children occur in the cervical spine and less than 30% occur in the thoracolumbar spine (5). Children have a high head-to-body ratio, a sizeable amount of ligamentous laxity, and underdeveloped paraspinal muscles due to age. Due to these differences in anatomy and physiology, the pediatric population is predisposed to injury of the cervical spine in contrast to adults (6). More specifically, younger children (≤ 8 years) have the tendency for injuries of the upper cervical spine, and older children and adolescents have a predilection for injuries of the lower cervical spine (7). Injuries to the thoracolumbar spine occur more commonly in older children and adolescents and are often accompanied by thoracoabdominal injuries (5,8). The majority of children with cervical spine trauma can be managed nonoperatively with a hard collar or halo with good outcomes. However, it is not always the best quality of life option for a child to wear a hard collar or halo for many weeks. Surgical management such as anterior or posterior fusion and instrumentation may be necessary in severe unstable injuries, or for those patients who have a high likelihood of nonfusion secondary to anatomical or environmental influences (9). Fractures in the pediatric population are uncommon and tend to resemble fractures seen in adults (Figures 15.1A and B). Fractures in the pediatric population are most often due to trauma.
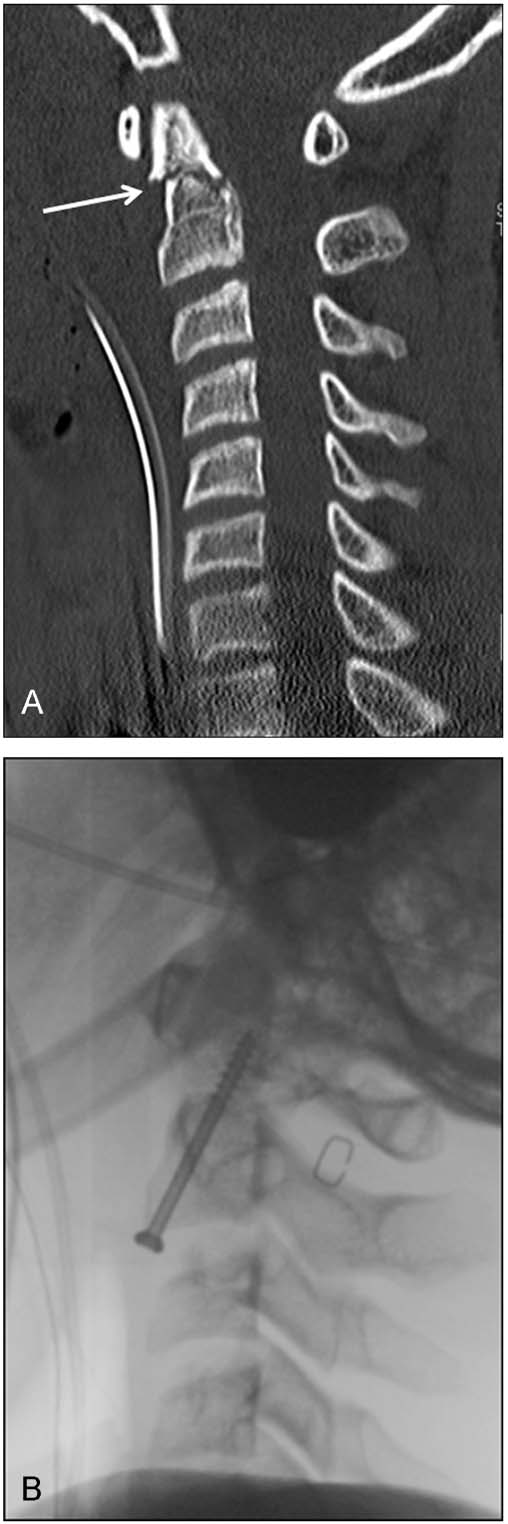
FIGURE 15.1 A 16-year-old male involved in a motor vehicle accident. Lateral C-spine x-ray showed an abnormality, thus a sagittal computed tomographic scan (A) was obtained which showed a type II odontoid fracture (arrow). The patient underwent an anterior instrumented fusion with an odontoid screw (B).
Atlantooccipital Dislocation
Atlantooccipital dislocation (AOD) is a devastating condition that often ends in cardiorespiratory arrest prior to hospitalization. Historically, AOD had been considered almost always fatal and associated with devastating neurologic injury. The injuries are highly unstable and the mechanism of injury is almost always a hyperextension injury caused by a high velocity injury such as a motor vehicle accident (1). A large force is necessary to disrupt the ligaments that connect the cranium from the rest of the cervical spine. AOD is five times more common in the pediatric population versus the adult population (10). Additionally, children with trisomy 21 have atlantoaxial instability and are at particular risk for AOD with or without subluxation (11). Likely due to a variety of factors including improved prehospital resuscitation, diagnostic imaging, and a higher index of suspicion, there has been an increase in posttraumatic AOD survival rates (12).
Diagnosis can be made with plain cervical radiographs (Figure 15.2A) and is aided with computed tomographic (CT) scans and MRI (Figure 15.2B). For children who survive AOD with an incomplete SCI, the literature supports surgical intervention (occipital-cervical fusion) for older children (Figure 15.2C) and immobilization for infants (10,13,14). The signs of AOD are often subtle, and the possibility of this diagnosis must be kept high on the differential, especially in the pediatric population where ligamentous injury without bony fractures may not be apparent on x-rays or CT. Even in the absence of neurologic signs, a methodical approach to evaluating plain x-rays with subsequent use of CT scans and MRI is essential to identifying AOD.
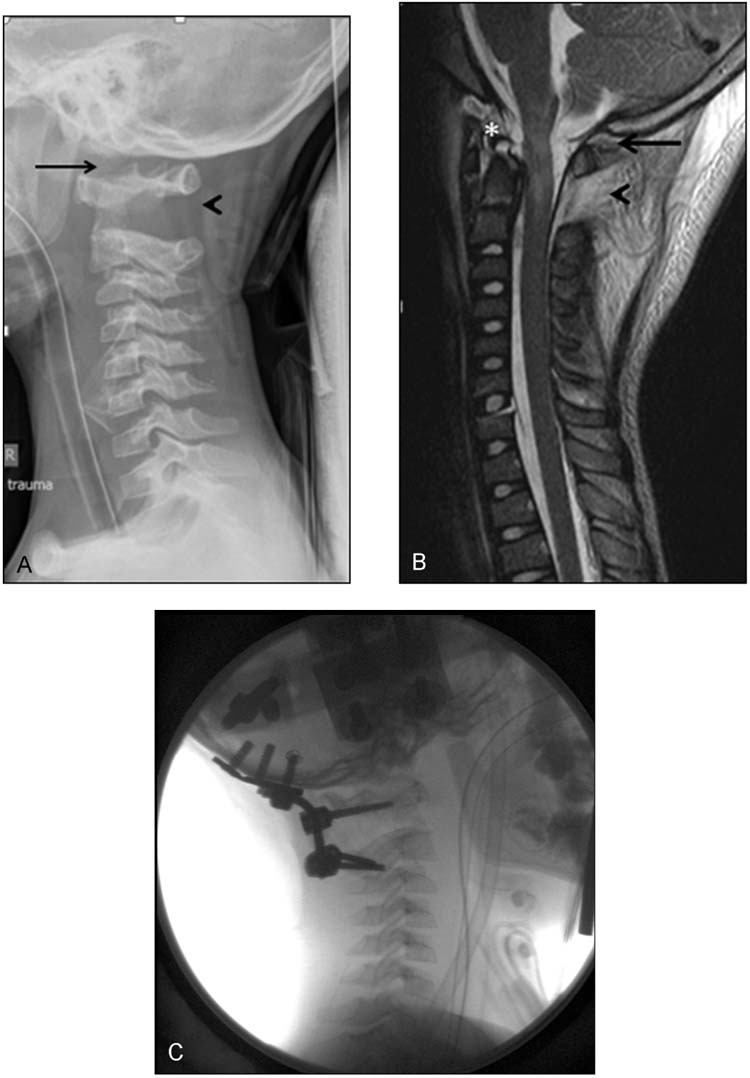
FIGURE 15.2 A 5-year-old boy unrestrained passenger in a motor vehicle accident was found to be quadriplegic but with Glasgow Coma Score of 15. Lateral radiographs (A) and magnetic resonance imaging (MRI) (B) revealed an atlantooccipital (arrow) as well as an atlantoaxial dissociation (arrowhead) with disruption of the cruciate and alar ligaments (asterisk). The patient underwent an occipital to cervical (C2) fusion (C).
Pseudosubluxation
Pediatric pseudosubluxation refers to the anterior displacement of C2 (axis) on C3. In children up to 10 years of age, the normal flexion mobility of C2 on C3 of 2 to 3 mm may be misinterpreted for pathologic motion (13). Especially in the presence of cervical muscle spasm, when the head is flexed, there may be an exacerbation of anterior displacement. This anatomical difference occurs because of the increased laxity in ligaments in children and also because of the increase in horizontal anatomical alignment of the facet joint than in adults (14).
Pharmacologic Treatment
A recent meta-analysis examined eight adult randomized controlled trials in which steroids were administered in the setting of acute spinal cord injury. Seven of the eight studies used high-dose methylprednisolone. A common regimen was a bolus of 30mg/kg followed by a 24 hour infusion at 5.4mg/kg/hour. The study concluded that steroids improved neurologic outcome at up to one year if started within 8 hours of the injury. One of the trials extended the infusion to 48 hours after injury and demonstrated that additional motor and functional improvement was gained by extending the length of the infusion. This was particularly true in patients in whom the treatment was not begun between 3 and 8 hours of the injury (50). There are no randomized clinical trials for high-dose steroids in the setting of acute pediatric spinal injury, but steroids may be considered in this setting. They are used routinely to decrease edema in other pediatric spine diseases like tumors and vascular malformations. However, in the settings of tumors and vascular malformations, dexamethasone given every 4 to 6 hours may be more commonly used than methylprednisolone.
■ INFECTIONS
Prompt diagnosis of spine infections is crucial since early treatment can decrease morbidity and mortality (15). Spine infections may be divided into a handful of major categories: vertebral osteomyelitis, discitis, epidural abscess, subdural abscess/empyema, meningitis, and cord abscess. We will discuss the two more common infections that affect the pediatric population.
Discitis and Vertebral Osteomyelitis
Discitis and vertebral osteomyelitis are interrelated and describe different aspects of the same clinical spectrum. Children rarely present to clinic with back pain, so the diagnosis of this disease can be challenging, leading to a delay in diagnosis or unnecessary and futile tests and treatments. Children of less than 3 years of age tend to be the age group most affected (16). Usually, children with discitis are younger than those with vertebral osteomyelitis, and discitis most commonly affects the lumbar spine (17,18). The typical presentation is an older child who refuses to walk or to stand due to back pain or a toddler who refuses to sit. The underlying pathologic cause may be infectious, inflammatory, or traumatic. Discitis in younger children may be more common than in adults and older children because of the presence of abundant intraosseous arterial anastomoses that nourish the nucleus pulposus that disappear by adulthood (1). Since the cartilaginous disc has an abundant blood supply in children, the treatment of choice is long-term antibiotics. Surgery is a last resort, reserved for cases that progress despite antibiotic treatment or that develop spinal instability (19, 20).
Spinal Epidural Abscess
Epidural abscesses are uncommon in the adult population and even less frequent in the pediatric population; however, they are seen not uncommonly in the tertiary care setting. Because of the rare nature of this disease process in children, management is controversial with no consistent surgical and nonsurgical treatment approaches. In a study examining pediatric spinal epidural abscesses over 15 years (21), the incidence of epidural abscesses was stated as 0.6 per 10, 000 hospital admissions, a figure comparable to an estimate in adults of 0.2 to 1.2 per 10, 000 hospitalizations (22). Especially in the pediatric population, epidural abscess is often undiagnosed until the progression of neurologic deficits because of the rarity of the disease process (23). The common presenting symptoms are similar to those in adults, including fever, general malaise, pain, and gait difficulties. Some reports suggest that children may present with pain in the hip, leg, or abdomen, presumably from referred pain or radiculopathy rather than midline back pain (23,24). However because there is a broad range of nonspecific symptoms, the time from symptom onset to diagnosis and treatment can be prolonged, which increases the likelihood of developing neurologic deficits including weakness, paresthesias, and even paraplegia.
In contrast to adults, only a third of children have an underlying medical condition that predisposes them to spinal epidural abscesses (21). The most common disorders include sickle cell disease or immunosuppression from chemotherapy for malignancy (21). The lower thoracolumbar areas of the spine are more prone to epidural infections because the epidural space is wider and the spinal cord is narrower in this area. This epidural space is septated and contains larger amounts of adipose and vascular tissue which is the reason it has the potential to harbor infections. However, the septations are also potentially responsible for limiting extension of infection in adults. In children, the epidural space and vasculature are not as well developed and are still in the maturation phase with less adipose tissue. The anatomical differences between adults and children partially explain the age-related differences in abscess formation. Children, therefore, have the potential of multisegmented and very extensive epidural abscesses (Figure 15.3A and B). The most common mechanism of epidural abscess is hypothesized to be hematogenous spread into the epidural space from another infection such as endocarditis and urinary tract infections. There is also the possibility of direct extension from vertebral osteomyelitis or superinfection of a hematoma as the result of a trauma (24). Most of the literature, including reviews, report that over 80% of adult and pediatric epidural abscesses are caused by a Staphylococcus aureus infection (24). Some less common bacteria include Pseudomonas, Pneumococcus, and Escherichia coli (21). Mechanical compression from epidural abscesses may cause SCI, but this is not always the underlying cause of injury. Vascular mechanisms including thrombophlebitis of epidural veins or venous thrombosis and subsequent infarction have been described (22).
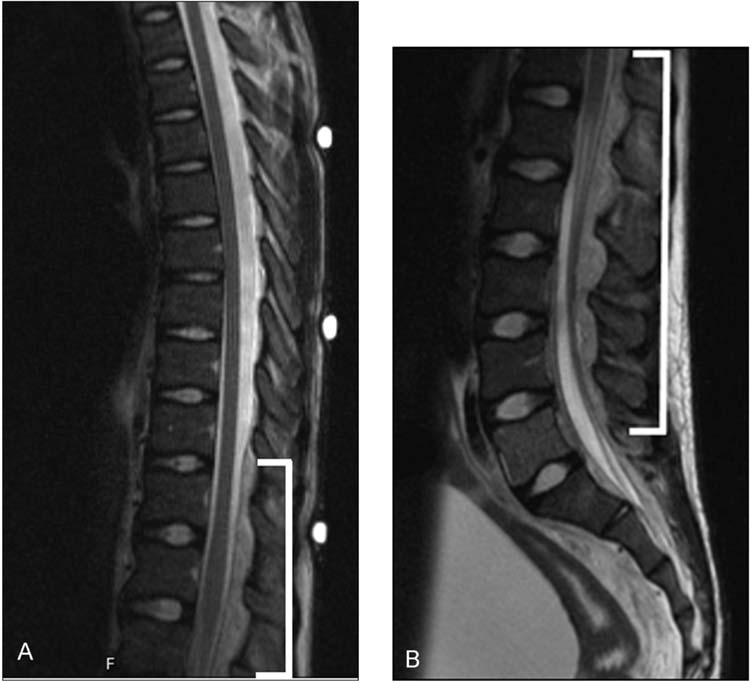
FIGURE 15.3 A 12-year-old male with sepsis from a urinary tract infection was found to have decreased motor strength (2/5) in his lower extremities with the inability to walk. Sagittal MRI of the thoracic (A) and lumbar (B) levels was obtained which showed an extensive thoracolumbar posterior epidural abscess without spinal cord infarction or compression (brackets). The patient’s parents elected not to undergo any surgical intervention, and the patient was placed on antibiotics. One week later, the patient was walking unassisted with major improvement in his motor strength (4+/5).
The treatment of spinal epidural abscess remains controversial especially in the pediatric population. There have been many articles in the adult literature that illustrate using antibiotic therapy only without surgical intervention for the treatment of epidural abscesses with good neurologic outcome (25,26). The caveat in these case series was that the patients tended to present early in the course of the infection with no neurologic compromise. There has been very limited literature with only a couple of case reports on spinal epidural abscesses in neurologically intact children that were successfully treated with antibiotics alone without surgical intervention (21,27). The gold standard treatment for epidural abscess includes combined surgical drainage and extended antibiotic therapy in children (28). The goal of surgical intervention is to decompress the spinal cord or thecal sac by performing a laminectomy to remove the compressive purulent material or granulation tissue. This will enable systemic antibiotics to penetrate the region (29). Exceptions to this approach can be made if the child has no neurologic deficit with extensive infection, where multilevel laminectomy would be the only treatment (27). The complications and morbidity associated with multilevel laminectomy in children are considerable, as this operation can lead to kyphosis and spinal instability.
■ TUMORS
Spinal cord tumors are a relatively rare diagnosis in both pediatric and adult populations. In children, the incidence is even less common and accounts for 0.5% to 10% of all pediatric central nervous system tumors (30,31) depending on the region of the world. Spinal tumors can be classified into three groups: extradural, intradural extramedullary, and intradural intramedullary. Extradural tumors arise from vertebral bodies or epidural tissues external to the leptomeninges and spinal cord (Figure 15.4A). Metastatic tumors to the spinal cord usually fall within this category; however, common pediatric tumors such as medulloblastomas or ependymomas may have intradural “drop mets” (Figure 15.4B). Intradural extramedullary tumors arise from the leptomeninges or nerve roots but arise outside of the neuronal tissue of the spinal cord. This category includes common adult tumors such as meningiomas and peripheral nerve sheath tumors. Intramedullary tumors also arise within the meninges but from cells within the spinal cord itself. They are invasive and destructive to spinal cord tracts and gray matter (32,33). The incidence of intramedullary tumors is higher in children than in adults with reports citing ranges from 44% to 63% (31,34); this is compared to an average of 5% in the adult literature (1).
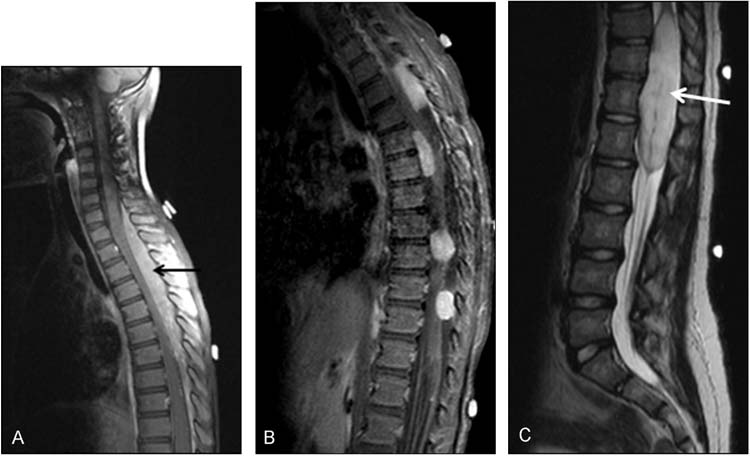
FIGURE 15.4 A 3-year-old male who presented with back pain and difficulty with ambulation (A). His neurologic deficit progressed to paraplegia and MRI showed a large cervicothoracic epidural lesion causing compression of the spinal cord (black arrow). He was taken to the operating room for gross total resection of the mass and pathology showed Burkitt’s lymphoma. A 3-year-old female who was diagnosed with a large posterior fossa medulloblastoma (B). Surveillance spinal imaging showed multiple intradural extramedullary “drop mets” that enhanced with gadolinium on sagittal T2 MRI. She underwent surgical resection of her intracranial mass and went on to receive chemotherapy and radiation of her neuroaxis. At 5-year follow-up, she had no residual disease in her brain or spine. An 11-year-old female who started having abnormal gait around 18-months of age that was diagnosed as cerebral palsy (C). She had worsening paresthesias, wide-based gait, incontinence of urine and bowel, and motor strength of 3/5 in her left lower extremity. Sagittal T2 MRI shows a T10-L2 intradural intramedullary spinal cord tumor (white arrow). The patient underwent a moderate debulking, and pathology revealed a fibrillary astrocytoma. She underwent proton therapy and treatment with oral Temodar.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


