90 Skin and Soft Tissue Infections
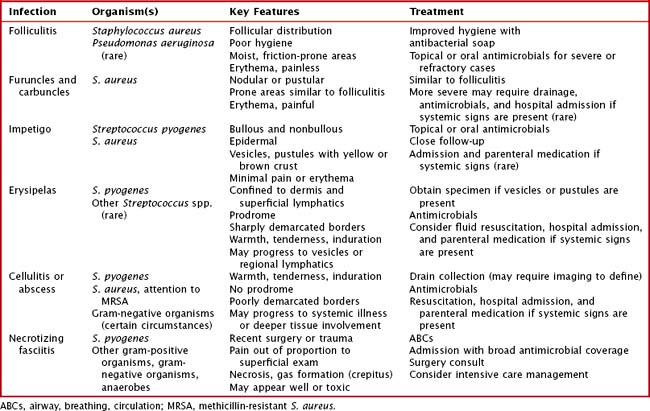
For clinicians, it is essential to quickly recognize these infections, assess and evaluate their depth and rate of spread, and begin appropriate antimicrobial treatment (Table 90-1).
Clinical Presentation
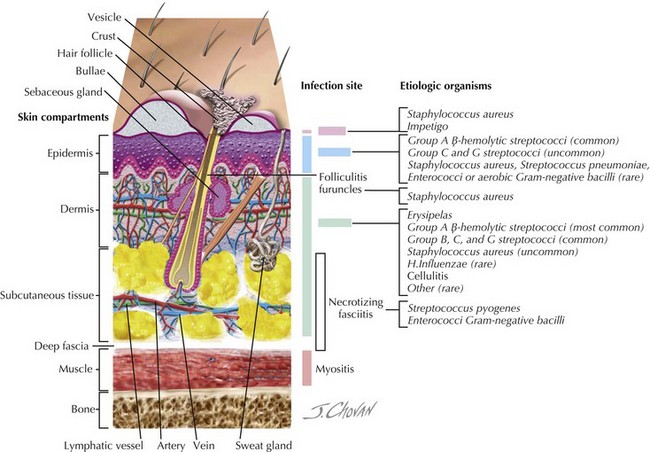
Nearly all skin and soft tissue infections are characterized by a varying degree of erythema, pain or tenderness, and warmth. For clinicians, after it has been established that there is a likely bacterial infection, the next steps are to determine the depth and degree of the infection and its rate of spread (Figure 90-1).
Folliculitis
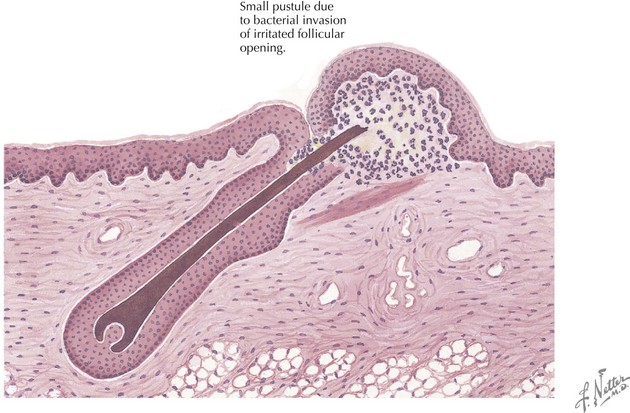
Folliculitis is a superficial pustule or local area of inflammation surrounding a hair follicle (Figure 90-2). It can be solitary, but it can also occur in clusters. The most commonly affected areas include those of high moisture and friction, such as the axillae and inguinal creases, but the scalp, extremities, and perioral and paranasal areas are also commonly affected. Poor hygiene and a humid environment are risk factors, as are active drainage from more severe nearby wounds. S. aureus is the predominant organism, with the exception of folliculitis that occurs shortly after immersion in a poorly maintained pool or hot tub, in which case Pseudomonas aeruginosa is the likely organism. Folliculitis is not usually painful, but if progression to more significant infections takes place, pain can become significant.
Furuncles and Carbuncles
Furuncles (boils) and carbuncles are uncommon in childhood, with the notable exception of children with atopic dermatitis (Figure 90-3). This population, perhaps because of its higher rates of S. aureus (the primary causative organism) colonization, is at risk for these infections. Both of these infections can be sequelae of poorly managed folliculitis. A furuncle is an acute infection of the hair follicle, often accompanied by necrosis, that begins as a nodule and then progresses to a pustule. Common locations are the neck, face, axillae, groin, and buttocks, and risk factors are similar to those of folliculitis, with the addition of hyperhidrosis, anemia, and obesity. A carbuncle is a collection of confluent furuncles, often with multiple drainage points. They can be single or multiple, frequently appearing in crops in areas similar to furuncles. Both lesions are erythematous and can be painful, and occasionally, carbuncles can progress to the point where the patient develops constitutional symptoms and laboratory evidence of more severe infection.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree