Joseph C. Gambone

What Is Quality Care?
It has been more than a decade since the Institute of Medicine (IOM) published two seminal works in the fields of patient safety and medical care quality: To Err Is Human and Crossing the Quality Chasm (1,2). Despite the heightened awareness and increased public focus on the crucial issues raised by these publications, there is limited evidence of significant progress toward making this country’s health care both safer and better (3). One reason for this absence of momentum may be the very gradual incorporation of an emphasis on the principles of patient safety during medical school and residency. Leaders in the patient safety movement have called for the redesign of education for health care professionals in order to equip these individuals with the essential knowledge, skill, and attitude required to function safely and effectively in the health care delivery environment of the 21st century. Although this imperative affects all health professions, it is particularly compelling in medical education because physicians’ actions and decisions indicate parameters for the care that most other health care professionals provide (4).
The IOM defined quality as “the degree to which health services for the individual and populations increase the likelihood of desired health outcomes . . . consistent with current professional knowledge” (5). Of note in this assertion is the recognition that health care quality is important and applicable to entire groups of people, as well as to every single patient. Implicit is the obligation to be sensitive to the flexible meaning of “desired health outcomes,” because desired outcomes may differ from the perspective of hospitals, physicians, patients, and their families. Adherence to the definition includes rigorous application of accepted standards of information and treatment to any clinical problem, a process now referred to as evidence-based medical practice (6).
Another construct to define and achieve higher quality health care can be derived from the “Five Rights” of medication administration: right patient, right drug, right dose, right time, and right route (7). The Five Rights of medical quality could be thought of as doing the right thing for the right patient at the right time; doing it right the first time; and doing it right for every patient (8).
The concepts embodied in these two statements are elegantly incorporated into the IOM’s six “Aims for Improvement” that are articulated in Crossing the Quality Chasm and listed in Table 3.1 (The Six Aims) (2). It is notable that “Safe” is listed first. Safety has always been considered “first among equals” in the hierarchy of physicians’ responsibilities. This was initially understood as an admonition to individual medical practitioners. However, it is now recognized that fulfilling this promise of safety requires conscientious evaluation and careful renovation of the systems that deliver medical care.
Table 3.1 Six Aims for Quality Health Care
| Care should be: | |
| Safe (First among equals) | Timely |
| Effective | Efficient |
| Patient-centered | Equitable |
Clinical Variation
Each patient receiving an identical diagnosis might not be given the same treatment. This is known as clinical variation, and can be broadly categorized as falling into two types. One is necessary clinical variation, an alteration in medical practice that is required by the differing needs of individual patients. This modification may be in response to differences in the patients themselves, because of age, overall health status, or other clinical characteristics; or it may be caused by differing desired outcomes as part of a patient-centered approach to care (8). This kind of variation is expected in any system of care. The other type is unexplained clinical variation, which comprises differences in medical care and patient management that are not accounted for by differences in patient symptoms, objective findings, or patients’ goals for care. These treatment discrepancies could account for wide variations in the cost of care without any demonstrable difference in outcomes as measured by morbidity or mortality (9–11). Often this unexplained variation is the result of management choices made by physicians in cases that fall into so-called clinical gray areas, where no single course is clearly correct. Sometimes this variation is both unexplained and unintended. It is this unexplained or unintended variation that is considered one of the greatest barriers to the delivery of consistently high-quality care (12). The specialty of gynecology is subject to this treatment inconsistency. Significant geographic variations in hysterectomy rates, largely unexplained by the clinical characteristics of those local populations, were reported (11,13). Further study and reduction of unnecessary variation in these rates could contribute to making medical care more efficient and equitable.
Role of Organizational Leadership
Creating a safe environment for the delivery of medical care requires the active participation of organizational leadership. Each physician assumes a significant responsibility for safety and excellent care in his or her own practice environment. In the hospital, oversight for issues of safety and quality is shared by the hospital board, executive leadership, and physicians who serve as chief medical officer, vice president of medical affairs, or department chairs. A new position being adopted by many hospitals is the patient safety officer (14). This individual takes direct responsibility for overseeing all aspects of the hospital patient safety program and reports to the hospital chief executive officer or board of directors. It is an emerging role for physicians who want to make patient safety the focus of their professional lives.
An integral part of promoting patient safety is the creation of an organizational culture where patient safety is recognized as everyone’s responsibility. Culture in an organization is “the way we do things around here” mindset, and it reflects the attitude of the members of the organization toward what is important and how that fits into the structure of their activities (15). The first step in creating a culture of safety is to measure a starting point for both nursing and physician staff regarding the attitudes and perceptions around patient safety. This can be accomplished using any of several validated tools such as a safety attitude questionnaire or hospital survey on patient safety culture (14). Once areas of deficiency are identified, steps can be taken to improve culture by direct interaction with frontline clinicians to ascertain appropriate changes to the clinical environment to promote safety. This can be done through regular safety meetings or direct observation of the workplace with Executive WalkroundsTM (16).
Another method for improving the safety climate in a hospital is the adoption of the tenets of “Just Culture” (17). Just Culture recognizes that human error cannot be eliminated from any complex system such as health care. People sometimes make mistakes. They can be held accountable for following procedural rules to reduce harm to patients resulting from human error. Adverse outcomes and near misses allow the organization to examine its processes of care with an eye to continuous improvement. With such a system in place, the reporting of safety problems and concerns will often increase dramatically. This in turn allows the hospital or other health care organization to initiate programs to address these issues and to make “first, do no harm” a reality.
Communication
In an assessment of the factors leading up to serious adverse events in hospitals, communication problems were the most frequently identified root cause, occurring in almost three-fourths of cases (18). Assuring clear and timely communication between all caregivers is perhaps the single most important measure to improve the safety and quality of medical care. In the health care setting, structured communication techniques are referred to under the title “team resource management.” The basic principle of team resource management is to foster an atmosphere where individuals with different roles are brought together to achieve a successful outcome to a complex operation (19). Despite differing roles, training, and ranking within a perceived hierarchy, and the fact that some individuals may not have worked together as a team before, it is understood that each participant has an overarching responsibility. That responsibility is to communicate with all team members whenever they see anything that is potentially unsafe or when other team members are not acting appropriately in a given situation. This concept is particularly applicable in the operating room, by nature a highly complex environment. Everyone present—physicians, nurses, house staff, and technicians—must keep patient safety foremost in their minds. No one should be hesitant to raise questions and concerns when an unsafe situation is observed.
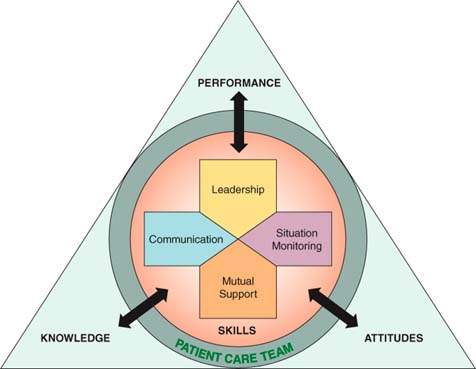
There are excellent formalized systems to train health care providers in this important skill (19). One of the most comprehensive and well-recognized systems is Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS), a joint project of the Agency for Health Care Research and Quality and the Department of Defense (20). The TeamSTEPPS logo (Fig. 3.1) is a visual model representing the four basic teamwork skills of leadership, communication, situational monitoring, and mutual support. The program teaches how the interaction of these skills produces the three desired team outcomes for knowledge, attitudes, and performance, and how these outcomes further reinforce those skills in a reciprocal manner. TeamSTEPPS includes the principles of team resource management, as well as many specific techniques for effective communication. One of the most useful is represented with the acronym SBAR: Situation, Background, Assessment, and Recommendation (or Request) (21). It is a structured method for relaying information about a changing clinical situation. The initiator of the exchange gives a brief description of the clinical change or concern that is prompting the communication. This is followed by the clinically relevant background information about the patient. The initiator then gives his or her assessment of what he or she thinks is happening with the patient and makes a recommendation or request for action by the other party. It is frequently used by nurses to update on-call physicians about a patient’s clinical status, but can also be used between residents and attending physicians or any other pair of providers where concise, clear communication is required.
Figure 3.1 The TeamSTEPPS program logo. (From Team STEPPS Program of the U.S. Agency for Healthcare Research and Quality [AHRQ]).
Certain situations in health care are particularly prone to miscommunication. One example is during the stress of emergency situations, when a physician may be rapidly giving orders for medications, blood transfusions, or procedures to be initiated. A technique referred to as “call-outs” helps ensure that critical orders are received correctly. The person to whom the verbal order is directed repeats the order verbatim to acknowledge he or she has received it and will be responsible for carrying it out. Hearing this call-out assures the ordering physician that the order was received, who will be performing it, and allows an opportunity to correct the order if it was misheard. Similarly, telephone orders are well known to be sources of misinterpretation of physicians’ treatment intentions (22). Check-back is a technique to minimize errors in this medium. In a typical situation, a doctor calls a nurse to order a medication for a patient. Check-back has three components. First, the physician gives the medication order to the nurse. Second, the nurse repeats the order back to the physician, specifying medication name, dose, route, and timing of administration. Lastly, the physician confirms back to the nurse that the order was correctly received. A handoff of a patient from one physician to another is a third opportunity for miscommunication. This relay team approach to care is occurring more frequently in medical education as a result of residency work-hour restrictions (23). To minimize errors in this setting, it is wise to use a structured script for communicating critical clinical information. One such script from the TeamSTEPPS program is the mnemonic I PASS the BATON, which is essentially a checklist of clinical items to be related to the person assuming the care of the patient (Fig. 3.2) (19). The key point is that management handoffs should be a formal process that does not rely on memory to convey crucial information.
Figure 3.2 I PASS the BATON. (From Team STEPPS Program of the U.S. Agency for Healthcare Research and Quality [AHRQ]).

An important feature of team resource management is the ability of any team member to “stop the line”; that is to halt the process or procedure when they feel a risk to patient safety is present. One recommended technique is the “CUS” method. This acronym represents three possible sets of “code words” that any team member may articulate to indicate that the procedure must stop until the safety concern is addressed. The letters in the acronym stand for “I’m Concerned”; I’m Uncomfortable”; and “I have a Safety concern.” Another method is the “Two-Challenge Rule.” This indicates that when a team member has a safety concern he or she should bring it to the attention of the physician in charge of the procedure in question. If the concern is not acknowledged or adequately addressed, the team member should address it a second time. If the concern is still unanswered or uncorrected, the team member is then obligated to go up the chain of command to a supervisor or higher-ranking physician to have his or her concerns satisfied.
All of these techniques can contribute to a safer environment for patient care in the operating room, emergency department, and on patient floors. However, none of them can be very effective without practice. The use of drills and simulations to rehearse these techniques in mock emergency situations is well established in anesthesia training programs (24,25). The use of simulators to teach basic surgical techniques including laparoscopy and robotic surgery are becoming more common (26–28). Drills and rehearsals for emergency situations improve outcomes and enhance safety (29–31).
Infection Control
Hospital-acquired infections are one of the most common causes of morbidity in hospitalized patients (32). Reducing the incidence of these infections, and preventing their spread to other patients, should be a top priority for all health care providers.
Surgical site infections result in an increased length of stay for surgical patients, with all the attendant associated risks and increased costs (33). While not preventable 100% of the time, their incidence can be significantly reduced. There are many operating room techniques available to accomplish this, and they should be used consistently (34). These include avoidance of shaving of the operative site, appropriate antimicrobial skin preparation, preoperative hand antisepsis, use and correct timing of administration of antibiotic prophylaxis, and observance of sterile technique.
In addition to preventing the occurrence of infection, it is equally important to prevent transmission of infection from one patient to another. One of the most effective, but widely underutilized techniques is simple hand washing. The effectiveness of hand washing in the prevention of disease transmission was first demonstrated by Ignac Semmelweis in the obstetrical wards of Vienna in the 1840s (35). Despite having this knowledge for over 150 years, compliance with hand-hygiene techniques in the hospital setting remains poor (36). Hand washing using appropriate technique before and after every patient encounter should be considered mandatory. Beyond this basic technique, certain infections require special precautions to prevent transmission, known as isolation techniques (37). These involve combinations of masks, gowns, and gloves to prevent contact with infected skin, body fluids, or airborne particles. It includes special handling of trash, linens, and environmental surfaces. The level of precautions to be taken will be determined by the hospital’s infection control personnel. The key point is to adhere rigorously to the isolation instructions posted outside the patient’s room.
Operating Room Safety
The operating room is by its nature a highly complex health care environment. It is a potential site for adverse events, which can be catastrophic. These include wrong patient surgeries, wrong site surgeries, and retained foreign objects. All of these occur in hospitals, despite recognition that these events should never take place (38,39). The Joint Commission, a national accrediting body for hospitals, has developed the Universal ProtocolTM that all surgeons and operating rooms should follow (40). There are three major components of the Universal Protocol. First is to conduct a preprocedure verification process that confirms the identity of the patient and his or her understanding of what procedure is to be performed. Second is marking of the operative site by the surgeon, which is especially critical in cases involving bilateral structures. This is to be done in the preoperative area with the patient awake as a confirmation of accuracy. Third is the performance of a surgical “time out” in the operating room prior to the start of the surgery to confirm the correct patient identity and correct planned procedure. Failure to perform any of these steps increases the risk of performing the wrong operation on the wrong patient.
The traditional use of checklists resulted in dramatic increases in the safety of aviation (41). Their use in medicine is recent but is demonstrated to decrease complications significantly when used consistently to verify that procedural steps are not overlooked. A simple five-step checklist for central-line placement in the intensive care unit was shown to reduce the incidence of catheter-related sepsis almost to zero (42,43). Similarly, checklists are advocated for use in the surgical suite to ensure that critical steps for error prevention and patient safety are not overlooked. The World Health Organization (WHO) released a surgical checklist in 2009 under their “Safe Surgery Saves Lives” program (44). It involves items to be reviewed and documented before the induction of anesthesia, before the skin incision, and before the patient leaves the operating room. Use of the WHO checklist was shown to reduce major complications of surgery from 11% to 7% and the inpatient death rate from major surgery from 1.5% to 0.8% (45). The use of checklists such as this to improve patient safety in the operating room should become more widespread.
The inadvertent retention of foreign bodies such as sponges, instruments, or other objects at the conclusion of surgery is a continuing source of patient harm. Risk factors associated with retained foreign bodies are emergency surgery, an unexpected change in surgical procedure, high patient body mass index, and failure to perform sponge and instrument counts (46). Systems must be established to prevent these occurrences, and surgeons need to aware of the contributing risk factors listed above (47). The most commonly retained item is a surgical sponge. Strict adherence to guidelines for tracking surgical sponges is necessary to reduce the incidence of this serious complication. One comprehensive program to assist in this adherence is called “Sponge Accounting” (48). It involves standardized counting and recording of sponges at the start of the case and as additional sponges are added to the surgical field. At the conclusion of the surgery, all sponges are placed in special transparent holders to allow visual confirmation that all sponges were taken out of the patient. Other systems employ radiofrequency tagging of all sponges so that retained sponges can be detected easily before the surgical wound is closed (49).
Table 3.2 Examples of Dangerous Abbreviations and Dose Expressions
| Abbreviation/Dose Expression | Intended Meaning | Misinterpretation |
| AU | Aurio uterque (each ear) | Mistaken for OU (oculo uterque-each eye). |
| D/C | Discharge, discontinue | Premature discontinuation of medications when D/C (intended to mean “discharge”) has been misinterpreted as “discontinued” when followed by a list of drugs. |
| μg | Microgram | Mistaken for “mg” when handwritten |
| o.d. or OD | Once daily | Misinterpreted as “right eye” (OD-oculus dexter) and administration of oral medications in the eye |
| TIW or tiw | Three times a week | Mistaken as “three times a day” |
| per os | orally | The “os” can be mistaken for “left eye” |
| q.d. or QD | every day | Mistaken as q.i.d., aspecially if the period after the “q” or the tail of the “q” is misunderstood as an “i” |
| qn | Nightly or at bedtime | Misinterpreted as “qh” (every hour) |
| qhs | Nightly at bedtime | Misread as every hour |
| q6PM, etc. | Every evening at 6PM | Misread as every 6 hours |
| q.o.d. or QOD | Every other day | Misinterpreted as “q.d.” (daily) or “q.i.d.” (four times daily) if the “o” is poorly written |
| sub q | Subcutaneous | The “q” has been mistaken for “every” (e.q., one heparin dose ordered “sub q 2 hours before surgery” misunderstood as every 2 hours before surgery) |
| SC | Subcutaneous | Mistaken for SL (sublingual) |
| U or u | Unit | Read as a zero (0) or a four (4), causing a 10-fold overdose or greater (4U seen as “40” or 4u seen as 44”) |
| IU | International unit | Misread as IV (intravenous) |
| cc | Cubic centimeters | Misread as “U” (units) |
| ×3d | For 3 days | Mistaken for “three doses” |
| BT | Bedtime | Mistaken for “BID” (twice daily) |
| ss | Sliding scale (insulin) or ½ (apothecary) | Mistaken for “55” |
| > or < | Greater than or less than | Mistakenly used opposite of intended |
| / (slash mark) | Separates two doses or indicates “per” | Misunderstood as the number 1 (“25 unit/10 units”) read as “110” units |
| Name letters and dose numbers run together (e.g., Inderal 40 mg) | Inderal 40 mg | Misread as Inderal 140 mg. |
| Zero after decimal point (1.0) | 1 mg | Misread as 10 mg if the decimal point is not seen |
| No zero before decimal dose (.5 mg) | 0.5 mg | Misread as 5 mg |
Modified from Reiter RC, Yielding L, Gluck PA. Clinical performance improvement: assessing the quality and safety of women’s health care. In: Hacker NF, Moore JG, Gambone JC, eds. Essentials of obstetrics and gynecology, 4th ed., Philadelphia: Elsevier/Saunders, 2004:52, with permission. | ||
Application of Safety Technology
Computerized physician (prescriber) order entry system (CPOE) is a prescription ordering system where the prescriber enters ordering information directly into a computer. Some of the more sophisticated systems can check for errors and make suggestions based on preprogrammed guidelines and protocols. CPOE is known to reduce serious medical errors and prevent otherwise undetected adverse drug events (ADEs) (50). When CPOE systems are properly designed and implemented, they can improve workflow efficiency by supplying real-time dosing information and other decision support protocols and guidelines. Poorly designed or improperly implemented CPOE systems, however, have the potential to decrease efficiency and increase medication error.
Medication safety is a high priority for quality improvement initiatives. Avoiding abbreviations that may lead to medication error increases patient safety (51). Table 3.2 lists examples of dangerous abbreviations and dose expressions that should be avoided. Avoiding abbreviations that can be misread is an important and effective improvement, especially when orders are handwritten. One easily remembered and important rule about the written medication order is “always lead and never follow” a decimal point when using zeros. An order that is written as .1 mg should be written as 0.1 mg—an example of leading with a zero. It can be very dangerous for the written period to be missed, resulting in 1 mg being given to a patient rather than 0.1 mg. The leading zero should alert to the correct dosage. An order that is written as 1.0 mg should be written as 1 mg—never following with a zero, so that a patient is not mistakenly given 10 mg of a drug if the period is missing or not seen. Exclusive use of properly designed and implemented CPOE systems can eliminate misread written orders.
Bar coding of medications improves error occurrence by reducing the rate of wrong medication by nearly 75%. Other types of medication error improvements attributed to bar coding include incorrect dose, wrong patient errors, and wrong time errors, which were reduced substantially through the use of bar coding (52).
The Leapfrog Group, comprised of Fortune 500 companies and other large health care purchasers, has made CPOE one of its top priorities for improving patient safety along with appropriate staffing of intensive care units (ICUs) and appropriate referral of high-risk patients to “centers of excellence.” CPOE and bar coding are two safety technologies that are proven to lower the risk of medical errors.
Disruptive Provider Behavior
In 2009, as part of its accreditation standards, the Joint Commission proposed that all health care organizations with professional staffs develop and implement a Code of Conduct Policy along with an education program that addresses disruptive behavior.
Disruptive physician (provider) behaviors include inappropriate conduct in the hospital setting, resulting in conflict or confrontation. These behaviors can range from verbal and even physical abuse to sexual harassment. In recent years disruptive behavior in the hospital setting has become more evident, if not more common. One study showed that the vast majority of surveyed physicians, nurses, and administrators had witnessed disruptive behavior by physicians (53). Nurses and other hospital employees also commit disruptive behavior, but it is far less common than disruptive physician behavior. Disruptive behavior in the hospital setting can have adverse effects on patient safety and overall quality of care.
One recommendation for mitigating disruptive behavior among health care professionals when concise and clear communication is needed is the SBAR method, mentioned above. Having an accepted and agreed-upon verbal process to question or suggest changes in patient management improves communication. Team building that encourages collegial interaction and a sense that all members of the health care team are important and have something to offer can promote a culture that makes disruptive behavior less likely.
Patient and Family Involvement in Quality and Safety
One of the better definitions of quality is “meeting a customer’s (patient’s and their families) expectations.” Clear and frequent communication between the team of health care professionals and the patient and the patient’s family is the most effective way to determine and meet appropriate expectations. The Joint Commission, in collaboration with the Centers for Medicare and Medicaid Services, introduced an initiative they called “Speak Up.” The program features brochures, posters, and buttons on a variety of patient safety topics. The program goal is designed to urge patients to take an active role in preventing health care errors by becoming involved and informed participants as members of the health care team. In 2008 a survey conducted by the Joint Commission indicated that campaigns like Speak Up add significant value to the accreditation process (54). Eighty percent of the more than1,900 organizations that responded rated the program as good or excellent.
Another initiative developed at Rand and the University of California–Los Angeles is the PREPARED checklist for informed, collaborative choice (Table 3.3) . Studies show that greater patient (and family) involvement in health care decision making results in improved satisfaction and better outcomes (55). The PREPARED checklist, using each letter in the word and a mnemonic, consists of a structured conversation that includes the Plan, Reason for the plan, Expectation of benefit, Preferences (e.g., prefer or avoid surgery), Alternatives, Risks, and Expenses, followed by an informed collaborative Decision to accept or reject the plan.
Table 3.3 PREPARED Checklist Process for Informed Communication
| P lan: | Course of action being considered |
| R eason: | Indication or rationale |
| E xpectation: | Chances of benefit and failure |
| P references: | Patient-centered priorities |
| A lternatives: | Other reasonable options/plans |
| R isks: | Potential harms from considered plans |
| E xpenses: | Direct and indirect costs |
| D ecision: | Fully informed collaborative choice |
The use of either or both of these programs should improve overall safety by informing the patient and his or her family about what will happen, what is expected along with the known risks (complications and side effects), so that they can alert the health care team of any expected or unexpected adverse events. Patients and their families traditionally have low self-efficacy or confidence that they can understand and actively participate during their health care. Programs such as Speak Up and PREPARED are shown to increase patient and family member self-efficacy.
Disclosure and Apology for Adverse Events
Organized medicine is increasing its focus on the prevention of medical error. A controversial issue involving medical error is the need to promptly disclose and apologize for any medical errors that occur. In the past many, if not most, health care organizations focused on managing the medical legal risk of medical error. The conventional wisdom was that any disclosure and apology for error would lead to litigation and bigger payouts. The Joint Commission and other professional organizations require or endorse active disclosure to the patient when adverse events occur, including those caused by error (56).
Three programs are worth noting in any discussion of disclosure and apology for medical error. First is the University of Michigan’s patient safety program, which addresses the need to disclose medical error in several publications (57). Important points are made about a patient’s rights concerning disclosure of medical error and that an apology for errors can be a productive benevolent gesture rather than an admission of fault. The authors point out several fallacies about disclosure, including that disclosing medical error always leads to litigation and that error always means negligence.
Lucian Leape, one of the fathers of the modern patient safety movement, pointed out that a patient has an ethical right to full disclosure of medical error (58). Although an apology is not an ethical right, it is a therapeutic necessity, according to Leape. Several programs are under way to test the assertion that disclosure and apology can decrease the likelihood of litigation. COPIC, a Colorado medical insurance company, found that full disclosure results in small early settlements and dramatically reduced law suits and payouts (59).
The Sorry Works Coalition, which is a coalition of doctors, insurers, and patient advocates, urges the use of full disclosure and apology for medical errors (60). They point out that the current tort system has failed, resulting in higher and higher malpractice premiums without decreasing the rate of medical error. Demands for caps on malpractice awards and greater disciplinary measures for providers are largely ineffective. The Sorry Works Coalition advocates early disclosure with apology and financial settlements without litigation as the way forward in dealing with medical error.
Safety in the Office Setting
Thus far, most efforts to improve safety involved activities that occur in the inpatient setting. This is a logical initial approach because most risky procedures and tests are performed in the hospital setting. There is a trend to adapt some invasive procedures and tests and offer them in the office setting. Gynecologic procedures such as hysteroscopy and loop excision of the cervix are examples of this. It is anticipated that there will be increasing numbers of “risky” invasive procedures performed in the office setting. The American College of Obstetricians and Gynecologists (ACOG) established a Task Force on Patient Safety in the Office Setting. In addition to the task force and its report, the college developed a patient safety assessment tool and a certification process (61).
The charge to the task force was to “assist, inform and enable Fellows of the College to design and implement processes that will facilitate a safe and effective environment for the more invasive technologies currently being introduced into the office setting.” The task force produced a monograph and a publication containing an executive summary of the work and recommendations (62). The task force addressed issues of leadership in the office setting; competency and assessment; teamwork and communication; anesthesia safety; measurement (of processes and outcomes); and tools such as checklists, time-outs, and drills.
In the hospital setting, leadership for safety is provided at multiple levels, starting with the department chair, with assistance from designated personnel in risk management and quality assurance. In the office setting, this responsibility must be assumed by one individual in a solo practice and one or several in a group practice. One individual should be designated as medical director and his or her responsibilities are outlined in Table 3.4.
Table 3.4 Medical Director Responsibilities in an Office Setting
• Motivation of staff to create a “safety culture” < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|