CHAPTER 60 Sexual dysfunction in urogynaecology
Introduction
Sexuality and its expression contribute to some of the most complex aspects of human behaviour. The expression of sexuality and intimacy remains important throughout the lifespan of a woman, and hence needs to be understood in health as well as in illness. Although sexual problems are highly prevalent, a very small proportion of women consult a physician. In a UK- based survey, 54% of women reported at least one sexual problem lasting for at least 1 month during the previous year, which caused 62% of them to avoid sex. Only 21% with problems had sought help, of which 74% consulted their general practitioner (Mercer et al 2003). A web-based survey of 3807 women in the USA revealed that the most important barriers for women to seek help were embarrassment and feeling that the physician would not be able to provide help. Only 42% of this cohort sought help from their gynaecologist (Berman et al 2003). The high prevalence of sexual dysfunction and reluctance of women to seek help is a reflection on physicians’ attitudes and ability to communicate with female patients about their sexual function.
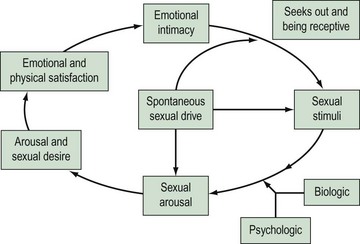
Research into female sexuality has been a neglected area. It was Kinsey’s research in the 1950s on sexual practices in men and women that helped to dispel the myth that women are not interested in sex. However, it has taken a long time to accept that women have a right to sexuality. The advent of new therapies for male sexual dysfunction has led to recent interest in these problems in women. There are a number of reasons why research in the past has focused more on male sexual problems than female. Firstly, it has been difficult to measure appropriate endpoints in clinical trials due to a lack of valid outcome measures. Secondly, the female sexual response is complex, as highlighted by current models (Figure 60.1) compared with the previously described linear models which were based on the relatively uncomplicated male sexual response cycle. The new, non-linear model of female sexual response considers emotional intimacy, sexual stimuli and relationship satisfaction (Basson 2001). This circular model demonstrates that many women initially begin a sexual encounter from a point of sexual neutrality. The decision to be sexual may come from a conscious wish for emotional closeness or as a result of seduction or suggestion from a partner. Women may have numerous reasons for engaging in sexual activity other than sexual drive. Sexual neutrality or being receptive to rather than initiating sexual activity is considered a normal variation of female sexual functioning. In addition, it is frequently the case that subjective and physiological sexual arousal precedes desire.
Definition and Classification
According to the World Health Organization’s International Classification of Diseases (ICD-10) (World Health Organization 1992), the definition of sexual dysfunction includes ‘the various ways in which an individual is unable to participate in a sexual relationship he or she would wish’. On the other hand, in the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) (American Psychiatric Association 1994), female sexual dysfunction (FSD) is defined as ‘disturbances in sexual desire and in the psychophysiological changes that characterise the sexual response cycle and cause marked distress and interpersonal difficulty’. Although both systems recognize the need for a subjective distress criterion, these definitions rely on the linear human response cycle. Furthermore, both systems are based on conceptualization of sexual response as a ‘psychosomatic process’ involving psychological and somatic components. In 1998, the Sexual Function Health Council of the American Foundation devised the first consensus-based definition and classification system for FSD, which was further updated in 2003 (Basson et al 2004) (Box 60.1). FSD is best regarded as a spectrum of disorders with considerable overlap. Understanding this interplay of physical and psychosocial factors in context with illnesses, and medical and/or surgical interventions will help the clinician in managing FSD. Sexual dysfunction may arise because of an illness or disability, a medication or surgical procedure, changes accompanying the ageing process, relationship difficulties, abusive experiences, performance anxiety or any combination of factors such as these (Table 60.1).
Box 60.1 Definition and classification of FSD
Arousal disorder
Table 60.1 Conditions that affect female sexual function and their effects
| Effect(s) | |
|---|---|
| Condition | |
| Oestrogen deficiency e.g. menopause, secondary amenorrhea (binge-eating disorders, rigorous diet), puerperal amenorrhoea (lactational amenorrhoea), contraception with super-light pills, menopause | Decreased lubrication and arousal |
| Testosterone deficiency e.g. premature iatrogenic menopause | Decreased desire |
| Diabetes | Decreased lubrication |
| Hormonal disorders e.g. thyroid, pituitary, adrenal | Decreased lubrication and desire |
| Neurological disorders e.g. Parkinson’s disease, multiple sclerosis | Decreased lubrication, arousal, desire and difficulty reaching orgasm |
| Genital prolapse | Decreased desire and arousal |
| Urinary incontinence | Decreased desire, arousal and pain |
| Atrophy, vaginitis, pelvic inflammatory disease, endometriosis, vestibulitis, cystitis | Pain and vaginismus |
| Arthritis | Limitation of movement |
| Trauma, sexual assault | Arousal disorder |
| Procedure | |
| Oophorectomy | Decreased desire and lubrication |
| Episiotomy and pelvic floor repairs | Pain |
| Drugs | |
| Antihypertensives e.g. β-blockers, α-blockers, diuretics | Decreased desire and difficulty reaching orgasm |
| Psychotherapeutic drugs e.g. tricyclic antidepressants, selective serotonin reuptake inhibitors, lithium, benzodiazepines | Difficulty reaching orgasm |
| Hormones e.g. oral contraceptives, oestrogens, progestins, gonadotrophin-releasing hormone agonists | Decreased desire |
| Cardiovascular agents e.g. lipid-lowering agents, digoxin | Decreased desire |
| Chemotherapeutic agents | Vaginal dryness, decreased desire and difficulty reaching orgasm |
Prevalence of Sexual Dysfunction in Women with Urogynaecological Problems
Sexual dysfunction occurs commonly in women attending urogynaecological services. Up to 64% of sexually active women attending a urogynaecology clinic suffer from FSD (Pauls et al 2006). Although it is a very common problem, a recent survey of members of the American Urogynecologic Society (AUGS) showed that only a minority of urogynaecologists screen all patients for FSD. Lack of time, uncertainty about therapeutic options and older age of the patient were cited as potential reasons for failing to address sexual complaints as part of routine history (Pauls et al 2005). A survey of the members of the British Urogynaecological Society (BSUG) using the same questionnaire with a few modifications reflected similar findings. Fifty percent of the BSUG members regularly screened for FSD at clinic visits and 49.5% after surgery, compared with 77% and 76% of AUGS members, respectively. The most important barrier for not enquiring about FSD was lack of time. Seventy-six percent found training for FSD to be unsatisfactory (Roos et al 2009). The similarity in trends between the UK and USA highlights that this may be a more global problem that needs wider exploration. Furthermore, the subject of FSD should be given more importance in the undergraduate and postgraduate curriculum, so that clinicians enquire about this embarrassing problem.
Aetiology of Sexual Dysfunction in Women with Pelvic Floor Dysfunction
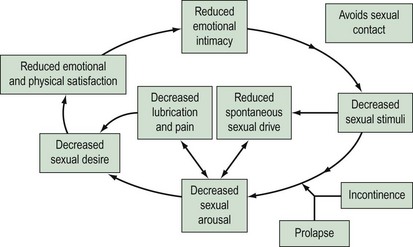
In a survey of 104 patients attending a urogynaecology clinic (Sutherst 1979), 46% admitted that their urinary disorder had an adverse effect on sexual relations. The reasons for reduced frequency of sexual intercourse were superficial or deep dyspareunia (most common), wetness at night and the need for protection of a towel all the time, leakage of urine during coitus, decreased libido, depression or embarrassment, marital discord and the need for separate beds. Women with pelvic organ prolapse may have sexual dysfunction due to mechanical obstruction. However, the reasons probably extend beyond the local effects. It has been shown that women seeking treatment for advanced prolapse have poorer body image and quality-of-life scores compared with women with normal vaginal support (Jelovsek and Barber 2006). Using the female sexual response cycle, one can conceptualize how incontinence and prolapse may affect sexuality. Arousal may be reduced in a woman with coital incontinence or prolapse due to embarrassment. This, in turn, affects orgasm and can also lead to reduced lubrication. Sexual intercourse in this situation will cause the woman to experience pain, which may affect arousal (Figure 60.2).
Relationship between Pelvic Organ Dysfunction and Sexual Function
Evidence from large prospective studies has demonstrated that prolapse and/or incontinence have an adverse effect on sexual function (Rogers et al 2001a, Handa et al 2004, Novi et al 2005). Complaints of stress urinary incontinence, overactive bladder (OAB) and lower urinary tract symptoms have been shown to have a negative impact on all domains of sexual function (Salonia et al 2004, Aslan et al 2005). The most common sexual complaints in women with urinary incontinence are low desire, vaginal dryness and dyspareunia (Handa et al 2004). Amongst the different types of urinary incontinence, OAB has a particularly high association with sexual dysfunction, which could be indicative of an underlying psychosomatic disorder.
Using a validated questionnaire, Novi et al (2005) demonstrated significantly lower measures of sexual function in women with pelvic organ prolapse. Women with prolapse were more likely to have urinary and/or faecal incontinence during sexual activity, more dyspareunia and fewer orgasms. They were also more likely to report negative emotional reactions associated with sex, and higher rates of embarrassment leading to avoidance of sex. Presence of both prolapse and incontinence has a cumulative negative effect on sexual function, with libido, sexual excitement and orgasm being significantly affected (Ozel et al 2006). Increasing severity of prolapse is associated with symptoms related to urinary incontinence, voiding, and defaecatory and sexual dysfunction, which do not necessarily correlate with the location of prolapse and therefore are not compartment specific (Ellerkmann et al 2001).