Fig. 18.1
Nodular lesion adjacent to the left uterosacral ligament: ectopic pregnancy in the retroperitoneal space
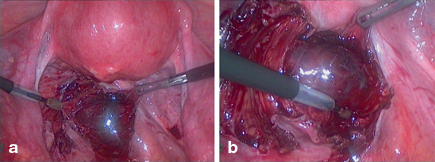
Fig. 18.2
a and b Mass containing the ectopic pregnancy in the retroperitoneal space
The optimal management of retroperitoneal pregnancy remains unclear [12]. To date, there have been less than 20 cases reported in the literature [3]. Nevertheless, their treatment options may be similar to those of the more frequent abdominal pregnancy. Compared to laparotomy, laparoscopic approach is associated with shorter operative time, reduced blood loss [4, 8, 16], less adhesion formation [4], less pain, and faster recovery [8]. Although laparoscopic approach is cost-effective and is the preferable approach to the treatment of abdominal and retroperitoneal pregnancies [3, 4, 7], laparotomy should be considered in patients with extensive intraperitoneal bleeding, intravascular compromise, or poor pelvic visualization at the time of laparoscopy [3]. It is important to have an early diagnosis [12, 17]. The possible risk of uncontrolled bleeding from the placental bed associated with the removal of the products of conception can be reduced with preoperative administration of methotrexate [13, 16] or selective arterial embolization [4, 16]. No mortality associated with this type of pregnancy has been reported.
Medical treatment with systemic methotrexate has also been reported without the need for further surgery [4, 16]. In fact, a few pregnancies of unknown location could be retroperitoneal pregnancies. Yet, none of the reported cases of retroperitoneal ectopic pregnancy has been successfully treated by systemic methotrexate alone [12] and an immediate surgical treatment on presentation seems to be the preferred approach [17]. Recent data suggest that a combination of methotrexate and gefitinib, a small-molecule thyrosin kinase inhibitor that blocks epidermal growth factor (EGF) receptor signaling, might lead to a rapid decline in hCG levels compared with methotrexate alone. However, this treatment should not be used until its efficacy and safety is confirmed [19].
Outcome of the Case
The patient was discharged 48 h after surgery. The serum β-hCG levels declined rapidly after surgery. Expecting management to wait for a spontaneous resolution would not be appropriate due to the gestational weeks of the patient, the progressive increase in the β-hCG levels, and the risk of gestational sac rupture and massive hemorrhage.
If both the uterus and adnexa are normal during laparoscopic exploration, unusual location of ectopic pregnancy should be considered. Through examination of the entire abdominal cavity including the retroperitoneum should be performed [3]. The increasing number of pregnancies after ARTs increases the risk of ectopic pregnancies including implantation at unusual sites, with a more difficult diagnosis and a high risk of life-threatening complications [3].
Clinical Pearls/Pitfalls
Retroperitoneal ectopic pregnancy is a rare condition, but must be considered in pregnancies of unknown location.
Laparoscopic approach is preferable than laparotomy.
Medical management with methotrexate could be considered in retroperitoneal pregnancies after an early diagnosis in a stable patient.
Methotrexate use for ectopic pregnancies does not seem to affect future ovarian reserve and pregnancy.



