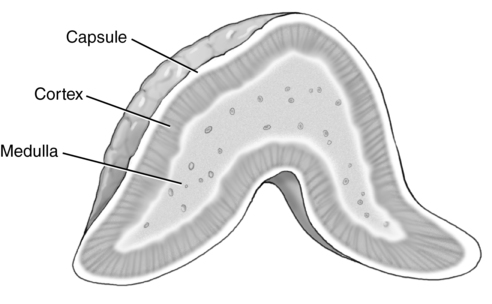
CHAPTER 12 congenital disorder causing an increase in production of androgens. uncommon condition resulting from excessive aldosterone secretions. excessive production of aldosterone. focal or generalized enlargement of the lymph nodes. malignant tumor of the adrenal gland found in young children. rare vascular tumor of the adrenal medulla. pertaining to organs closely attached to the posterior abdominal wall. • Retroperitoneal structures located in Gerota’s fascia within the perinephric space. • Located anterior, medial, and superior to each kidney. • Lie lateral to the diaphragmatic crura. • Right adrenal gland lies posterior and lateral to the inferior vena cava. • Left adrenal gland lies lateral to the aorta and posterior-medial to the splenic artery and tail of the pancreas. • The superior, middle, and inferior suprarenal arteries supply the adrenal glands. • Superior suprarenal artery arises from the inferior phrenic artery. • Middle suprarenal artery arises from the lateral aspect of the abdominal aorta. • Inferior suprarenal artery arises from the renal artery. • Right suprarenal vein drains directly into the inferior vena cava. • No preparation is necessary for a sonogram of the adrenal glands or retroperitoneum. • Nothing by mouth (NPO) 6 to 8 hours before examination for adults, 6 hours for children, and 4 hours for infants to decrease intestinal interference. • Use the highest-frequency abdominal transducer possible to obtain optimal resolution for penetration depth. • Place gain settings to display the normal liver parenchyma as a medium shade of gray with adjustments to reduce echoes within the vessels. • Focal zone(s) at or below the place of interest. • Sufficient imaging depth to visualize structures immediately posterior to the region of interest. • Harmonic imaging or decreasing system compression (dynamic range) can be used to reduce artifactual echoes within anechoic structures. • Spatial compounding can be used to improve visualization of structures posterior to a highly attenuating structure. • Supine, oblique, and/or decubitus positions may be used. • Sagittal or coronal and transverse planes are used to evaluate and document the adrenal glands using surrounding anatomical landmarks. • Documentation and measurement of the length, height, and width. • Color Doppler imaging, using a 60-degree angle or less, to evaluate each adrenal gland visualized. • Evaluation and documentation of the retroperitoneum using a four- or nine-quadrant method. • Length, height, and width of visible lymph nodes, including color Doppler imaging of the hilum. • Documentation and measurement of any abnormality in two scanning planes with and without color Doppler should be included. • Normal range: 10 to 80 pg/mL. • Regulates cortisol production. • Produced in the pituitary gland. • Elevation associated with adrenal tumor, Cushing disease, and lung tumor. Conditions Associated with the Adrenal Glands
Retroperitoneum
Location
Vascular anatomy
Technique
Preparation
Examination technique and image optimization
Laboratory values
Adrenocorticotrophic hormone (ACTH)
Sodium
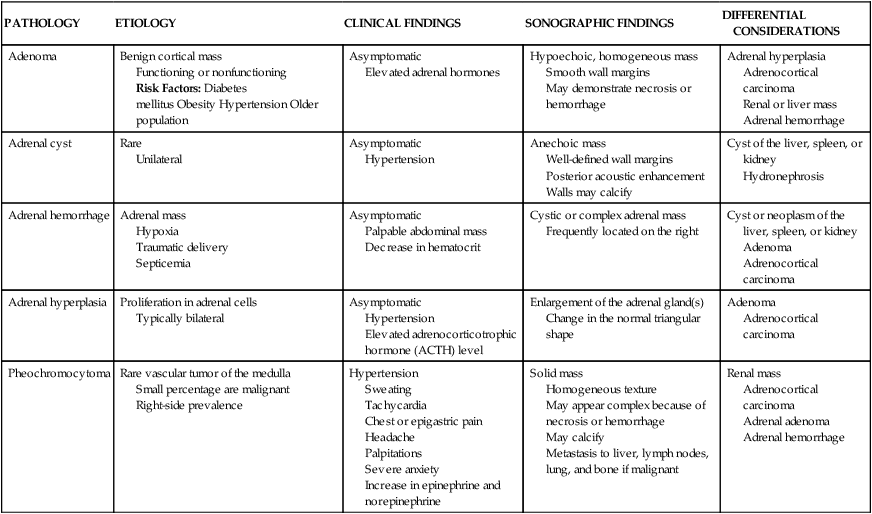
PATHOLOGY
ETIOLOGY
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Adenoma
Benign cortical mass
Functioning or nonfunctioning
Risk Factors: Diabetes mellitus Obesity Hypertension Older population
Asymptomatic
Elevated adrenal hormones
Hypoechoic, homogeneous mass
Smooth wall margins
May demonstrate necrosis or hemorrhage
Adrenal hyperplasia
Adrenocortical carcinoma
Renal or liver mass
Adrenal hemorrhage
Adrenal cyst
Rare
Unilateral
Asymptomatic
Hypertension
Anechoic mass
Well-defined wall margins
Posterior acoustic enhancement
Walls may calcify
Cyst of the liver, spleen, or kidney
Hydronephrosis
Adrenal hemorrhage
Adrenal mass
Hypoxia
Traumatic delivery
Septicemia
Asymptomatic
Palpable abdominal mass
Decrease in hematocrit
Cystic or complex adrenal mass
Frequently located on the right
Cyst or neoplasm of the liver, spleen, or kidney
Adenoma
Adrenocortical carcinoma
Adrenal hyperplasia
Proliferation in adrenal cells
Typically bilateral
Asymptomatic
Hypertension
Elevated adrenocorticotrophic hormone (ACTH) level
Enlargement of the adrenal gland(s)
Change in the normal triangular shape
Adenoma
Adrenocortical carcinoma
Pheochromocytoma
Rare vascular tumor of the medulla
Small percentage are malignant
Right-side prevalence
Hypertension
Sweating
Tachycardia
Chest or epigastric pain
Headache
Palpitations
Severe anxiety
Increase in epinephrine and norepinephrine
Solid mass
Homogeneous texture
May appear complex because of necrosis or hemorrhage
May calcify
Metastasis to liver, lymph nodes, lung, and bone if malignant
Renal mass
Adrenocortical carcinoma
Adrenal adenoma
Adrenal hemorrhage
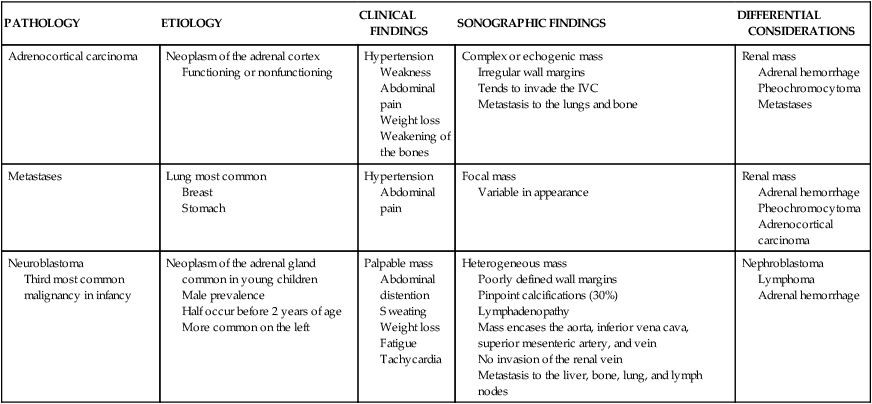
PATHOLOGY
ETIOLOGY
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Adrenocortical carcinoma
Neoplasm of the adrenal cortex
Functioning or nonfunctioning
Hypertension
Weakness
Abdominal pain
Weight loss
Weakening of the bones
Complex or echogenic mass
Irregular wall margins
Tends to invade the IVC
Metastasis to the lungs and bone
Renal mass
Adrenal hemorrhage
Pheochromocytoma
Metastases
Metastases
Lung most common
Breast
Stomach
Hypertension
Abdominal pain
Focal mass
Variable in appearance
Renal mass
Adrenal hemorrhage
Pheochromocytoma
Adrenocortical carcinoma
Neuroblastoma
Third most common malignancy in infancy
Neoplasm of the adrenal gland common in young children
Male prevalence
Half occur before 2 years of age
More common on the left
Palpable mass
Abdominal distention
Sweating
Weight loss
Fatigue
Tachycardia
Heterogeneous mass
Poorly defined wall margins
Pinpoint calcifications (30%)
Lymphadenopathy
Mass encases the aorta, inferior vena cava, superior mesenteric artery, and vein
No invasion of the renal vein
Metastasis to the liver, bone, lung, and lymph nodes
Nephroblastoma
Lymphoma
Adrenal hemorrhage
CONDITION
DESCRIPTION
ETIOLOGY
CLINICAL FINDINGS
Addison disease
Life-threatening condition caused by partial or complete failure of adrenocortical function (hypofunction)
Destruction of the adrenal cortex
Loss of cortisol and aldosterone secretions
Increased incidence in females
Diagnosis is established if the amount of cortisol in the plasma and steroid in the urine do not increase after stimulation with adrenocorticotrophic hormone (ACTH)![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access