89 Sexually Transmitted Infections
Vaginitis
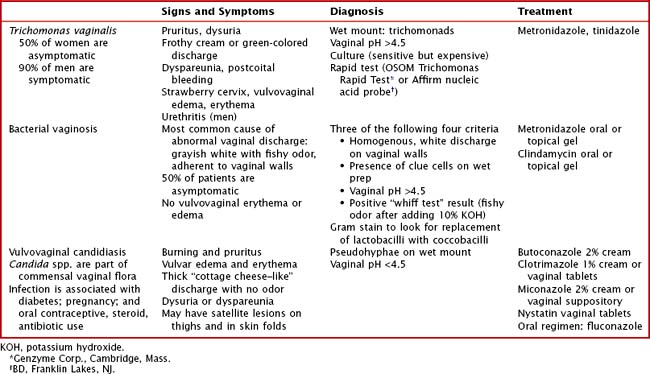
Vaginitis is one of the most common symptoms among adolescent females. It typically presents as increased or malodorous vaginal discharge and vulvovaginal erythema or edema. Although this can be caused by chemical or physical irritation, infectious causes include Trichomonas vaginalis, bacterial vaginosis (caused by Gardnerella vaginalis, genital Mycoplasmas, anaerobic bacteria) and Candida spp. In postpubertal women, normal vaginal flora is dominated by lactobacilli, which decrease the pH within the vaginal canal and prevent colonization by pathogens. However, any change to the genital environment can alter this balance and result in infection. Except T. vaginalis vaginitis, infectious vaginitis is not an STI. However, vaginitis is frequently diagnosed as part of the evaluation for STIs. The signs, symptoms, diagnostic criteria, and treatments for each infection are shown in Table 89-1.
Urethritis and Cervicitis
Clinical Presentation
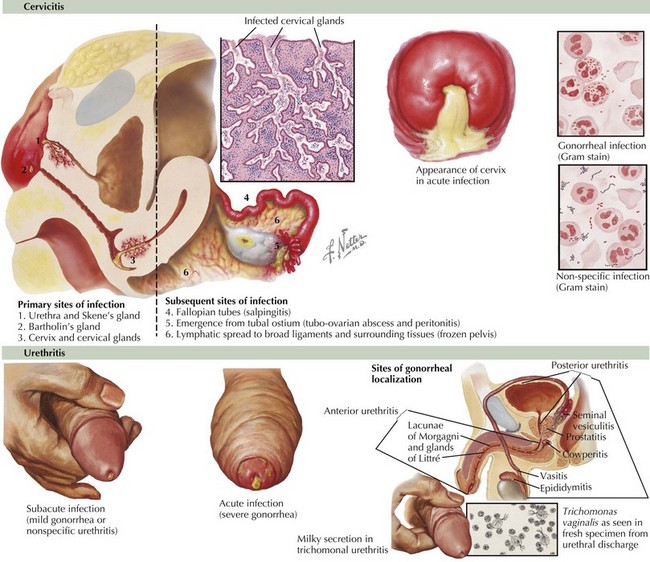
The clinical presentations of urethritis and cervicitis and their associated infections are detailed in Table 89-2 and Figure 89-1.
Pelvic Inflammatory Disease
The presenting symptoms of patients with PID are described in Table 89-2. Some patients may have subclinical infection that is not diagnosed until evaluation for infertility reveals fallopian tube scarring. On examination, patients usually have lower abdominal tenderness. Pelvic examination may reveal cervical discharge; an inflamed cervix; cervical, adnexal, or uterine tenderness; or an adnexal mass. Timely diagnosis of PID is important to prevent infertility. Because the signs and symptoms of infection are not specific, the Centers for Disease Control and Prevention developed criteria to guide diagnosis and empiric treatment (Table 89-3). Fulfillment of minimal criteria indicates presumptive treatment.
Table 89-2 Signs and Symptoms of Urethritis, Cervicitis, and Associated Syndromes in Men and Women
| Men | Women | |
|---|---|---|
PID, pelvic inflammatory disease; RUQ, right upper quadrant.
Table 89-3 Signs and Symptoms of Pelvic Inflammatory Disease
| Minimal Criteria | Additional Criteria | Definitive Criteria |
|---|---|---|
Transvaginal sonography showing thickened fluid-filled tubes, free pelvic fluid, or tubo-ovarian complex |
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; WBC, white blood cell.
Other Manifestations of Gonococcal and Chlamydial Infection
Nongenitourinary manifestations of gonococcal and chlamydial infection include pharyngitis, conjunctivitis, and disseminated infection. Gonococcal pharyngitis should be considered for exudative pharyngitis in a sexually active adolescent. Disseminated gonococcal infection often manifests as arthritis, tenosynovitis, and dermatitis. Chlamydia is associated with Reiter’s syndrome (urethritis, spondylitis, uveitis). Both chlamydia and gonorrhea can also cause neonatal infection (see Chapter 105).
Evaluation and Management
Patients with gonorrhea or chlamydia are at risk for co-infection. Therefore, treatment guidelines recommend covering for both pathogens when treating urethritis, cervicitis, or PID (Table 89-4). This is critical in PID, in which cervical culture results are often negative. Recommendations for PID also include anaerobic coverage because of the polymicrobial nature of the infection.
Table 89-4 Treatment Recommendations for Urethritis, Cervicitis, and Pelvic Inflammatory Disease*
| Treatment | Special Considerations | |
|---|---|---|
| Nongonococcal urethritis or cervicitis | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|