32 Respiratory Symptoms
Of all symptoms that very ill children experience, perhaps the most dreaded and disturbing to patients, parents, and caregivers are pain and difficulty breathing. With regard to the latter, common respiratory difficulties encountered are related to a wide spectrum of conditions. These include illnesses that cause systemic problems such as weakness, anemia, or cystic fibrosis. Other times, localized problems such as airway abnormalities, swallowing problems, aspiration of secretions, or pneumonia may cause breathing difficulties. Metastases from cancer may cause widespread disease within the entire thorax, including multiple tumors, pleural effusions, pneumothorax, or airway compression. This list is by no means exhaustive, but gives some idea as to the variety of causes that can lead to disturbing respiratory symptoms in children, particularly toward the end of life. However, not all respiratory symptoms are necessarily progressive, and are sometimes transient as children recover from other life-threatening illnesses (Fig. 32-1).
Apart from physical or mechanical derangements that lead to breathing problems, anxiety can also compound feelings of shortness of breath and/or difficulty swallowing. There is clearly a role for many specific skills of different health professionals and caregivers to maximize a patient’s comfort. These include numerous psychological strategies,1 careful positioning of the patient, artificial ventilatory supports, and medications. Additionally, children require clear explanations for these distressing symptoms, and reassurance that we will work together to alleviate them.
This interdisciplinary approach to care becomes even more important over time, because as technology continues to develop more children who would have died because of their underlying illness now survive. In this context, some of the therapies used to assist with respiratory symptoms also extend life, but with residual respiratory symptoms or limitations lingering in the background. Examples of these therapies range from treating pneumonia with new generation antibiotics to receiving a lung transplant for cystic fibrosis. In other situations, children who cannot be cured of their disease might have their lives extended by months or years by noninvasive ventilation, such as facemask or nose cradle, or tracheostomy, with or without chronic mechanical ventilation. The number of children who live in the hospital or at home requiring respiratory support by biphasic positive airway pressure (BiPAP), continuous positive air pressure (CPAP) or continuous mechanical ventilation by way of tracheostomy has grown significantly in the past decade.2 Despite this, there are some who believe these procedures are underused in pediatric populations.3 In addition to the array of medical equipment and operative procedures that may alleviate respiratory symptoms, there are also many medical therapies that may be employed, which will be described later in more detail.
Dyspnea
Dyspnea is “a distressful subjective sensation of uncomfortable breathing that may be caused by many disorders, including certain heart and respiratory conditions, strenuous exercise, or anxiety.”4 The differential diagnosis is vast, and the causes can perhaps best be organized by anatomic location. Dyspnea can result from:
In terms of assessing dyspnea, two self-report tools could be located.5,6 One has been tested only in hospitalized patients with asthma, and the other has been limited to small focus groups of children with cystic fibrosis or asthma, compared to normal children. They were found to be reliable in children 6 or 8 years of age, respectively, but not younger. In the absence of any validated tool for dyspnea in other diseases, visual analogue scales (VAS) can also be used for children in these age ranges.
There are many studies evaluating both pharmacologic and non-drug treatment of this distressing problem. Results from meta-analyses in the Cochrane Database of systematic reviews are mixed:7
Many children anecdotally do respond positively to practicing deep, slow breathing, singing, or blowing bubbles or pinwheels when they are feeling anxious and short of breath. The use of self-hypnosis in children to manage dyspnea has also been found to be beneficial.8 This may be directed for younger children by a professional skilled in hypnotherapy. Pediatricians and others can learn to help their patients learn self-hypnosis, which gives the child more immediate and constant access to this form of therapy, through the Society for Developmental and Behavioral Pediatrics. Maintaining a calm and quiet environment is also important, and can be accentuated by use of machines that create light patterns on the ceiling, relaxation carts such a Snoezelen, and favorite music being played quietly.
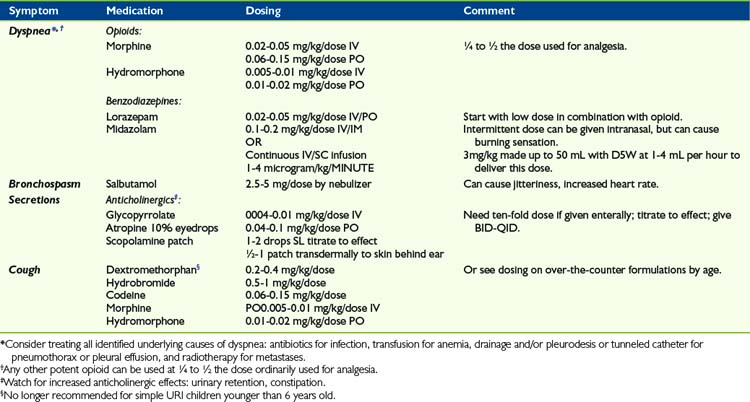
As for drug treatment of dyspnea, the mainstay medications are opioids and benzodiazepines, titrated to minimal effective dose (Table 32-1). There is sometimes an exaggerated concern on the part of health professionals and parents that initiating opioids to treat dyspnea may cause respiratory depression. Very often, the dose of opioid required for the treatment of dyspnea is a quarter to half that required for the treatment of pain. A recent Cochrane review did report benefits of opioid therapy in ameliorating breathlessness in patients due to both malignant and non-malignant disease.9 Although the number of studies was small, the results were significant when these medications were given via the enteral or parenteral route. Educating families and colleagues that judicious use of opioids have been found to be safe and beneficial often allays these fears. Also, opioids can sometimes be used transiently, while other therapies aimed at ameliorating the cause of the dyspnea can be employed and given time to take effect. In addition to systemic administration of opioids, there have been many studies evaluating the possible role of inhaled opioid agonists, the theory being that this might confer a direct benefit by stimulating mu receptors in the lungs themselves, thereby reducing systemic side effects such as pruritis, somnolence, and constipation. A recent meta-analysis reveals that this mode of therapy is not beneficial, even in dose ranges from 1 to 40 mg morphine equivalent,10 despite isolated case reports showing positive effects.
There is no meta-analysis that evaluates the use of benzodiazepines for relief of dyspnea, though the Cochrane Database has a published protocol for such a study. Other published clinical trials in adults have demonstrated that use of midazolam, in addition to morphine, can further diminish the sensation of dyspnea.11 There are no similar trials in children, but the combination of morphine or another opioid in conjunction with benzodiazepines are frequently used to treat this symptom in children despite the paucity of data for both children and adults. Occasionally, suffering from symptoms such as dyspnea becomes intractable, despite multiple combined treatments. In this event, many patients and/or families agree to a course of sedation as a last resort to provide comfort, although conscious awareness may be very diminished as a consequence.12 This treatment might be continued until death occurs, but certainly not always if other treatments such as radiotherapy alleviate the symptom over time in such a way that sedation can be lessened or discontinued. In one study, such sedation was eventually discontinued in a quarter of adult patients.13
Other medications that may provide relief, depending on the underlying disease, are bronchodilators, inhaled steroids, or mucolytics.14 Many patients suffer from orthopnea, and occupational therapists and physiotherapists can often combine their skills to devise modifications to beds and seating such that the patient can maintain a comfortable position even during sleep. Other helpful therapies that may assist with dyspnea include use of a fan for increased air movement in the room. Patients experiencing dyspnea also often feel less symptomatic at an incline of 30 degrees to 90 degrees.
The role of oxygen has been controversial in the management of dyspnea. However, in a 2008 study, patients dying of metastatic lung disease and receiving oxygen therapy were no less dyspneic than those receiving only room air.15 However, oxygen therapy may have a symbolic role for families, particularly if their child has required oxygen frequently throughout his or her life. Therefore, many patients and families do request that oxygen be provided, particularly in home settings. Having oxygen to provide often seems to enhance patient and parental sense of control, and can be important from that point of view.
Cough
A very aggravating symptom is cough. Cough interferes with activities as basic as eating and sleeping, and also as far-reaching as social isolation that prevents one from attending concerts, movies, etc. Moreover, cough leads to fatigue, abdominal or chest pain, and even vomiting and rib fractures. Persistent cough is a serious problem that healthcare professionals sometimes minimize, perhaps because everyone has had a cough at one time or other. Again, medical treatment to this point is somewhat limited, given that mechanical factors such as secretions in the alveoli and bronchi, and irritation of the carina, are potent stimuli of the cough reflex. No meta-analysis looking at treatment of cough in palliative care could be located. Cough may respond to N-methyl-d-aspartate (NMDA) receptor antagonists, such as dextromethorphan. This is often available in low-dose formulations in over-the-counter cough preparations. There are no controlled trials in children evaluating its role in cough due to progressive respiratory illness. However, one study demonstrated more improvement in parent-report of cough compared with placebo when used for viral upper respiratory infection, though not as effective as ingesting honey.16 Some patients get a measure of relief from a relatively small dose of opioid.17 However, for those with a lesion in the bronchi, cough can be fairly intractable without more intense treatments, such as radiotherapy or surgery. With regard to radiotherapy, an area of lung or total lung can be targeted when there is diffuse parenchymal disease, but in the case of bronchial tumors, this can be administered by endobronchial brachytherapy. This is accomplished by delivering a radioactive treatment via an endoscopically placed catheter, which is left in place for a few minutes, then removed.18,19
Secretions
When loss of airway control is caused by imminent death, and causes caregivers distress, it can be treated by a variety of anticholinergic medications, although the evidence for these strategies is quite weak.20 One noninvasive strategy is to use 10% atropine eyedrops sublingually, titrated to effect. Another is to use a scopolamine patch applied transdermally behind the patient’s ear. Systemic medications such as glycopyrrolate can also be used, either enterally or parenterally, and this particular medication has the added advantage of not crossing the blood-brain barrier. These medications need to be carefully titrated such that secretions do not become too thick or tenacious. If this complication arises, secretions may become much harder to move within the airways, leading to the formations of large, solid mucous plugs, which can then worsen the child’s respiratory symptoms. In these situations, families and caregivers also need to be alert to other anticholinergic symptoms, such as urinary retention, which sometimes requires indwelling urinary catheterization, dry mouth, and worsening constipation.
Pleural Effusions and Pneumothorax and/or Hemothorax
A pleural effusion, accumulation of fluid between the lung and chest wall, or pneumothorax, collection of air between the lung and the chest wall, may be asymptomatic when it is small. However, as they enlarge, they often cause increasing dyspnea. Depending on the child’s overall disease trajectory, more conservative attempts to control symptoms might be limited to medications if the child is believed to be very advanced in the course of the underlying disease. On the other hand, if the child is relatively well overall, it often is reasonable to consider other options, including surgery and/or radiotherapy. For malignant pleural effusion, it is not worthwhile to place a chest tube as a sole therapy only transiently, as the effusion will doubtlessly re-accumulate, often within days. Many patients complain of increased pain at the chest tube site for the entire time it is in place, and this discomfort needs to be anticipated and weighed against the benefit that might be conferred by its placement. Surgeries undertaken often include the insertion of pigtail catheters or chest tubes for emergency drainage, and sometimes pleurodesis once the effusion is drained. Pleurodesis is a process by which the pleural surfaces of the chest wall and the lung can be intentionally inflamed by reaction to placement of foreign material in this space, with the goal that the two pleural surfaces permanently adhere to each other, avoiding recurrence of the pneumothorax or pleural effusion. A recent review in adult patients did show that pleurodesis is preferentially done thorascopically rather than by thoracotomy, given the more minimal nature of the former therapy, and that talc is the material of choice to seal the pleural surfaces together.21
A more recent innovation is the insertion of a tunneled catheter for control of malignant pleural effusion. These are increasingly being used for ambulatory adult patients, and can often be inserted by a thoracic surgeon as an outpatient procedure.22 This procedure involves placing a tunneled catheter under the skin and subcutaneous tissue, through the thorax, and into the pleural collection of fluid. The exterior portion of the catheter can then be attached to a sterile collection bottle to perform serial drainages of the effusion as it re-accumulates, to maintain comfort. A 2006 local study23 of 250 insertions in adults suggested that this approach is superior compared with talc pleurodesis, due primarily to the avoidance of a days-long hospital admission and long duration of result, usually until patients’ deaths (Fig. 32-2).
Weakness of respiratory musculature
Children with such diseases are highly symptomatic from a respiratory standpoint. The degree and timing of weakness is variable, depending upon the underlying condition. Symptoms caused by these diseases include dyspnea, swallowing difficulties, resultant excessive oral secretions, and aspiration of feeds and secretions. Recently, more and more families have been advocating for significant respiratory intervention for these children, including long-term CPAP, BiPAP, or tracheostomy and ventilation. With the first two forms of noninvasive ventilation support, children with diseases such as SMA 1 might have life expectancy lengthened from a few months to somewhere into the first decade of life. For many parents, these forms of respiratory supports cannot be emphasized enough in terms of their importance in their child’s care. To that end, many parents correspond through a variety of websites, including www.curesma.org, and have become strong advocates for parents newly adjusting to this serious diagnosis. This has certainly resulted in globalization of medical advice. It is not uncommon for families from around the world to be corresponding with each other, or even with clinicians. This can sometimes be problematic, as parents seek to be involved in clinical trials for their children in other cities, or even foreign countries, but find that practical limitations of their child’s ability to travel, or insurance and other issues, will preclude their participation.24–26 Parents often feel over time that they would be better off in other treatment centers, and this can lead to feelings of frustration and distrust of local care providers, despite the fact that the day-to-day care will include all proven therapies for these incurable diseases.
Recent consensus suggests that combination therapy of noninvasive ventilation, gastrostomy feeding and fundoplication, and use of a mechanical insufflation/exsufflation machines that mimic cough, extend life.27 The Cough Assist® machine mimics a cough. When a healthy person coughs, it is preceded by a deep inspiration. With insufflation/exsufflation machines, this is mechanically simulated by applying positive pressure to the airways, followed by rapid switch to a negative pressure through a facemask. This often moves secretions higher into the airway or pharynx to allow for improved suctioning of deeper or inspissated secretions.28 However, despite the advances demonstrated in this most recent consensus statement, the same publication contends that it remains unclear as to which is ethically the more correct path; extension of life through these technologies, or providing care directed at comfort only, but resulting in much earlier death (Fig. 32-3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree