2.1 Physiological Skin Changes in Pregnancy
Skin changes occur during pregnancy under hormonal influence. Usually reassurance by the midwife or GP is all that is required, but further investigation and referral may be indicated in some cases.
Hyperpigmentation
The areola, nipples, genital skin, axillae, linea alba (becomes the linea nigra) and inner thighs can darken. Sometimes moles, freckles and scars also become darker. Hyperpigmentation usually fades postpartum1.
Melasma (chloasma)
Melasma (mask of pregnancy) is very common, affecting 75% pregnant women1, and consists of symmetrical increased pigmentation over the cheeks, jaw line, brow or upper lip. Melasma is worsened by sunlight so sun protection should be advised. It usually fades postpartum (see Figure 2.1.1)
Figure 2.1.1 Melasma (Burns 2010).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Hair
It is common to have some degree of hirsutism during pregnancy. This resolves 6 months after delivery. Postpartum there is often an increased loss of hair (telogen effluvium) which lasts for up to 15 months. (It may be worth checking for other causes of generalised hair loss, e.g. ferritin levels and thyroid function tests.)
Striae Gravidarum
These appear in the sixth and seventh month on the abdomen, breasts, thighs or inguinal areas, they gradually fade postpartum but do not resolve (see Figure 2.1.2).
Figure 2.1.2 Striae gravidarum (Buxton 2009).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Skin Tags
May occur after the first trimester in the flexures, on the face chest and neck. They may regress postpartum.
Vascular Changes
Spider naevi (Figure 2.1.3), facial flushing, varicose veins, red swollen gums and palmar erythema can all occur and resolve postpartum.
Figure 2.1.3 Spider naevi (Buxton 2009).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Pruritus
Itching without a rash can occur in up to 20% of pregnant women; it resolves spontaneously. Moisturisers and 1% menthol in aqueous cream may help.
Moles (naevi)
Significant changes to moles during pregnancy need referral to dermatology/GP for further evaluation. Women who develop malignant melanoma during pregnancy do not have a worsened prognosis (see Chapter 18.8).
2.2 Dermatoses Specific to Pregnancy
Atopic Eruption of Pregnancy (AEP)
This is the commonest pregnancy related rash; 20% have eczema and there is often a family history of atopy. It occurs on the face, neck, chest and flexures, as red scaly itchy patches, with some papules and nodules from scratching, in the second and third trimesters. Treat as eczema. UVB can be helpful. Rarely oral steroids are needed (Figure 2.2.1). There is no adverse effect for the mother or baby.
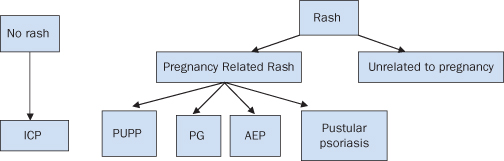
Figure 2.2.1 Dermatoses specific to pregnancy. Any blistering rash in pregnancy requires urgent referral for a dermatology opinion (Buxton 2009). AEP, Atopic eruption of pregnancy. PUPP, Pruritic urticarial papules and plaques of pregnancy. PG, pemphigoid gestationis. ICP, Intrahepatic cholestasis of pregnancy.
This figure is downloadable from the book companion website at www.wiley.com/go/robson
Pruritic Urticarial Papules and Plaques of Pregnancy (PUPP)
This occurs in 1 in 160 pregnancies and predominantly affects primiparous women in the third trimester. The rash usually starts in the abdominal striae and spares the umbilicus (Figure 2.2.2). It consists of urticarial papules and plaques but also vesicular, eczematous, annular and target lesions. The rash is usually itchy and disappears 10 days after delivery. There is no risk to mother and baby. Recurrence in subsequent pregnancies is unusual. Treatment is with topical steroids, moisturisers, 1% menthol in aqueous cream and if severe oral steroids. Appendix 2.2.1 outlines the use of emollients and steroid creams.
Figure 2.2.2 Pruritic urticarial papules and plaques of pregnancy (PUPP) (Buxton 2009).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Pemphigoid Gestationis (PG)
This is a rare autoimmune blistering disease occurring in 1 in 40 000 pregnancies. It starts in the second and third trimesters (occasionally postpartum), with an itch, followed by urticarial lesions, then large blisters (bullae) develop often around the umbilicus, which spread and can involve hands, soles and face. It will often quieten in late pregnancy but can flare badly postpartum. Referral to dermatology is necessary for a skin biopsy and further management with moisturisers, topical steroids, antihistamines, and oral steroids. Risk of premature delivery, low birth weight and small for gestational age is increased. Occasionally there are transient bullous lesions in the baby (10% of babies)1. It frequently recurs in future pregnancies (Figure 2.2.3).
Figure 2.2.3 Pemphigoid gestationis (PG) (Buxton 2009).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Pustular Psoriasis of Pregnancy
This is rare; most patients do not have a history of psoriasis. It can occur during any trimester, presents as itchy plaques surrounded by rings of sterile pustules, often starts in flexures and may spread all over. The patient feels unwell with diarrhoea, vomiting, fever and malaise. There is an increased risk of miscarriage, still birth and low birth weight. The rash resolves quickly postpartum (occasional flare). Recurrences can occur in future pregnancies. Urgent referral to dermatology is indicated. Treatment is with high dose steroids and an early delivery.
Intrahepatic Cholestasis of Pregnancy (ICP)
See Chapter 10.8.
2.3 Eczema
EXPLANATION OF CONDITION
Eczema is an itchy, dry, erythematous, skin condition. It can develop anywhere on the body but typically is found in the flexures (Figure 2.3.1).
Figure 2.3.1 Eczema (Buxton 2009).
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Acute eczema usually displays all the clinical signs of infection, heat, pain, and redness, with scaling and excoriations. If infected it is accompanied by a clear discharge which dries to form a crust (Figure 2.3.2).
Figure 2.3.2 Infected eczema.
This figure is downloadable from the book companion website at www.wiley.com/go/robson

Chronic eczema is due to constant scratching; the skin becomes thick and leathery (lichenification), with scaling, fissuring and redness.
Dermatitis – the terms dermatitis and eczema are now used interchangeably by most dermatologists.
COMPLICATIONS
- Bacterial infections: These are common, are caused by reduced waterproofing of the skin and Staphylococcus and/or Streptococcus. The eczema is usually weepy, crusted and yellow. Only swab if resistance is suspected or if you suspect a micro-organism other than Staphylococcus.
- Viral infections: The presence of the herpes virus (cold sore) in patients with eczema can lead to widespread skin infection with the virus (eczema herpeticum). This needs immediate referral to the dermatology team.
NON-PREGNANCY TREATMENT AND CARE
All skin conditions have the potential to lower an individual’s quality of daily life and the psychosocial impact of this condition must always be considered when treatment is discussed.
General advice
- Education plays an important role in the management of eczema. Advice about allergens, explanation about eczema and its management should be given2.
Topical treatment (1st line therapy)
- Daily lukewarm baths with a bath oil help to relieve symptoms, e.g. Oilatum bath or Dermol 600.
- Shower gels or soap should not be used. Suitable soap substitutes include, e.g. Hydromol bath/shower emollient or Hydromol ointment.
- Topical emollients should be applied after bathing when skin is still moist. Emollients can be applied as frequently as required during the day.
- Topical steroids: The correct potency for the severity of the eczema should be prescribed (a mild steroid, e.g. 1% hydrocortisone for mild eczema , a moderate steroid, e.g. Eumovate for moderate eczema and a potent steroid, e.g. Betnovate for severe eczema). Steroids can be stepped up and down according to severity3. Only hydrocortisone 1% should be used on the face.
- Antihistamines: May not help itching but may aid sleep if a sedating antihistamine is taken at night.
- Generalised secondary bacterial infection is treated with systemic antibiotics, e.g. flucloxacillin or erythromycin.
- Localised bacterial infections can be treated with topical creams, e.g. Trimovate or Betnovate C.
2nd line therapy
- Topical calcineurin inhibitors: Tacrolimus or pimecrolimus are only used for difficult to treat eczema where there is no infection.
- Oral prednisolone, methotrexate, azathioprine, ciclosporin, UVB or PUVA (psoralen with long-wave UVA) light treatment can be used to treat severe cases of eczema.
PRE-CONCEPTION ISSUES AND CARE
Atopic eczema generally worsens in pregnancy. However, improvement has been reported in up to 24% of cases2.
Emollients, topical steroids and antihistamines are all safe to use.
Topical tacrolimus/pimecrolimus are not to be used in pregnancy.
Azathioprine is not proven to be teratogenic, however there have been reports of low birth weight babies, spontaneous abortion and premature labour/birth. Ciclosporin is not considered to be any more harmful than azathioprine4. It would be advisable for any woman on these medications to seek preconception advice (see Appendix 11.1.1). Methotrexate should be stopped at least 3 months prior to conception.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


