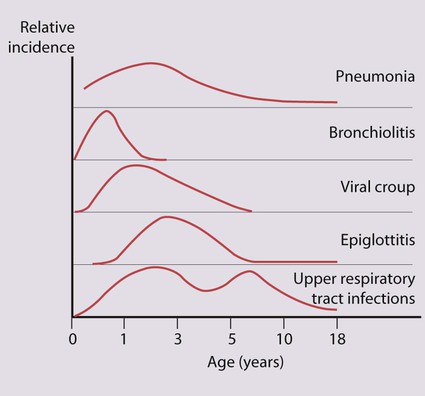
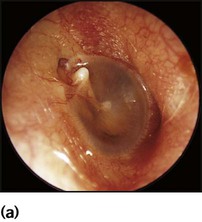
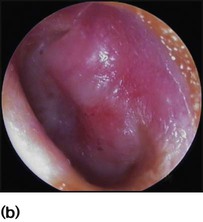
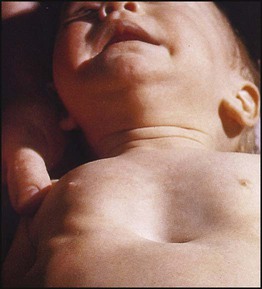
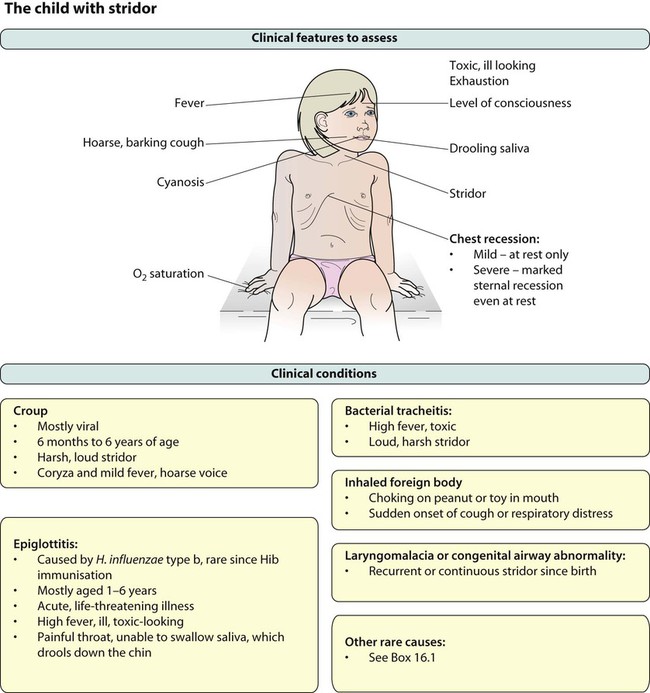
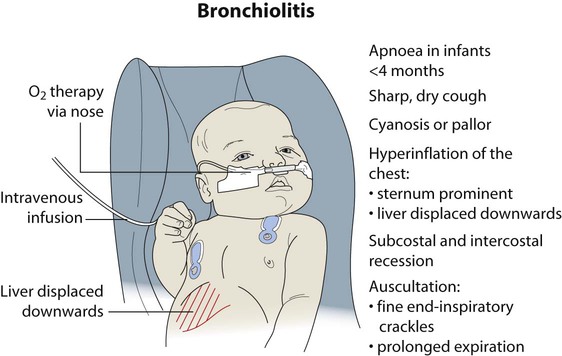
Notable features of respiratory disorders are: • Worldwide, respiratory disorders are the most common cause of death in children • In the UK, respiratory disorders account for 50% of consultations with general practitioners for acute illness in young children and a third of consultations in older children • Respiratory disorders are responsible for about 25% of acute paediatric admissions to hospital, some of which are life-threatening • Asthma is the most common chronic illness of childhood in the UK • Cystic fibrosis is the most common inherited life-limiting disorder in Caucasians. • Parental smoking, especially maternal • Poor socioeconomic status – large family size, overcrowded, damp housing • Underlying lung disease – such as bronchopulmonary dysplasia in infants who were born preterm, cystic fibrosis or asthma • Haemodynamically significant congenital heart disease • Immunodeficiency (either primary, see Ch. 14, or secondary, e.g. from HIV infection or chemotherapy). The child’s age influences the prevalence and severity of infections (Fig. 16.1). It is in infancy that serious respiratory illness requiring hospital admission is most common and the risk of death is greatest. There is an increased frequency of infections when the child or older siblings start nursery or school. Repeated upper respiratory tract infection is common and rarely indicates underlying disease. Most children will have at least one episode of acute otitis media (OM). This is most common at 6–12 months of age. Up to 20% will have three or more episodes. Infants and young children are prone to acute otitis media because their Eustachian tubes are short, horizontal and function poorly. There is pain in the ear and fever. Every child with a fever must have their tympanic membranes examined (Fig. 16.2a–d). In acute otitis media, the tympanic membrane is seen to be bright red and bulging with loss of the normal light reflection (Fig. 16.2b). Occasionally, there is acute perforation of the eardrum with pus visible in the external canal. Pathogens include viruses, especially RSV and rhinovirus, and bacteria including pneumococcus, non-typeable H. influenzae and Moraxella catarrhalis. Serious complications are mastoiditis and meningitis, but are now uncommon. Pain should be treated with an analgesic such as paracetamol or ibuprofen. Regular analgesia is more effective than intermittent (as required) and may be needed for up to a week until the acute inflammation has resolved. Most cases of acute otitis media resolve spontaneously. Antibiotics marginally shorten the duration of pain but have not been shown to reduce the risk of hearing loss (see Ch. 5). It is often useful to give the parents a prescription, but ask them to use it only if the child remains unwell after 2–3 days. Amoxicillin is widely used. Neither decongestants nor antihistamines are beneficial. Recurrent ear infections can lead to otitis media with effusion (OME or glue ear or serous otitis media). Children are asymptomatic apart from possible decreased hearing. The eardrum is seen to be dull and retracted, often with a fluid level visible (Fig. 16.2c). Confirmation of otitis media with effusion can be gained by a flat trace on tympanometry, in conjunction with evidence of a conductive loss on pure tone audiometry (possible if >4 years old), or reduced hearing on a distraction hearing test in younger children. Otitis media with effusion is very common between the ages of 2 and 7 years, with peak incidence between 2.5 and 5 years. This condition usually resolves spontaneously. Cochrane reviews have shown no evidence of long-term benefit from the use of antibiotics, steroids or decongestants. Otitis media with effusion is the most common cause of conductive hearing loss in children and can interfere with normal speech development and result in learning difficulties in school. In such children insertion of ventilation tubes (grommets, Fig. 16.2d) can be beneficial, but there is evidence, again from Cochrane reviews, that adenoidectomy can offer more long-term benefit. It is believed that the adenoids can harbour organisms within biofilms that contribute to infection spreading up the Eustachian tubes. In addition, grossly hypertrophied adenoids may obstruct and affect the function of the Eustachian tubes, leading to poor ventilation of the middle ear and subsequent recurrent infections. In practice, children with recurrent URTIs and chronic glue ear that do not resolve with conservative measures undergo grommet insertion. If these problems recur after grommet extrusion, reinsertion of grommets with adjuvant adenoidectomy is usually advocated. • Recurrent severe tonsillitis (as opposed to recurrent URTIs) – tonsillectomy reduces the number of episodes of tonsillitis by a third, e.g. from three to two per year, but is unlikely to benefit mild symptoms. • A peritonsillar abscess (quinsy) • Obstructive sleep apnoea (the adenoids will also normally be removed). The mucosal inflammation and swelling produced by laryngeal and tracheal infections can rapidly cause life-threatening obstruction of the airway in young children. Several conditions can cause acute upper airways obstruction (Box 16.1). They are characterised by: • Stridor, a rasping sound heard predominantly on inspiration • Hoarseness due to inflammation of the vocal cords • A barking cough like a sea lion The severity of upper airways obstruction is best assessed clinically by the degree of chest retraction (none, only on crying, at rest) and degree of stridor (none, only on crying, at rest or biphasic) (Fig. 16.3). There is intense swelling of the epiglottis and surrounding tissues associated with septicaemia. Epiglottitis is most common in children aged 1–6 years but affects all age groups. It is important to distinguish clinically between epiglottitis and croup (Table 16.1), as they require quite different treatment. Table 16.1 Clinical features of croup (viral laryngotracheitis) and epiglottitis The onset of epiglottitis is often very acute (see Case History 16.1), with: • high fever in an ill, toxic-looking child • an intensely painful throat that prevents the child from speaking or swallowing; saliva drools down the chin • soft inspiratory stridor and rapidly increasing respiratory difficulty over hours • the child sitting immobile, upright, with an open mouth to optimise the airway. Coryzal symptoms precede a dry cough and increasing breathlessness. Feeding difficulty associated with increasing dyspnoea is often the reason for admission to hospital. Recurrent apnoea is a serious complication, especially in young infants. Infants born prematurely who develop bronchopulmonary dysplasia or with other underlying lung disease, such as cystic fibrosis or have congenital heart disease, are most at risk from severe bronchiolitis. The characteristic findings on examination (Fig. 16.5) are:
Respiratory disorders
Respiratory infections
Host and environmental factors
Upper respiratory tract infection (URTI)
Acute infection of the middle ear (acute otitis media)
Tonsillectomy and adenoidectomy
Laryngeal and tracheal infections
Acute epiglottitis
Croup
Epiglottitis
Onset
Over days
Over hours
Preceding coryza
Yes
No
Cough
Severe, barking
Absent or slight
Able to drink
Yes
No
Drooling saliva
No
Yes
Appearance
Unwell
Toxic, very ill
Fever
<38.5°C
>38.5°C
Stridor
Harsh, rasping
Soft, whispering
Voice, cry
Hoarse
Muffled, reluctant to speak
Bronchiolitis
Clinical features
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Respiratory disorders