Analgesic
Relieves pain by altering perception of nociceptive stimuli
Sedative
Decreases activity, moderates excitement and calms patient
Anxiolytic
Relieves apprehension and fear due to anticipated act or illness
Amnestic
Affects memory; patient is unable to recall events after delivery of drug
Hypnotic
Produces drowsiness and aids in the onset and maintenance of sleep
Table 2
Levels of sedation
Minimal | Moderate | Deep | General anesthesia | |
|---|---|---|---|---|
Cognitive function | Normal to partially impaired | Partially to fully impaired | Fully impaired | Fully impaired |
Responsiveness | Normal response to verbal commands | Purposeful response to verbal commands and/or light touch | Purposeful response to painful stimulation | No response to stimulation |
Airway patency | Normal | May require intervention | Occasionally require intervention | Often require intervention |
Spontaneous breathing | Normal | Normal to adequate | May be impaired | Often impaired |
Cardiovascular function | Normal | Normal | May be impaired | Occasionally impaired |
3.
Pre-Sedation Assessment:
(a)
History:
(i)
A general history of each child should be known prior to administering sedative and analgesic medications. Important historical information that may impact the choice of medications administered is summarized in Table 3.
Table 3
Pre-sedation assessment
Active medical issues |
Current medications |
Known allergies |
Known adverse reactions to medications |
Previous history of sedation or anesthesia and any complications |
History of significant snoring or apnea |
Known anatomic limitations to opening mouth or moving head and neck |
Loose teeth or presence of dental devices |
Time since last oral or enteral intake |
Recent illnesses (fever, upper respiratory infection, etc.) |
Family history of problems with sedation or anesthesia |
Table 4
NPO guidelines
Food | Hours of NPO |
|---|---|
Clear liquids | 2 |
Breast milk (infants) | 4 |
Formula or light meal | 6 |
Full meal | 8 |
(b)
Physical Exam:
(i)
A focused physical exam should include assessment of vital signs, cardiopulmonary function and baseline neurological status.
(ii)
Airway.
1.
The pediatric airway is anatomically different than the adult.
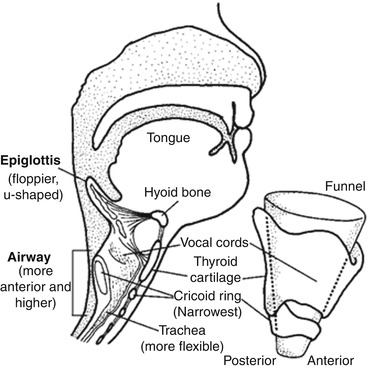
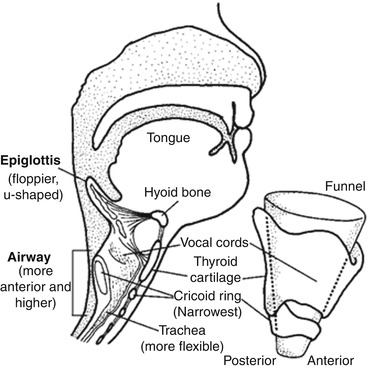
Fig. 1
Pediatric airway, as compared to the adult. The narrowest part of the pediatric airway is the cricoid ring (Included with permission from Susan Gilbert as published at http://www.medartist.com/emergency_pediatrics.html. Downloaded 28 Apr 2013)
2.
A child’s tongue is relatively larger compared to the space it occupies in the oropharynx.
(a)
Children with macroglossia, micrognathia or retrognathia may have even more limited space relative to the oropharynx.
3.
Larynx is more anterior and superior.
4.
Relative to adult’s epiglottis, a child’s is longer, more narrow and more floppy.
5.
Children younger than 8-years-old have the narrowest part of their upper airway located in the subglottic region at level of cricoid cartilage.
(a)
Any obstruction in this area will significantly impair airflow.
(b)
When supine, care should be taken to ensure the airway remains aligned and excess flexion or extension of the neck does not occur.
6.
A roll under the neck and/or shoulders should be utilized to create a “sniffing” position, whereby the horizontal plane of the ears (with patient lying supine) is anterior to the shoulders
7.
Mallampati classification may be performed to assist in predicting a difficult intubation but has not been shown to affect risk stratification for children undergoing procedural sedation.
(iii)
In addition to the airway assessment, attention should be paid to any physical attributes the child may have that would put him/her at risk for complications, such as:
1.
Obesity or failure to thrive.
2.
Scoliosis or other skeletal abnormalities.
3.
Baseline neurologic impairment.
(iv)
A brief examination of the chest with auscultation of lungs and heart should be performed.
(v)
After completion of physical exam, assignment of ASA score may be helpful in stratifying the child’s relative risk of sedation (Table 5)
Table 5
ASA classification
ASA Classification | |
ASA I | Normal healthy patients |
ASA II | Patients with mild systemic disease |
ASA III | Patients with severe systemic disease that is limiting but not incapacitating |
ASA IV | Patients with incapacitating disease which is a constant threat to life |
ASA V | Moribund patients not expected to live more than 24 h |
ASA VI | A declared brain dead patient whose organs are being removed for donor purposes. |
4.
Intra-procedure:
(a)
Informed consent must be obtained for all sedated procedures.
(b)
A time out should occur prior to administering any medications or starting the procedure.
(i)
Monitoring and equipment.
1.
All children undergoing sedation to facilitate invasive or non-invasive procedures require continuous cardiopulmonary monitoring including pulse oximetry.
2.
Capnography, a tool that measures exhaled CO2, can be very useful in monitoring airway patency and ventilation in the sedated child.
3.
Get Clinical Tree app for offline access

The mnemonic SOAPME can help the provider ensure he/she has the appropriate equipment in place prior to starting the procedure.



