At term, 2000 rad is the threshold & fetal risks same as mat risks.
Risk of anomalies, growth restriction, or SAB not increased w/ radiation exposure of <5 rad. True threshold dose is likely >20 rad.
Risk of CNS effects (eg, microcephaly, mental retardation) highest at 8–15 w. There is no established risk at <8 w or >25 w.
The threshold dose of ionizing radiation → mental retardation at <16 w is 35–50 rad. After 16 w, the threshold is 150 rad.
1–2 rad fetal exposure may ↑ leukemia risk by 1.5–2×, but baseline childhood cancer risk is 0.2–0.3%; therefore, overall risk is still low.
No single diagnostic procedure provides radiation dose signif enough for adverse embryonic/fetal effect, esp mid to late Preg.
• Nuclear medicine: Radioactive iodine contraindicated in Preg. Tc-99m usually results in fetal exposure of <0.5 rad.
• Contrast agents: Iodine-based contrast safe for use in Preg. Gadolinium relative contraindicated in Preg – assess risks/benefits of contrast & obtain consent. Gadolinium crosses placenta → excreted into amniotic fluid. Unk exposure duration & effect on fetus.
ULTRASOUND IN EARLY PREGNANCY
Ultrasound in Pregnancy (Obstet Gynecol 2009;113:451)
• 1st trimester US: TVUS best in early Preg to confirm IUP, evaluate ectopic Preg, determine GA, evaluate twin Preg chorionicity, confirm cardiac activity, evaluate adnexal masses. Also obtain nuchal translucency, nasal bone for prenatal screening.
GS: Visible by ∼4 w GA, eccentrically implanted in the midupper fundus w/ a bright decidual rxn (double-ring sign), visible in 2 planes. Not used to determine final GA. Mean sac diameter (the avg of 3 measurements in mm) + 30 = GA (days) ± 3 d.
Yolk sac: Visible at 5 w GA, should be seen when the mean GS diameter is >13 mm.
Embryo: Visible at 6 w GA, or when mean GS diameter is ≥20 mm.
1st trimester CRL is most accurate dating. If ≤9.5 w GA, CRL in mm + 42 = GA (days) ± 3 d.
FHM: Observed when the embryo is ≥5 mm CRL. FHR = 100 bpm at 5–6 w GA, & → peak 175 bpm at 9 w GA. If FHM is seen, SAB rate is 2–3% in asymptomatic low-risk women. Women <35 yo who p/w VB = 5% SAB rate if the US is nml & shows FHM.
To quickly estimate EDD from LMP, use Naegele’s rule: Add 1 y, subtract 3 mo, & add 7 d (= 280 d from LMP).
• 2nd & 3rd trimester US – see Chap. 9.
• US for determination of GA: US dating takes preference over menstrual dating when the discrep is >7 d in the 1st trimester; >10 d in the 2nd trimester. In the 3rd trimester, accuracy of a US is w/i 3–4 w.
ACUTE PELVIC PAIN
Definitions and Epidemiology (Natl Health Stat Report 2010;6:1)
• Lower abdominal or pelvic pain present for <7 d. Most common presenting complaint & primary dx for women of ages 15–64 who are seen in the ER.
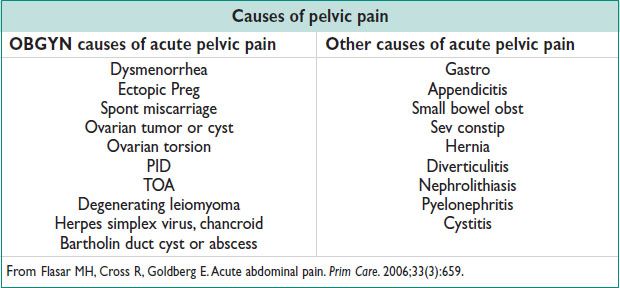
Pathophysiology and Clinical Manifestations (Prim Care 2006;33:659)
• Visceral pain: Stretch, distention, torsion, or contraction of abdominal organs is detected by autonomic, afferent nociceptors → “slow,” C-fibers relay the signal to the CNS → pain is usually midline or bilateral, poorly localized, dull, achy, or cramping.
• Parietal pain: Direct irritation of the peritoneal lining is detected by somatic, afferent nociceptors → “fast,” A-delta fibers relay the signal → pain is unilateral, localized, sharp.
• Referred pain: Visceral nerve afferents carrying stimuli from a diseased organ enter the spinal cord at the same level as somatic afferents from a remote anatomic location. Eg, free fluid in the abd can irritate the diaphragm causing referred pain in the shoulder.
Physical Exam
• Fever, tachy, HoTN → expedite w/u, concern for sepsis/infxn, intra-abdominal bleeding (eg, ruptured ectopic Preg, hemorrhagic ovarian cyst), ovarian torsion, appendicitis.
• Abdominal exam: Note prior surgical scars, distention, hyperactive or high-pitched bowel sounds, rebound, guarding, rigidity. Palpate 4 quadrants.
• Pelvic exam: Note swelling, erythema, lesions, bleeding, discharge, masses, nodularity, cervical motion tenderness, or pain.
Diagnostic Workup and Studies
• Labs: Urine or serum beta hCG (on every reproductive age woman in the ER), CBC, urinalysis & culture, vaginal wet prep, gonorrhea & chlamydia PCR
• Imaging: Transabdominal US or TVUS
• Culdocentesis: Rarely used. Aspiration of fluid from the post cul de sac. Considered in limited resource settings.
• Diagnostic laparoscopy: Consider for the unstable pt w/ abdominal pain.
• Rx & medications depend on dx (see other sections, below).
ECTOPIC PREGNANCY
Definitions & Epidemiology (Obstet Gynecol 2008;111:1479; NEJM 2009;361:379)
• Preg outside of the endometrial cavity. 2% of 1st trimester pregnancies.
• 6% of all pregnancy-related deaths (leading cause of death in the 1st trimester).
• Ectopic Preg increasing (4.5/1000 pregnancies in 1970 → 19.7/1000 in 1992).
• Rate of rupture w/ ectopic Preg is 20–35%.
Etiology
• Blastocyst implants & invades improperly at nonendometrial site. 97% in fallopian tubes, most frequently in the ampullary region. Other implantation sites include the isthmic portion of the tube, fimbria, uterine cornua, cervix, ovary, prior C/S scar, or abd.
• Heterotopic Preg → 2 or more implantation sites (ie, an IUP & ectopic Preg). Rare, only 1:8000–1:30000 nml pregnancies. Increased to 1.5/1000 after assisted reproductive technologies.
• Risk factors: Prior ectopic Preg, prior tubal Surg, tobacco smoking, prior PID, Chlamydia trachomatis infxn, 3 or more prior spont miscarriages, age >40 y, prior medical or surgical abortion, infertility >1 y, lifelong sexual partners >5, current IUD use, IVF/ART.
Clinical Manifestations and Physical Exam
• Lower abdominal pain on the affected side. Vaginal bleeding.
• Clinical findings are often unremarkable w/ unruptured ectopic Preg. Only 75% develop marked abdominal tenderness. May p/w shoulder pain, dizziness, syncope. Hx & risk factors are useful to assess risk/suspicion.
• VS & clinical assessment to look for signs of hemodynamic stability.
• Pelvic exam: Adnexal mass (20%). Abdominal exam: Tenderness to palpation. Evaluate for surgical abd: Rebound, guarding, rigidity.
Diagnostic Workup and Studies
• Labs: CBC (sometimes serial Hgb), bld type (RhoGAM if Rh-negative), CMP for BUN/Cr, & AST/ALT (if considering MTX).
• Serum (quantitative) hCG:
If hCG above “discriminatory zone” of 1500–2000 mIU/mL, nml IUP seen on TVUS.
If hCG >1500–2000 mIU/mL & no IUP on TVUS → likely abn Preg (eg, ectopic Preg, incomplete AB, resolving completed AB)
If hCG <1500 mIU/mL & no IUP → rpt hCG in 48 h (at SAME lab).
In 85% of women w/ a nml IUP, the hCG will ↑ ≥63% in 48 h.
In 99% of women w/ a nml IUP, the hCG will ↑ ≥53% in 48 h.
An ↑ in serum hCG of <∼60% in 48 h → abn Preg
• TVUS: 91% accuracy of TVUS for dx of ectopic Preg. Extrauterine GS or embryo seen in only 15–30% of cases. Most common US finding is a solid mass btw the ovary & uterus.
Adnexal mass (other than a simple ovarian cyst) is 84% sensitive & 99% specific for ectopic Preg.
Trilaminar endometrial stripe (only) is 38% sensitive & 94% specific for an ectopic Preg.
Pseudosac (intrauterine midline fluid collection) is neither sensitive nor specific for the dx of ectopic Preg. Do not confuse pseudosac for IUP.
• Serum progesterone: Often not definitive. Levels from 5–20 ng/mL are equivocal.
Serum progesterone <5 ng/mL sugg abn Preg (100% specific, 60% sensitive).
Serum progesterone >20 ng/mL sugg nml IUP (40% specific, 95% sensitive)
• Endometrial curettage: For “Preg of unk location,” D&C can evaluate POCs (float the villi), & assist in decision for diagnostic laparoscopy vs. dx of abn Preg (eg, missed AB).
Treatment and Medications
• Expectant mgmt: 68% → successful resolution (Lancet 1998;351:1115)
If initial hCG is <200 mIU/mL, 88% resolve w/o rx
Recheck hCG 48 h after initial lab tests to ensure declining serum hCG
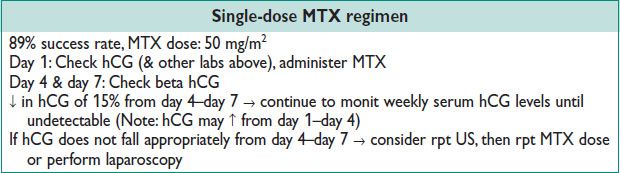
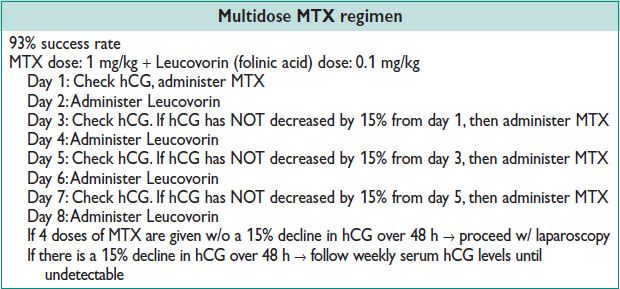
• Medical mgmt: MTX inhibits dihydrofolate reductase → decreased tetrahydrofolate → ↓ purine nucleotide synthesis → ↓ DNA/RNA in S-phase of cell cycle→ prevent proliferation (in active tissues like trophoblast, bone marrow, buccal/intestinal mucosa). 2 protocols (see below). Multidose regimen more effective for advanced GA & +ve fetal cardiac activity.
Side effects: Usually self-limited. Most common are nausea, vomiting, stomatitis, conjunctivitis, worsening abdominal pain 2–3 d after MTX dose due to expansion of the affected gestational tissue, transient liver dysfxn, & uncommonly myelosuppression, alopecia, pulmonary damage, anaphylaxis.
Pt instructions: Stop taking prenatal vitamins & folate supplements, avoid sun exposure, refrain from EtOH consump, intercourse, & vigorous physical activity.
Strong contraindications to MTX: Tubal rupture or hemodynamic instability, breast-feeding, alcoholism, alcoholic liver dz, or chronic liver dz, immunodeficiency, pre-existing bld dyscrasias (bone marrow hypoplasia, leukopenia, thrombocytopenia, signif anemia), active pulmonary dz, peptic ulcer dz, hepatic, renal, or hematologic dysfxn, Cr >1.3 mg/dL, AST or ALT >50 IU/L.
Relative contraindications to MTX:
GS >3.5 cm. Single-dose MTX 93% effective when the GS is <3.5 cm. Decreases to 87–90% efficacy when >3.5 cm. Large GS → ↓ success.
Embryonic cardiac activity. Single-dose MTX is 87% effective if +ve fetal heart motion.
Serum hCG level >5000 mIU/mL. Failure w/ single-dose MTX is 14.3% if hCG >5000 mIU/mL (compared to 3.7% failure if hCG <5000 mIU/mL). Consider multidose therapy or surgical mgmt.
• Surgical mgmt: Laparoscopy preferred if the pt is hemodynamically stable → shorter operative times, less bld loss, less analgesic requirements, shorter hospital stay, no difference in tubal patency rates, similar rates of subseq IUP.
Salpingostomy: Gold std Surg for ectopic. Open affected tube & evacuate ectopic POCs. Esp useful for pt w/ abn contralateral tube who desires future fertility. Persistent ectopic Preg in 4–15% of cases. Follow weekly serum hCG levels until they are undetectable. Check pathology to confirm POCs.
Salpingectomy: Removal of entire affected fallopian tube. Appropriate for pts w/ a nml appearing contralateral tube who desire future fertility, or pts who do not desire future fertility. Eliminates risk of persistent ectopic Preg, or recurrent, ipsilateral ectopic Preg. If confident that all trophoblast removed, no need for serial hCGs.
OVARIAN CYSTS
Definitions (Obstet Gynecol 2011;117:1413; Am Fam Physician 2009;80:815)
• Functional ovarian cysts: Follicular cysts form when an unruptured ovarian follicle fills w/ serous fluid → capsule distention/pain. Corpus luteum cysts, normally present in early Preg; can bleed → distention or active hemorrhage.
• Benign & neoplastic ovarian cysts (see also Chap. 21): Dermoid, stromal & germ cell tumors, fibroma, epithelial neoplasm, cystadenoma, endometrioma.
Epidemiology and Etiology
• Incid of ovarian cysts = 5–15%. Lifetime risk 5–10% for adnexal mass Surg
• Diff dx: Leiomyomata, TOA, hydrosalpinx, ectopic Preg, paratubal cysts, diverticular abscess, appendiceal abscess, nerve sheath tumors, ureteral diverticulum, pelvic kidney, bladder diverticulum, peritoneal inclusion cysts, malig.
Clinical Manifestations
• Most are asymptomatic, but may p/w pain, pressure sensation, dyspareunia
• Intermittent pain may indicate ovarian torsion. Acute, sev pain may represent ovarian torsion or cyst rupture. Increased abdominal girth, bloating, wt loss, & early satiety raise concern for malig. Hormonal disruption w/ estrogen/androgen secretion.
Physical Exam and Diagnostic Workup
• Pelvic exam: 45% sens & 90% spec. ↓ detection w/ BMI >30
• Labs: hCG, CBC, coags/other labs depending on presentation & Hx
• Abdominal & pelvic US: TVUS sens 82–91% & spec 68–81% for distinguishing benign from malignant dz. Classic US appearance of a simple cyst is anechoic, well circumscribed, echolucent w/ post acoustic enhancement.
• See Chap. 21 for w/u for malig, tumor markers, & referral to gyn oncology
Treatment and Medications
• Observation: Most simple ovarian cysts spontaneously regress in 6 mo. ↑ adnexal/ovarian torsion at 6–10 cm mass. 0–1% risk of malig if cyst is unilocular, thin walled, sonolucent, <10 cm in diameter, & has smooth, regular borders.
Premenopausal women w/ cyst <3 cm do not require f/u
Premenopausal women w/ cyst 4–10 cm who desire expectant mgmt → rpt US for resolution in 12 w (4–12 w depending on concern)
Postmenopausal women w/ cysts 4–10 cm & CA-125 <35 U/mL who desire expectant mgmt → serial USs every 4–6 w
• Surg: Provides definitive pathologic dx. Indicated for hemodynamic instability, cyst >6–10 cm, concern for malig, concern for torsion, or persistent sx
Laparoscopy: ↓ operative morbidity, postoperative pain, analgesics, recovery time, & costs
Laparotomy: Usually for malig (w/ appropriate staging), hemodynamic instability, or failed laparoscopy
Cystectomy vs. oophorectomy: Consider the pt’s age, reproductive desires, menopausal status, & preoperative dx. (If a corpus luteum cyst is removed during Preg at <12 WGA → progesterone supplementation.)
ADNEXAL TORSION
Definition and Epidemiology (Am J Obstet Gynecol 1985;152:456)
• Twisting of adnexal components (most commonly ovary ± fallopian tube) on their ligamentous supports → venous, arterial, & lymphatic obst
• 5th most common gyn emergency; 2.7% of female surgical emergencies
• Females of all ages (fetal/neonat to elderly); however, 70% are of ages 20–39
• Increased risk w/ Preg (20–25% of all cases) & ovarian hyperstimulation
Etiology (Clin Exp Obstet Gynecol 2004;31:34; Am J Obstet Gynecol 1991;164:577)
• 94% a/w adnexal mass (48% cysts, 46% neoplasms). ↑ w/ masses 6–10 cm
• Congenitally long ovarian ligaments
• ↑ w/ strenuous exercise, intercourse or sudden ↑ in abdominal pressure
• Right ovarian torsion more common than left (protection from sigmoid colon)
Pathophysiology
• Compromise of vascular pedicles impedes arterial inflow & lymphatic & venous outflow → Venous drainage interrupted before arterial due to less compressibility of arterial walls → Marked ovarian enlargement can develop w/ continued perfusion & blocked outflow
Clinical Manifestations and Physical Exam (Ann Emerg Med 2001;38:1506)
• Acute pelvic pain (83%): Sudden/sharp pain (59%) radiating to back/flank/groin (51%) w/ peritoneal signs (3%)
• Nausea &/or vomiting (70%): Colicky or sporadic sx from intermittent torsion
• Neonates: Usually in 1st 3 mo of life w/ feeding intolerance, vomiting, abdominal distension, & fussiness/irritability – usually ovarian cysts have already been identified w/ prenatal US (Arch Pediatr Adolesc Med 1998;152:1245).
• Resolution of sx seen after ∼24 h due to ischemic death of involved structures. Functionality can be preserved w/ immediate intervention.
• Bimanual exam: Adnexal mass (72%), tenderness in RLQ or LLQ
• Fever (<2%): May be a marker of necrosis, particularly in the setting of increased WBC
Diagnostic Workup/Studies
• Dx confirmed at Surg. ∼40% correct preop dx (J Reprod Med 2000;45:831)
• Clinical dx: (1) Lower abdominal pain, (2) ovarian cyst/mass, & (3) diminished or absent bld flow in the ovarian vessels on color Doppler flow imaging. Rule out ectopic Preg, PID, appendicitis, diverticulitis, nephrolithiasis, & leiomyoma-related sx.
• Lab studies: hCG to rule out Preg; labs: CBC, BMP, may see anemia, leukocytosis, or electrolyte abnormalities from vomiting.
• US: Cystic or solid mass (70%), free fluid in post cul-de-sac (>50%), enlarged heterogenous appearing ovary (J Ultrasound Med 2001;20:1083). Nml ovary on US does not rule out torsion.
Doppler: Controversial; some studies w/ sens & spec of 100% & 97%, others w/ 43% & 92% (Eur J Obstet Gynecol Reprod Biol 2002;104:64); color Doppler flow ↑ dx of torsion when absent but not reliable when flow is present.
Whirlpool sign: Doppler finding in vascular pedicle (J Ultrasound Med 2009;28:657)
MRI/CT: Limited value, can ID ovarian edema; diagnostic criteria not been well defined or validated. CT potentially useful in excluding other diagnoses on diff.
Treatment (NEJM 1989;321:546; Obstet Gynecol Surv 1999;54:601)
• Swift operative eval: Preserve ovarian fxn & prevent infxn from necrosis
• Laparoscopic detorsion w/ cystectomy vs. salpingo-oophorectomy: Consider detorsion in premenopausal pts, majority regain prev form & fxn, even if ischemic appearing intraoperatively. No ↑ risk of clot dislodgement/PE in either detorsion or salpingo-oophorectomy. Consider oophoropexy for prevention esp w/ recurrent ovarian torsion.
PELVIC INFLAMMATORY DISEASE (PID)
Definition and Epidemiology (Obstet Gynecol 2010;116:419)
• PID: Clinical spectrum of inflamm disorders of the female upper genital tract including endometritis, salpingitis, TOA, & pelvic peritonitis
• >800000 cases/y in US; true magnitude unk due to difficult dx
• Risk factors: Age <25, young age at 1st intercourse, nonbarrier contraception, multi sexual partners, oral contraception, cervical ectopy, IUD insertion w/i prev 3 w
Etiology and Microbiology (NEJM 1975;293:166; Ann Intern Med 1981;95:685)
• Neisseria gonorrhoeae: 1/3 of cases; 15% w/ endocervical gonorrhea develop PID
• C. trachomatis: 1/3 of cases; 15% w/ endocervical chlamydia develop PID
• Other pathogens: Vaginal flora (eg, anaerobes, Gardnerella vaginalis, Haemophilus influenzae, enteric gram-negative rods, & Streptococcus agalactiae)
Clinical Manifestations
• Lower abdominal pain (90%). Mucopurulent discharge (75%).
• Long-term sequelae: Infertility (18%), ectopic Preg, chronic pelvic pain, dyspareunia
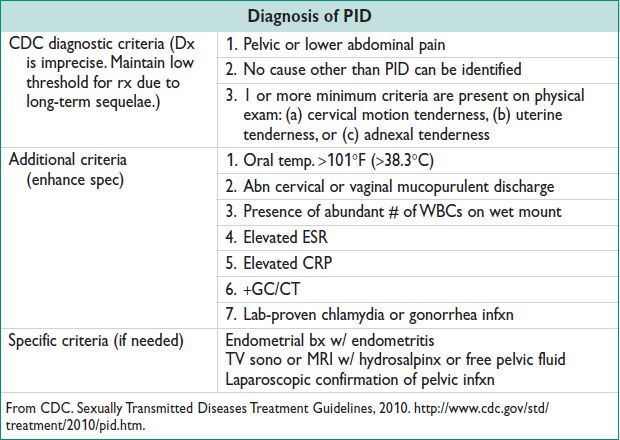
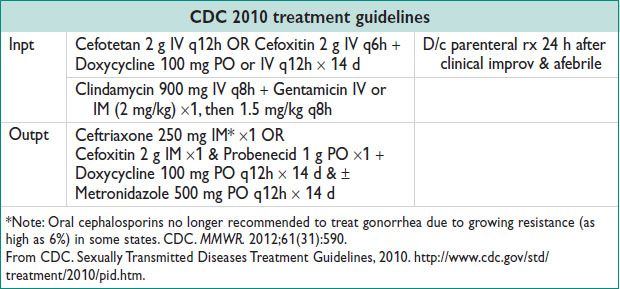
Treatment
• Indications for hospitalization: Preg, outpt therapy failure after 72 h, noncompliance, sev illness (eg, N/V, high fever), or TOA
• IUD: Do not need to remove IUD, close clinical f/u if remains in place
• Screen for additional STIs. F/u in clinic in 3 d
• EPT is indicated to prevent reinfection: See state-specific legislation: http://www.cdc.gov/std/ept/legal/default.htm
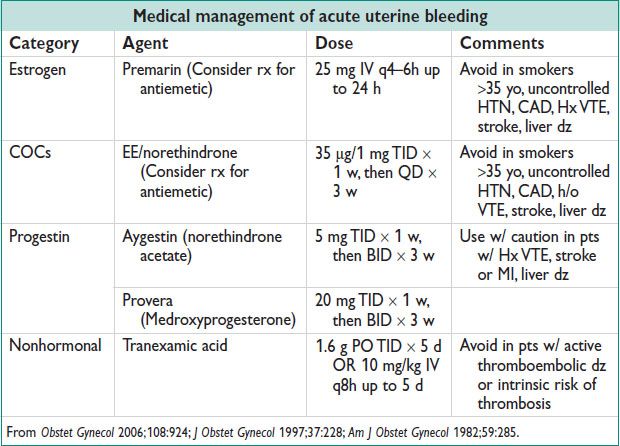
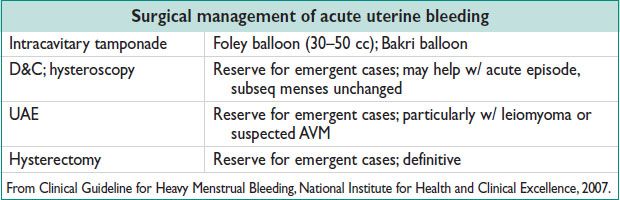
ACUTE UTERINE BLEEDING
Definition and Epidemiology (Fertil Steril 2011;95:2204; Obstet Gynecol 2002;99:1100)
• Heavy vaginal bleeding suff to require immediate intervention. May or may not occur in the setting of Chronic Abnormal Uterine Bleeding. See Chap. 5, Abnormal Uterine Bleeding.
• Affects 10–30% of women. 12% of gyn visits in ER. See SABs below, also.
Physical Exam
• Rapidly determine acuity: General appearance & stability. Orthostatic VS.
• Speculum exam: Rule out nonuterine causes (eg, rectal bleeding, genitourinary, vaginal lacerations, cervical lesions), assess extent of bleeding (eg, active/ongoing hemorrhage)
• Bimanual exam: Evaluate for structural abnormalities, such as a prolapsing fibroid
Diagnostic Workup/Studies
• Always rule out Preg – qualitative hCG. Labs: CBC, coags including fibrinogen, type & screen. Imaging: Consider TVUS.
Treatment and Medications
• If unstable: 2 large bore IVs, crystalloid fluid resusc
• Consider xfusion of 2 U packed RBCs if Hgb <7.5
• If anemic, start PO ferrous sulfate at discharge from hospital
• Initiate goal-directed therapy
SPONTANEOUS ABORTION (SAB)
Definition and Epidemiology (Fertil Steril 2003;79:577; Obstet Gynecol 2005;105:333)
• SAB (miscarriage) occurs before 20 w0d & <500 g
• Early Preg failure complicates 12–15% of known pregnancies & 17–22% of all pregnancies; 80% occur in the 1st 12 w of gest; fertilization → 30% implantation failure → 30% early loss (= 60% loss before recognized clinical Preg) → 12–15% clinical Preg SAB → 25% live birth.
• Vaginal bleeding in ∼25% known 1st trimester pregnancies → ∼50% of those are SABs
• Once fetal cardiac activity is noted, 90–96% have ongoing Preg
• Risk factors: ↑ mat age, prev SAB, heavy smoking, EtOH, cocaine, NSAIDs, fevers, caffeine >200 mg daily may be a/w SAB, chronic mat dz (DM, autoimmune, APLA syn), short interpregnancy interval, uterine anomalies.
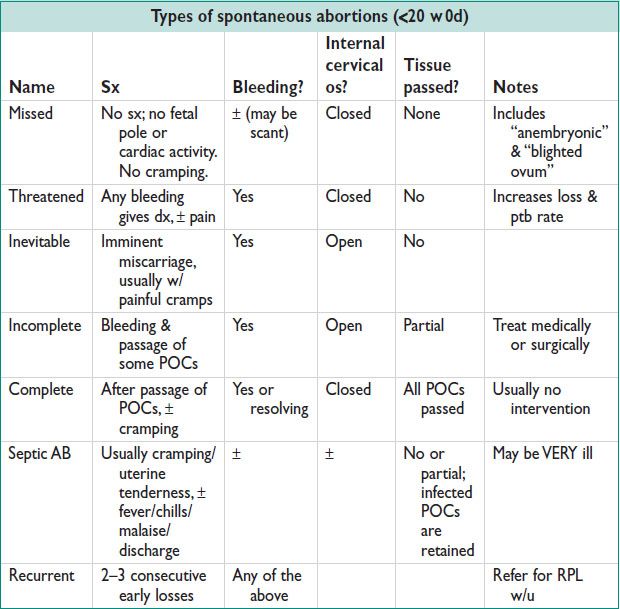
Etiologies
• Chromosomal abnormalities (50%); congen anomalies; trauma (early GA uterus generally protected from blunt trauma); host factors (eg, uterine abnormalities [septum]), mat infxn, mat endocrinopathies or corpus luteum dysfxn, mat inherited or Acq thrombophilia; unexplained.
• Diff: Cervical bleeding (polyp, malig, trauma), ectopic Preg, infxn, molar Preg, SAB (see above), subchorionic hemorrhage, vaginal trauma.
Clinical Manifestations and Physical Exam
• Amenorrhea, vaginal bleeding, &/or pelvic pain/cramping
• Cessation of nml sx of Preg (eg, nausea, breast tenderness)
• Speculum/digital exam to assess cervical dilation, POCs
• Evaluate extent of bleeding (eg, hemorrhage) & mat stability
Diagnostic Workup (Obstet Gynecol 1992;80:670; Ultrasound Obstet Gynecol 1994;3:63)
• Passed tissue: “Float villi” in saline to evaluate frond-like chorionic villi; send to pathology
• Transvaginal US: Distinguishes IUP vs. extrauterine Preg, viable vs. nonviable, presence of gestational trophoblastic dz, retained POCs, ectopic
Missed AB: No fetal cardiac activity + CRL >5 mm OR absence of embryonic cardiac activity w/ menstrual age >6.5 w
Findings suggestive of early Preg failure: Absence of yolk sac w/ MSD >13 mm; absence of embryonic pole w/ MSD >20 mm; enlarged yolk sac (>6 mm), irreg or low lying sac; slow FHT (<100 bpm at 5–7 w); small GS (difference btw MSD & CRL <5 mm); subchorionic hematoma >25% vol of the GS.
• Quantitative beta hCG: Low yield once IUP confirmed. If no IUP, serial hCGs q48h to rule out ectopic → ↓ hCG = nonviable IUP or spontaneously resolving ectopic.
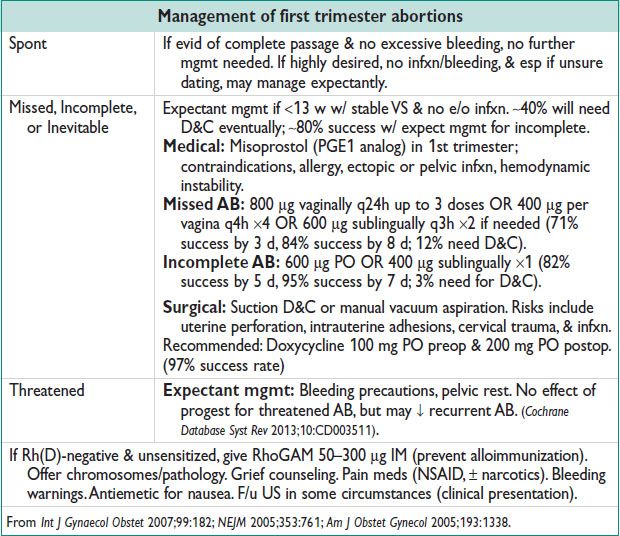
Management of First Trimester Abortions
TRAUMA IN PREGNANCY
Epidemiology (Int J Gynaecol Obstet 1999;64:87; Obstet Gynecol 2009;114:147)
• Leading cause of nonobstetric mat death during Preg. Complicates 3–8% of pregnancies; 2/3 from motor vehicle collisions.
• Up to 20% of pregnant women are victims of DV. Preg alone is an independent risk factor for DV (Am J Obstet Gynecol 1991;164:1491).
• Outcomes directly related to GA & severity/mech of injury
• 40–50% fetal loss rate w/ life-threatening mat trauma (eg, mat shock, head injury leading to coma, emergency laparotomy for mat indications) (Obstet Gynecol Clin North Am 1991;18:371).
• 1–5% fetal loss w/ nonlife-threatening injuries, but b/c more common, >50% of fetal losses occur w/ minor trauma
• Blunt trauma: Placental abruption (40% sev cases, 3% nonsevere cases), direct fetal injury (<1%), uterine rupture (<1%), mat shock, mat death
• Penetrating trauma: Gunshot wounds or stab wounds; fetal prog generally worse than mat prog
• Pelvic fractures: Fetal mortality rate 35%; may result in signif retroperitoneal bleeding. Not an absolute contraindication for vaginal delivery.
Clinical Manifestations & Physical Exam (Obstet Gynecol 2009;114:147)
• Placental abruption: Vaginal bleeding, uterine tenderness, abdominal pain, back pain, fetal distress, high-frequency uterine contractions, uterine hypertonus, decreased fetal movement, or even fetal death.
• Primary survey: Note that pregnant women can lose a signif amt of bld before tachy & HoTN occur due to their increased intravascular vol.
• Abd: Ecchymoses (new & old), seat belt injury, penetrating abdominal injuries, palpate for contractions or tenderness
• Speculum: Bleeding, rupture of membranes, vaginal lacerations, pelvic bone fragments
Diagnostic Workup/Studies (Obstet Gynecol 2009;114:147)
• US: Fetal cardiac activity, fetal GA & presentation, free peritoneal fluid or mat hemorrhage. Consider FAST to assess for free fluid in perihepatic, perisplenic, pelvic, & pericardial areas.
• Radiologic eval: Should not be deferred if req for mat assessment
Initial Management (ACOG 1998)
• Mat: Supplemental O2; 2 large bore IVs; early IV fluid resusc in ratio 3:1 based on bld loss; left lateral uterine displacement after 20 w (if spinal injury suspected, manual displacement or a wedge under a backboard ok); labs – CBC, type & screen, coags, & hold tube. Kleihauer–Betke & RhoGAM for Rh-negative moms.
• Once mother stabilized, proceed w/ fetal assessment:
GA <24 w0d: Document FHR by Doppler or real time US; tocometer if high concern for abruption by Hx or physical exam
GA >24 w0d: 4–6 h continuous fetal monitoring (includes FHR & tocodynamometry). If >6 contractions in an hour or sev injury → prolonged monitoring for 24 h. Nonreactive NST → further eval (BPP or prolonged fetal monitoring).
• In setting of mat cardiopulmonary arrest, delivery by C/S if >4 min has elapsed. Improves mat resusc by decreasing uterine compression of venous return.
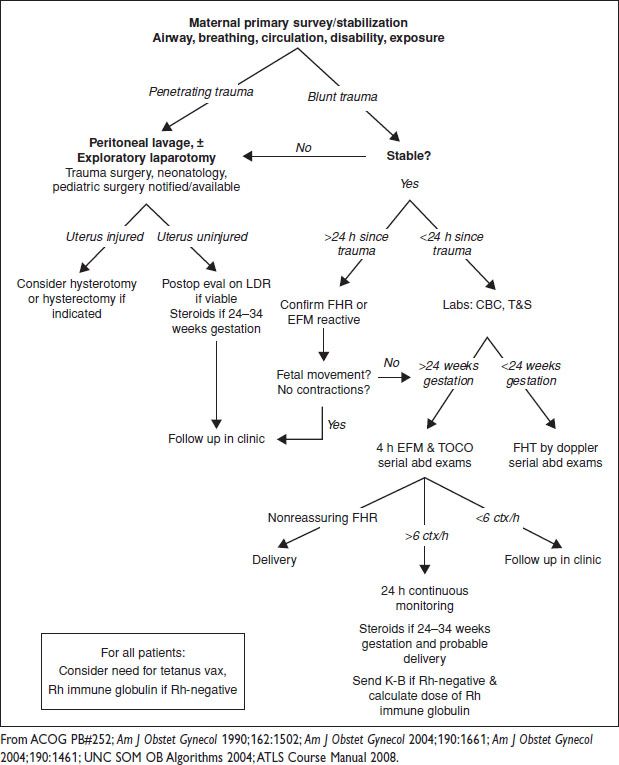
Figure 2.1 Management of trauma in pregnancy