Fig. 6.1
Normal saline infusion sonohysterography (SIS). (a) Sagittal view. (b) 3D rendering
Supporting Data
When compared to traditional two-dimensional (2D) transvaginal sonography, SIS has been found in numerous studies to be superior in the detection of endometrial abnormalities. For example, a prospective study comparing the accuracy of TVUS and SIS in pre and postmenopausal women with abnormal uterine bleeding reported that the sensitivity and specificity of SIS for the detection of endometrial pathologies were significantly higher than that of transvaginal ultrasound (98 % and 93 %, respectively, for SIS versus 83 % and 71 % for TVUS) [7]. SIS is particularly useful in diagnosing focal endometrial abnormalities and intracavitary masses such as endometrial polyps and fibroids. In the above mentioned study, the sensitivity and specificity of SIS in the detection of endometrial polyps were 100 % and 92 %, and in the case of fibroids were 95 % and 100 %, respectively. Another prospective study of a similar patient population compared the detection of polyps and fibroids using these two techniques. This study found that the sensitivity and specificity of SIS for polyps were significantly higher than TVUS (91 and 93 % for SIS versus 65 and 88 % for TVUS) [8]. The sensitivity and specificity for the detection of fibroids between the two techniques were similar in this study (92 % and 99 % for SIS versus 96 % and 95 % for TVUS), although other studies have demonstrated a small advantage of SIS over TVUS for the detection of myomas [6, 9]. The clear visual advantage of SIS for the detection of polyps and fibroids can be seen in Figs. 6.2, 6.3, and 6.4. Figure 6.2 illustrates the typical appearance of a polyp during SIS, while Figs. 6.3 and 6.4 demonstrate leiomyomas. Numerous studies confirm that SIS improves the diagnostic utility of standard 2D transvaginal sonography [2, 6–8, 10].
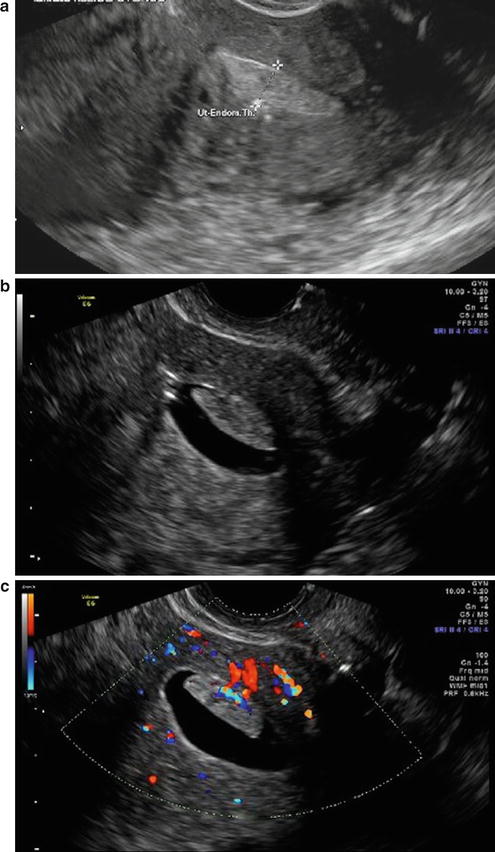
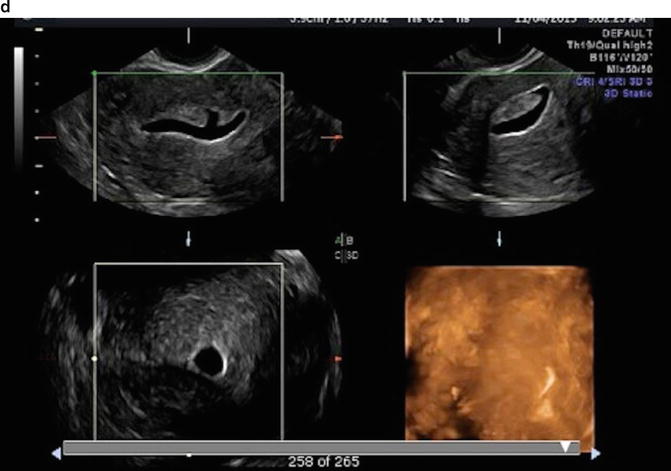
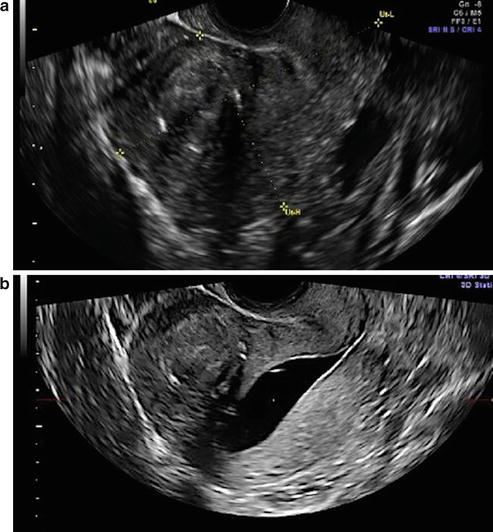
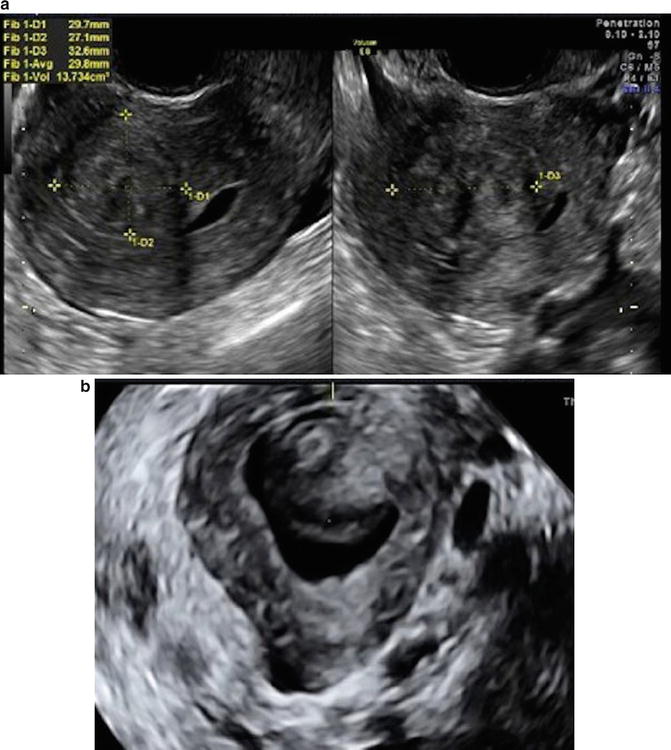
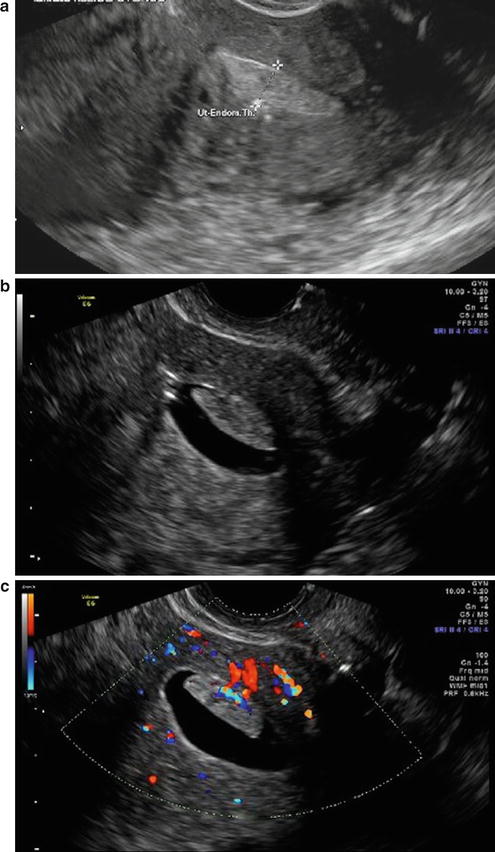
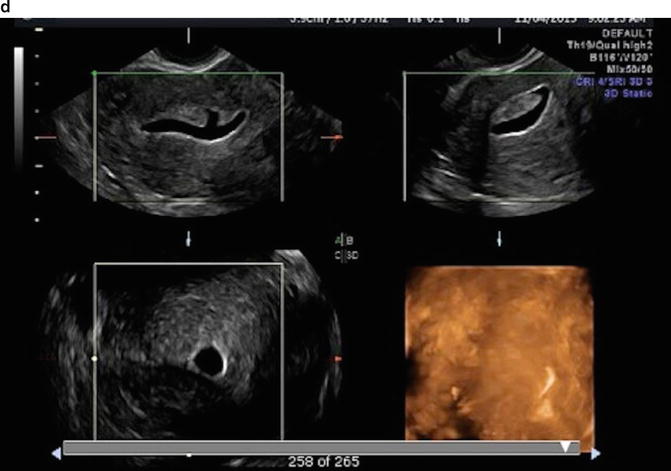
Fig. 6.2
Polyp in a perimenopausal woman with menorrhagia. (a) Standard 2D transvaginal imaging shows a thickened endometrial stripe. (b) SIS shows a 2 × 2 cm lesion of the anterior endometrium. (c) Color Doppler imaging shows flow within the lesion that is typical of a polyp. (d) 3D imaging of the endometrial cavity demonstrate two polyps on transverse view that were not apparent on original longitudinal view
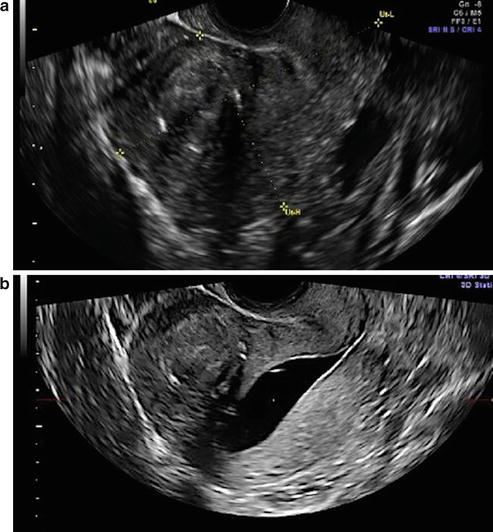
Fig. 6.3
Fibroid in a 38-year-old woman with infertility. (a) Gray scale images demonstrate a fibroid of the anterior uterus. (b) Instillation of saline demonstrates that the fibroid is intramural without distortion of the endometrial cavity. This fibroid is unlikely to interfere with implantation or pregnancy
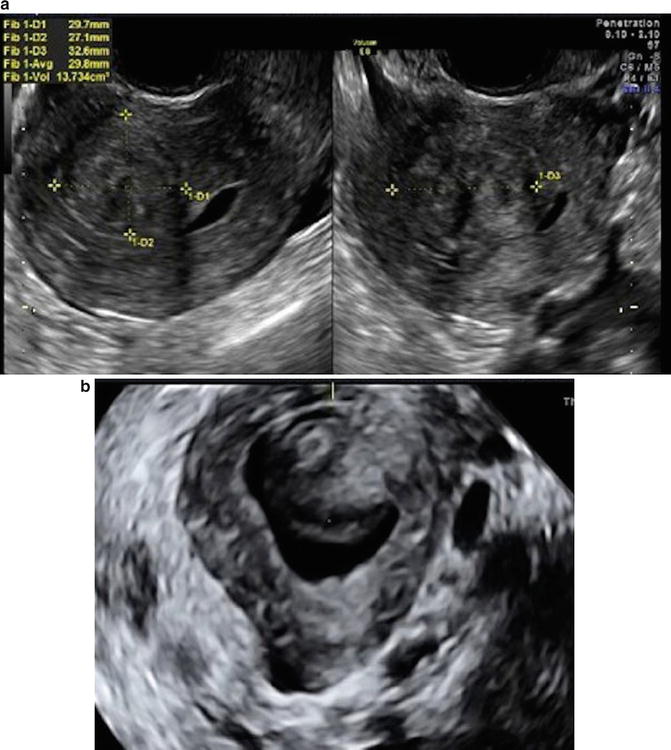
Fig. 6.4
Fibroid in a 34-year-old woman with dysmenorrhea and menorrhagia. (a) Gray scale images of 3 cm anterior myoma. (b) Saline sonohysterography reveals an intracavitary myoma. This fibroid was removed hysteroscopically with complete resolution of symptoms
It has been suggested that SIS may also serve as an alternative to HSG. HSG is often used to simultaneously evaluate the uterus and fallopian tubes. HSG is superior to SIS in the detection of tubal abnormalities, as nonpathologic fallopian tubes are not visualized ultrasonographically. While SIS can reliably identify tubal spill, all that can be concluded from the finding of free fluid on endovaginal ultrasound after SIS is that at least one of the fallopian tubes is patent. Recent adaptations to improve tubal evaluation during ultrasound include the instillation of either air bubbles or echogenic contrast media rather than saline (hysterosalpingo-contrast sonography [HyCoSy]) [11]. Although HSG remains the gold standard for evaluation of tubal pathology, SIS has higher accuracy than HSG in the detection of uterine anomalies, in particular septate and bicornuate uteri (100 % versus 81 % for HSG) [12]. The ability to assess fundal contour in the evaluation of uterine anomalies is a valuable addition provided by sonography as compared to HSG, especially when combined with 3D ultrasound images. SIS is also superior to HSG in the diagnosis of polyps and endometrial hyperplasia [13]. Both HSG and SIS have limited accuracy in diagnosing intrauterine adhesions, with high false positive rates from blood clots, shearing of normal endometrium, and mucus plugs [14]. Such uterine synechiae as visualized on SIS in a patient with Asherman’s Syndrome are shown in Fig. 6.5. Some authors have reported additional advantages of SIS which make it an appealing choice over HSG, including decreased patient discomfort, less expense, the absence of radiation exposure, and its availability in an office setting [12, 13].
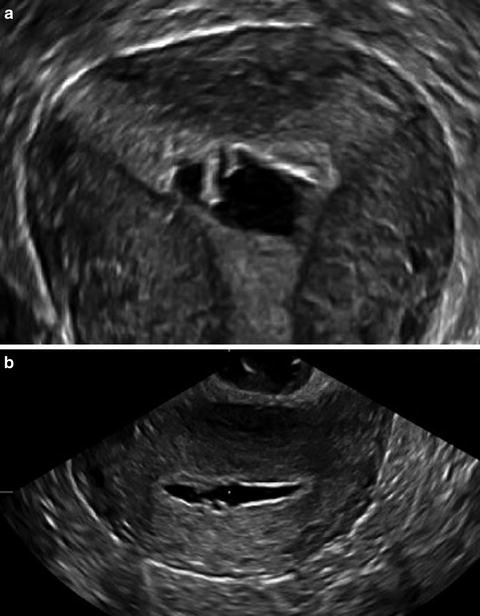
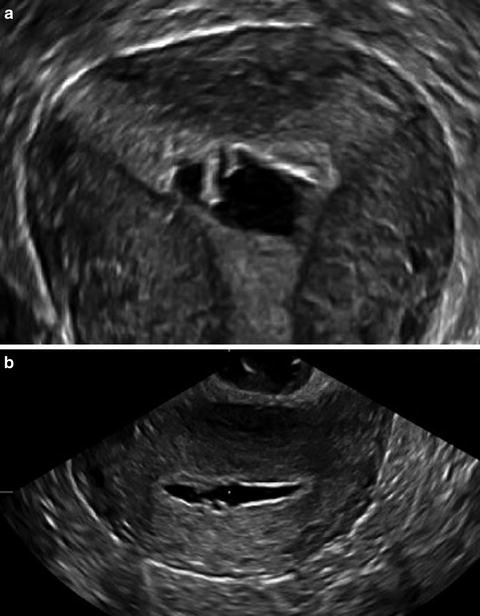
Fig. 6.5
Asherman’s Syndrome in a patient with multiple intrauterine procedures. (a) Saline sonohysterography shows echogenic foci within the endometrium. (b) 3D SIS demonstrates intrauterine adhesions at the right cornual region of the uterus
Diagnostic hysteroscopy with endometrial biopsy is the gold standard to evaluate uterine cavity abnormalities [6]. However, office hysteroscopy is expensive, invasive, and causes more discomfort to the patient than SIS [15, 16]. Additionally, hysteroscopy cannot visualize the myometrium and therefore cannot classify the depth of myometrial invasion of leiomyomas or carcinoma as SIS can [17]. In direct comparisons, the diagnostic accuracy for polyps, endometrial hyperplasia, and submucosal myomas with SIS has been found to be equivalent to hysteroscopy [6]. Several studies have reported that in patients with abnormalities on transvaginal ultrasound, SIS use, first-line was preferable to proceeding directly to hysteroscopy, as the latter could be avoided in 72–88 % of patients who could then be managed conservatively [4, 17, 18]. More support for this triaging method is reported in a study on cost-effectiveness which indicates that SIS as an initial screening procedure is superior to first-line diagnostic hysteroscopy [19]. Another set of authors stated that diagnostic hysteroscopy should be reserved for situations where SIS is either inconclusive or not feasible [20].
In conclusion, SIS is a safe, simple, inexpensive procedure with few side effects. It is well tolerated by patients, and it can easily be performed in the office setting [21] without the need for an operating room, extra personnel, anesthesia, or exposure to radiation. Distention of the uterine cavity with saline clearly improves upon traditional 2D transvaginal sonographic imaging of the uterine cavity, endowing SIS with greater sensitivity and specificity for the detection of endometrial pathologies. SIS is superior to HSG for the detection of uterine anomalies, and new adaptions may help SIS to overcome its longstanding inferiority to HSG in tubal evaluation. SIS is less invasive than hysteroscopy, and is cost-effective as a screening test prior to more invasive methods in investigating patients with abnormal or inconclusive transvaginal sonographic results [3, 8, 22].
Indications and Contraindications
SIS is indicated when the etiology of a woman’s symptoms is suspected to arise from an abnormality of her endometrium or uterine cavity, and it can be useful in other situations when transvaginal ultrasound is inadequate [23, 24]. Specifically, indications for SIS include, but are not limited to, evaluation of the following:
Abnormal uterine bleeding
Infertility
Recurrent pregnancy loss
Congenital abnormalities of the uterus
Evaluation of uterine cavity polyps, myomas, and synechiae
Abnormalities on transvaginal ultrasound, including focal or diffuse endometrial or intracavitary abnormalities
Absolute contraindications to SIS include pregnancy, pelvic infection, and unexplained pelvic tenderness [23, 24]. SIS can be performed during menses as active bleeding is not a contraindication. However, heavy menstrual bleeding may make interpretation of the study more difficult, as blood clots are known to cause false positive examinations [23].
Although not a contraindication, a concern exists regarding sonohysterography for the patient in whom there is high suspicion of endometrial carcinoma. In this situation, there is the potential risk of disseminating malignant cells into the pelvic cavity via transtubal spill of saline. Two prospective studies performed in women with endometrial cancer found malignant or suspicious cells from SIS in 25 % of cases [25, 26]. During surgical staging for endometrial cancers, the presence of malignant cells in peritoneal washings significantly increases the stage of disease. Both of the aforementioned studies concluded that SIS should not be performed in this population of women due to the risk of malignant cell dissemination. However, other studies have found the risk of cancer cell dissemination during this procedure to be smaller, with positive cancer cells after transtubal spill in only 2–12.5 % of patients [27, 28]. These studies concluded that SIS has a low probability of cancer cell dissemination. In addition, it is unclear whether positive peritoneal washings due to SIS have the same prognostic value as typical positive peritoneal cytology encountered in endometrial cancer staging. We encourage the clinician to consider this area of controversy prior to performing SIS in populations of women at high risk for endometrial cancer, such as in women with postmenopausal bleeding. Figure 6.6 illustrates a thickened endometrium found during SIS in just such a patient with postmenopausal bleeding.
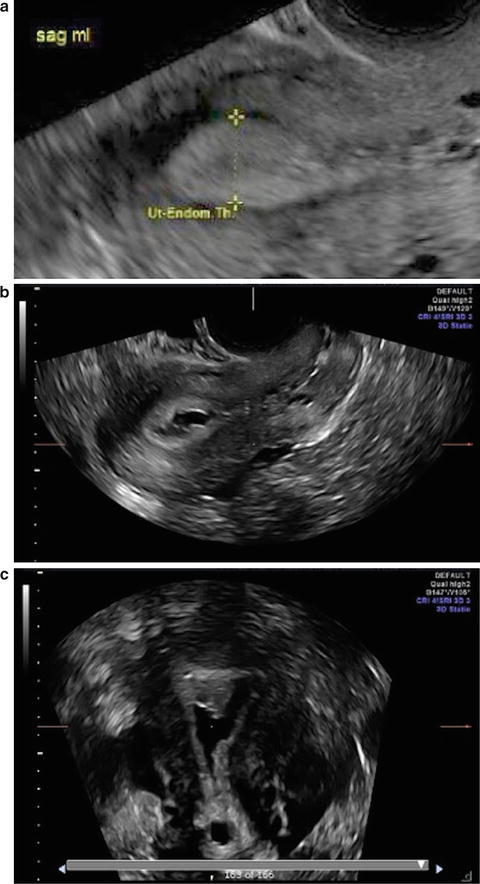
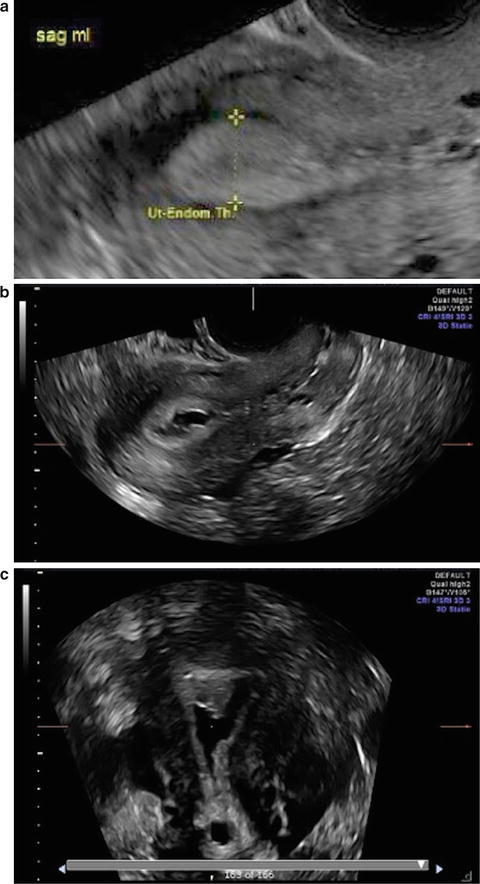
Fig. 6.6
Thickened endometrium in a patient with postmenopausal bleeding. (a, b) 2D images with and without saline demonstrate areas of irregular endometrial thickening. (c) 3D SIS shows with a focal area of thickening in the right fundus. The lesion was removed hysteroscopically and pathology confirmed a benign intrauterine polyp
Equipment
One of the advantages of SIS is the minimal amount of equipment needed. Although many types of transcervical catheters have been proposed of various complexities, all can be effective in experienced hands [29]. The cost for specialized catheters can vary, with the most expensive approaching $100. However, even a pediatric Foley catheter, the least costly option, can be used to instill fluid into the endometrium and provide good quality images if needed. The major difference between catheters is the presence or absence of an intrauterine balloon; when inflated and positioned at or in the cervix, the balloon can prevent loss of distending fluid from the uterus. In some cases, such as the multiparous cervix, the balloon is especially useful; however, it should be noted that most studies also associate balloon use with increased discomfort during the procedure [29, 30]. Beyond the transcervical catheter, a 20–30 mL syringe with sterile saline or sterile water, a speculum and light source as well as a ring forceps or uterine forceps to assist in placement of the catheter are all necessary. Lastly, a high frequency transvaginal US probe and high resolution ultrasound machine are required to perform SIS. A cervical dilator probe and/or a single tooth tenaculum may be used in cases where passage of the catheter is difficult.
Three-dimensional (3D) sonohysterography is a useful tool to increase the sensitivity for intrauterine lesions [31] and assist in more fully evaluating Mullerian anomalies. 3D SIS does require special training other than having an ultrasound machine with 3D capabilities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


