Features of skin disorders in children include: • In the newborn, transient skin disorders are common but need to be distinguished from serious or permanent conditions • Atopic eczema affects up to 20% of children • Skin infections and infestations, especially viral warts and head lice, are common in school-aged children Common naevi and rashes in the newborn period are described under the examination of the newborn infant (see Ch. 9). Some less common skin conditions presenting in the newborn period are described in this chapter. This is an uncommon but potentially serious blistering form of impetigo, the most superficial form of bacterial infection, seen particularly in the newborn (Fig. 24.1). It is most often caused by Staphylococcus aureus. Treatment is with systemic antibiotics, e.g. penicillinase-resistant penicillin (see also Ch. 14). Congenital moles occur in up to 3% of neonates and any that are present are usually small. Congenital pigmented naevi involving extensive areas of skin (i.e. naevi >9 cm in diameter) are rare but disfiguring (Fig. 24.2) and carry a 4–6% lifetime risk of subsequent malignant melanoma. They require prompt referral to a paediatric dermatologist and plastic surgeon to assess the feasibility of removal. This is due to a defect in biosynthesis and distribution of melanin. The albinism may be oculocutaneous, ocular or partial, depending on the distribution of depigmentation in the skin and eye (Fig. 24.3). The lack of pigment in the iris, retina, eyelids and eyebrows results in failure to develop a fixation reflex. There is pendular nystagmus and photophobia, which causes constant frowning. Correction of refractive errors and tinted lenses may be helpful. In a few children, the fitting of tinted contact lenses from early infancy allows the development of normal fixation. The disorder is an important cause of severe visual impairment. The pale skin is prone to sunburn and skin cancer. In sunlight, a hat should be worn and high factor barrier cream applied to the skin. This is a rare group of genetic conditions with many types, characterised by blistering of the skin and mucous membranes. Autosomal dominant variants tend to be milder; autosomal recessive variants may be severe and even fatal. Blisters occur spontaneously or follow minor trauma (Fig. 24.4). They need to be differentiated from scalds. Management is directed to avoiding injury from even minor skin trauma and treating secondary infection. In the severe forms, the fingers and toes may become fused, and contractures of the limbs develop from repeated blistering and healing. Mucous membrane involvement may result in oral ulceration and stenosis from oesophageal erosions. Management, including maintenance of adequate nutrition, should be by a multidisciplinary team including a paediatric dermatologist, paediatrician, plastic surgeon and dietician. This is a rare manifestation of the inherited ichthyoses, a group of conditions in which the skin is dry and scaly. Infants are born with a taut parchment-like or collodion-like membrane (Fig. 24.5). Emollients are usually applied to moisturise and soften the skin. The membrane becomes fissured and separates within a few weeks, usually leaving either ichthyotic or less commonly, normal skin. Napkin rashes are common, although irritant reactions are much less of a problem with the widespread use of disposable nappies, as they are more absorbent. Some causes are listed in Box 24.1. Irritant dermatitis, the most common napkin rash, may occur if nappies are not changed frequently enough or if the infant has diarrhoea. However, irritant dermatitis can occur even when the napkin area is cleaned regularly. The rash is due to the irritant effect of urine on the skin of susceptible infants. Urea-splitting organisms in faeces increase the alkalinity and likelihood of a rash. Candida infection may cause and often complicates napkin rashes. The rash is erythematous, includes the skin flexures and there may be satellite lesions (Fig. 24.6). Treatment is with a topical antifungal agent. This eruption of unknown cause presents in the first 2 months of life. It starts on the scalp as an erythematous scaly eruption. The scales form a thick yellow adherent layer, commonly called cradle cap (Fig. 24.7a). The scaly rash may spread to the face, behind the ears and then extend to the flexures and napkin area (Fig. 24.7b). In contrast to atopic eczema, it is not itchy and the child is unperturbed by it. However, it is associated with an increased risk of subsequently developing atopic eczema. Mild cases will resolve with emollients. The scales on the scalp can be cleared with an ointment containing low-concentration sulphur and salicylic acid applied to the scalp daily for a few hours and then washed off. Widespread body eruption will clear with a mild topical corticosteroid, either alone or mixed with an antibacterial and antifungal agent if appropriate.
Skin disorders
The newborn
Bullous impetigo

Melanocytic naevi (moles)

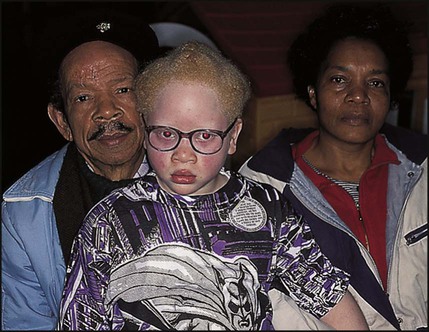
Albinism
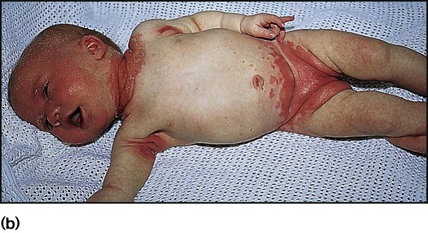
Epidermolysis bullosa
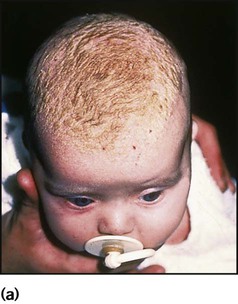
Collodion baby

Rashes of infancy
Napkin rashes
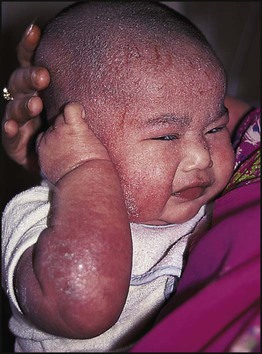
Infantile seborrhoeic dermatitis