and Kentaro Sekiyama2
Keywords
Step-by-step radical hysterectomyParavesical spaceOkabayashi’s pararectal spaceLatzko’s pararectal spaceCardinal ligamentUterine arterySuperficial uterine veinDeep uterine veinAnterior (ventral) leaf of vesicouterine ligamentSuperior vesical veinCervicovesical vesselsPosterior (dorsal) leaf of vesicouterine ligamentMiddle vesical veinInferior vesical veinUterosacral ligamentRectovaginal ligamentParacolpium (vaginal blood vessels)6.1 Surgical Process of the Step-by-Step Radical Hysterectomy
6.1.1 Open the Abdominal Cavity
6.1.2 Exposure of the Pelvic Cavity
6.1.3 Visual and Manual Examination of the Spread of the Disease and Operability
6.1.4 Traction of the Uterus (Figure 6.1)
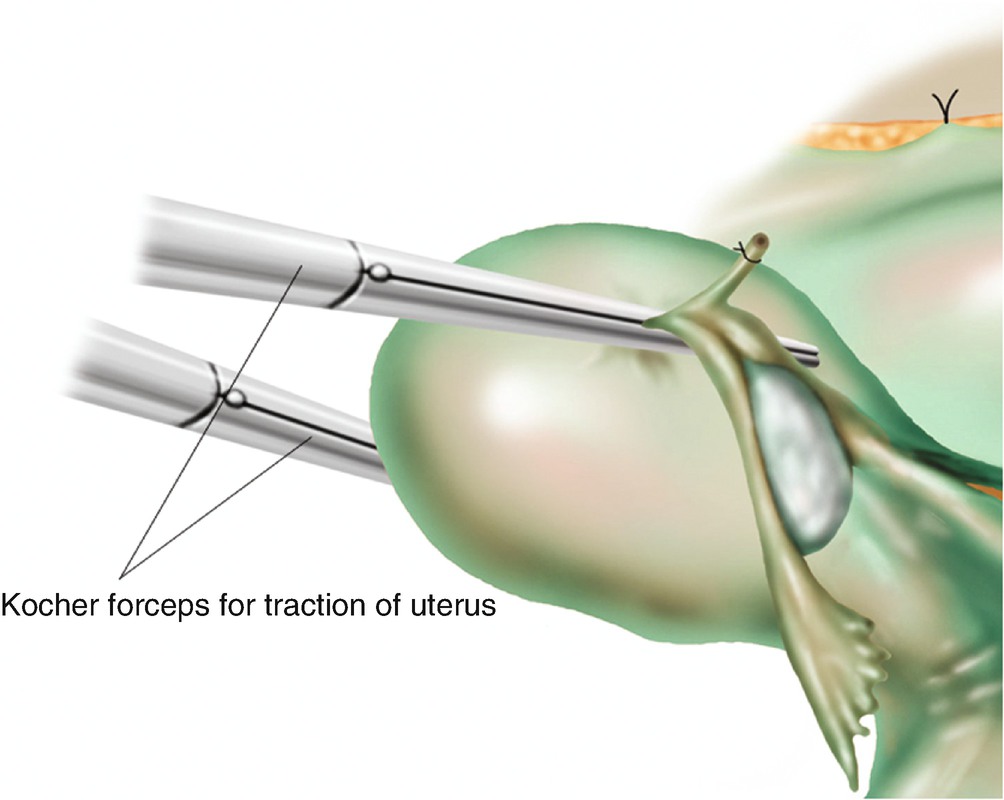
Traction of the uterus using two long Kocher forceps
6.1.5 Ligation and Division of the Round Ligament (Figure 6.2)
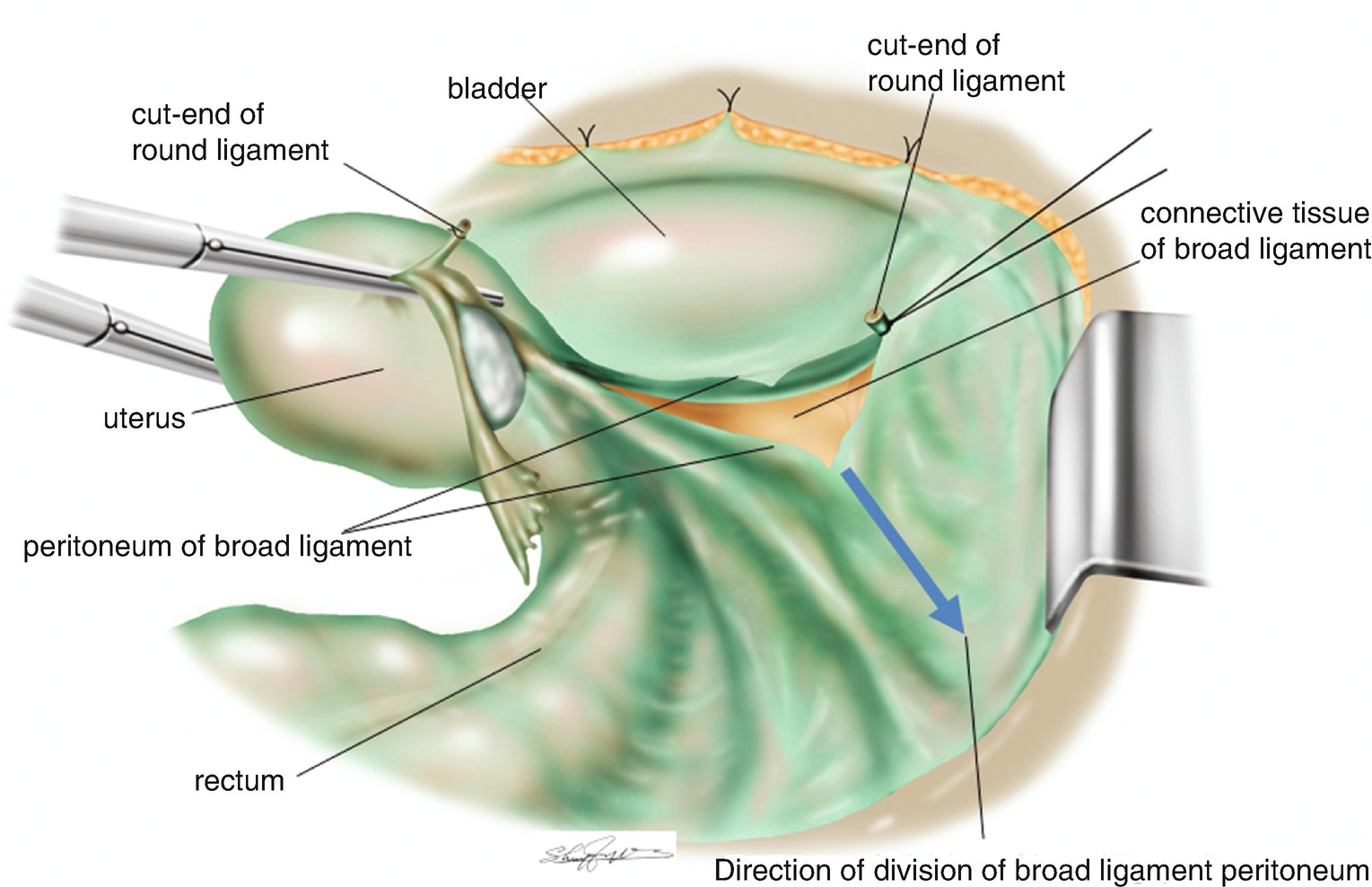
Ligation and division of the round ligament and the direction of the separation of the peritoneum of the broad ligament (blue arrow line)
6.1.6 Ligation and Division of the Suspensory Ligament of the Ovary (Ovarian Vessels) (Figure 6.3)
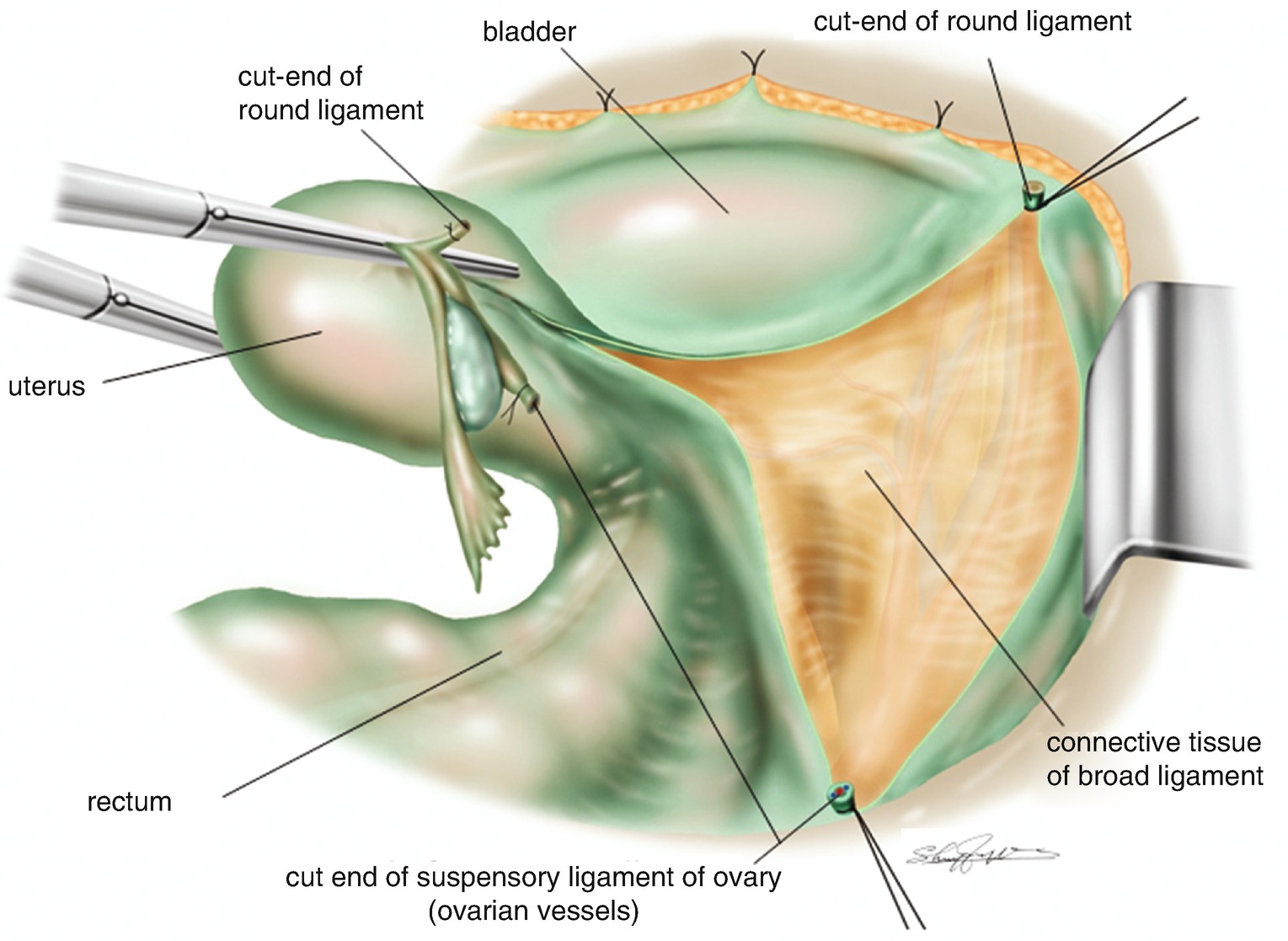
Ligation and division of the suspensory ligament of the ovary (ovarian vessels). The retroperitoneal space beneath the broad ligament is widely separated
6.1.7 Confirmation of the Ureter (Figure 6.4)
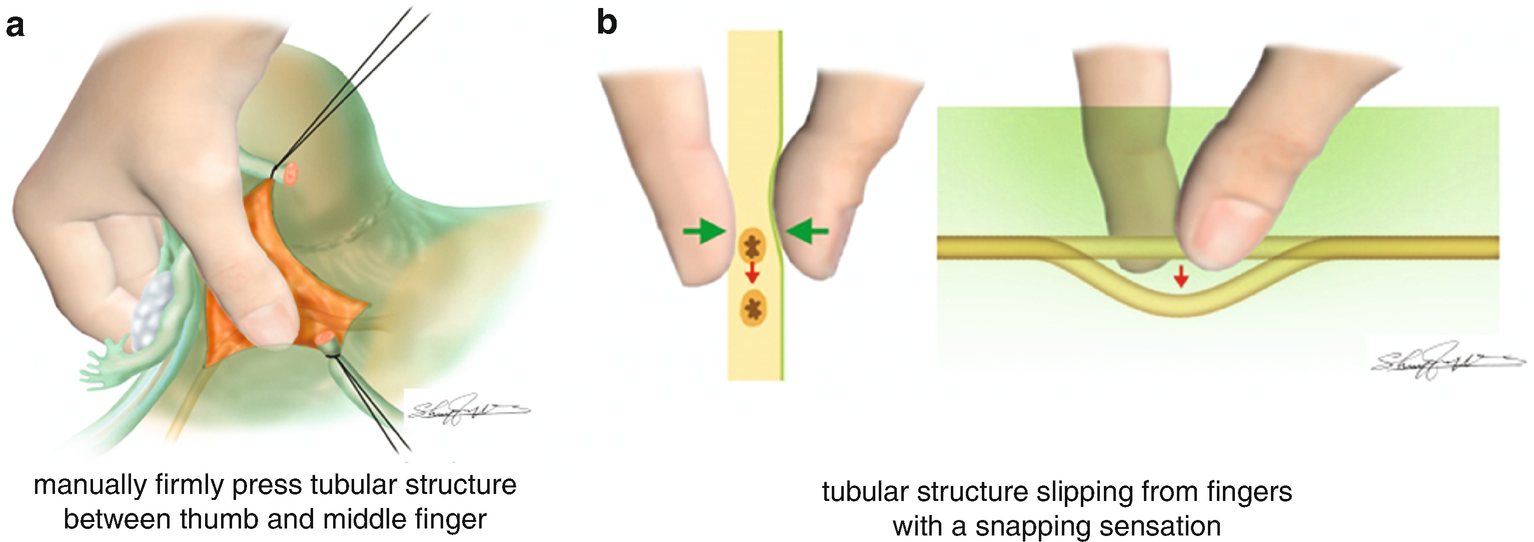
Manual confirmation of the ureter with fingers using thumb and middle fingers. (a) Putting the connective tissues of the broad ligament between thumb and middle fingers, search the tubular structure. (b) Press firmly the tubular structure with two fingers, then the ureter usually slips between the fingers and creates a snap sound (snapping sensation)
6.1.8 Isolation of the Ureter (Figure 6.5)
Isolation of the ureter. The ureter is isolated from the loose connective tissues beneath the rectal side of the broad ligament peritoneum
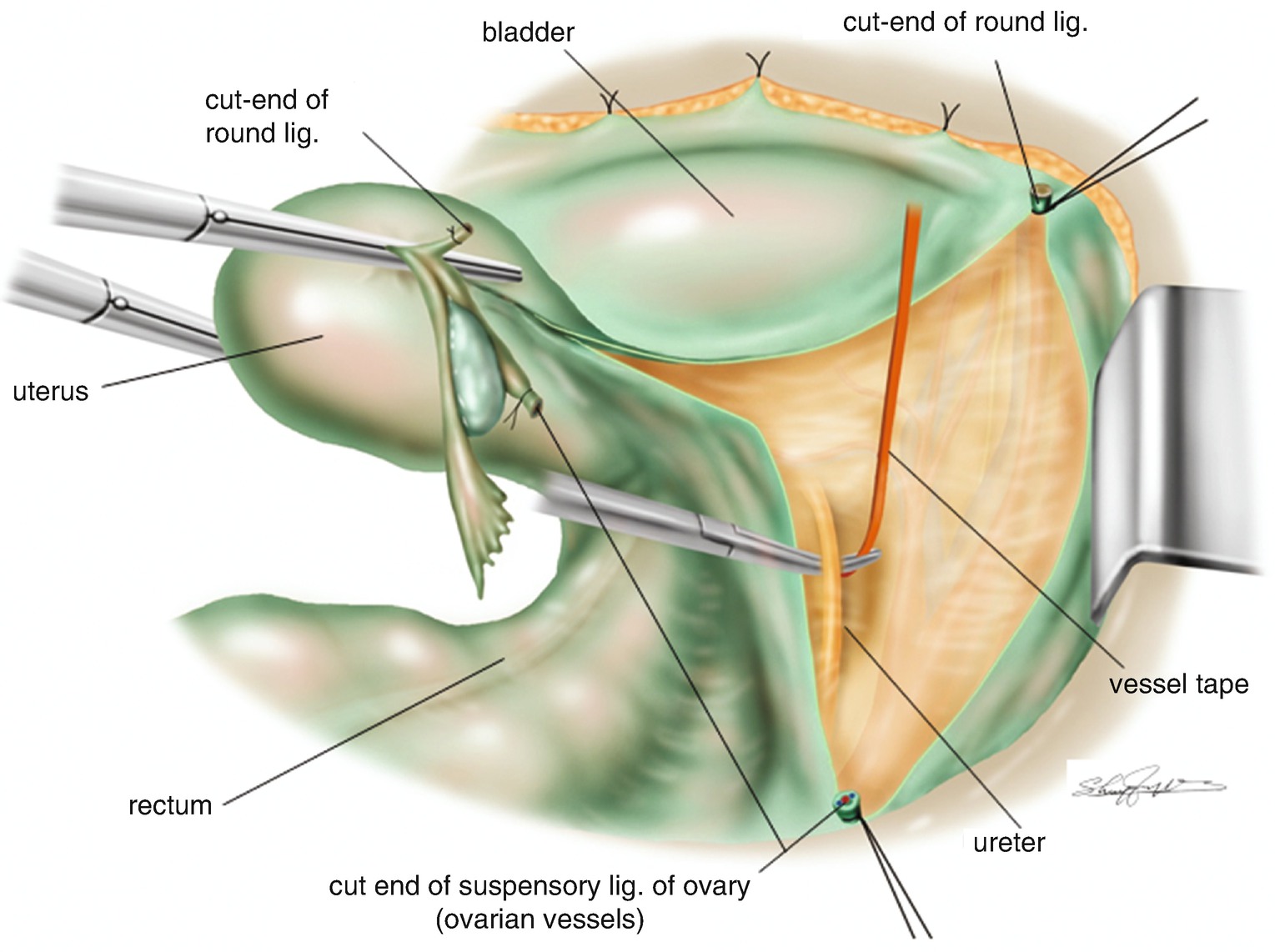
6.1.9 Application of a Vessel Tape for a Marker of the Ureter (Figure 6.6)
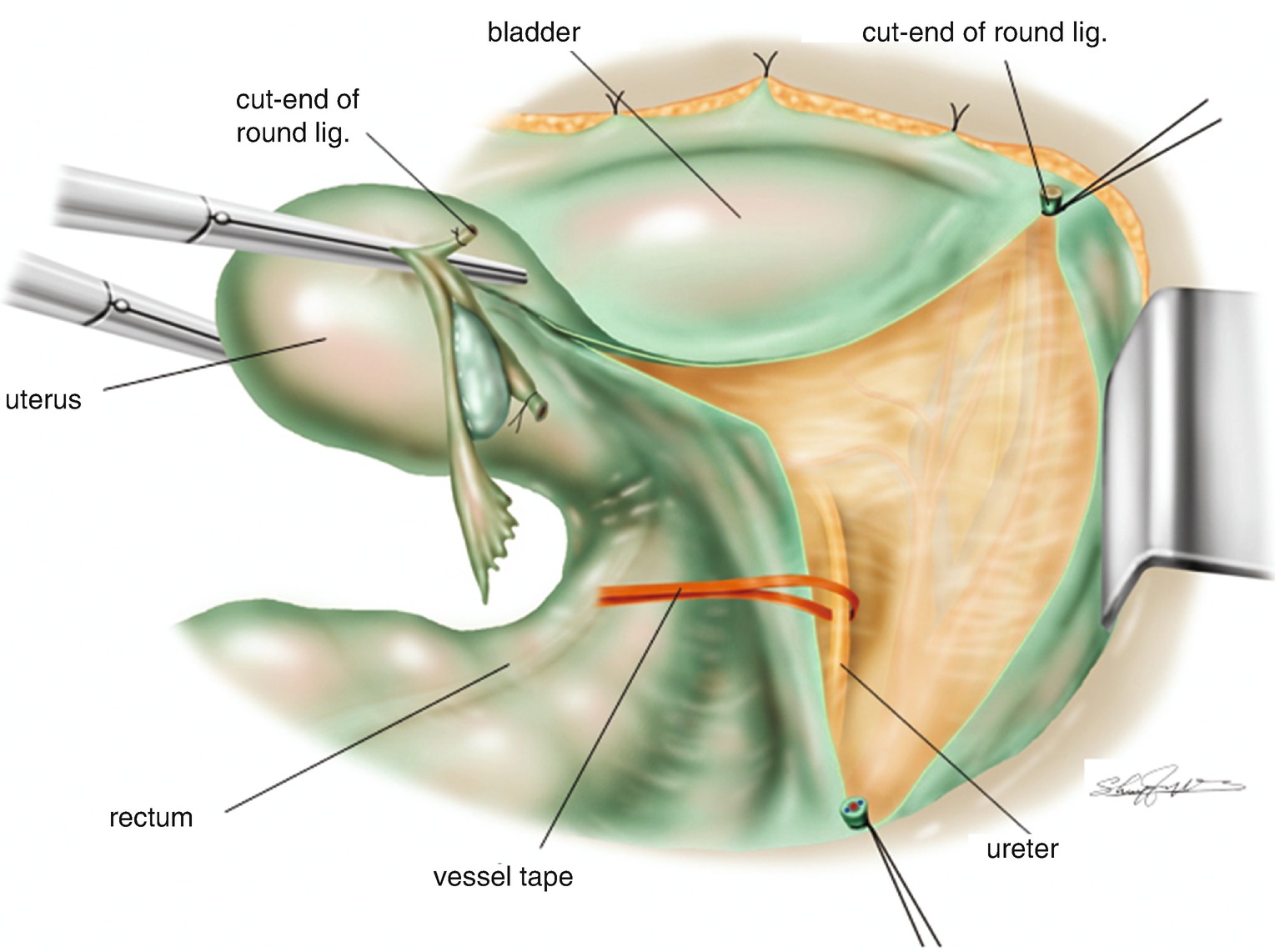
Application of a vessel tape for a marker of the ureter
6.1.10 Tentative Development of the Pararectal Space (Figure 6.7)
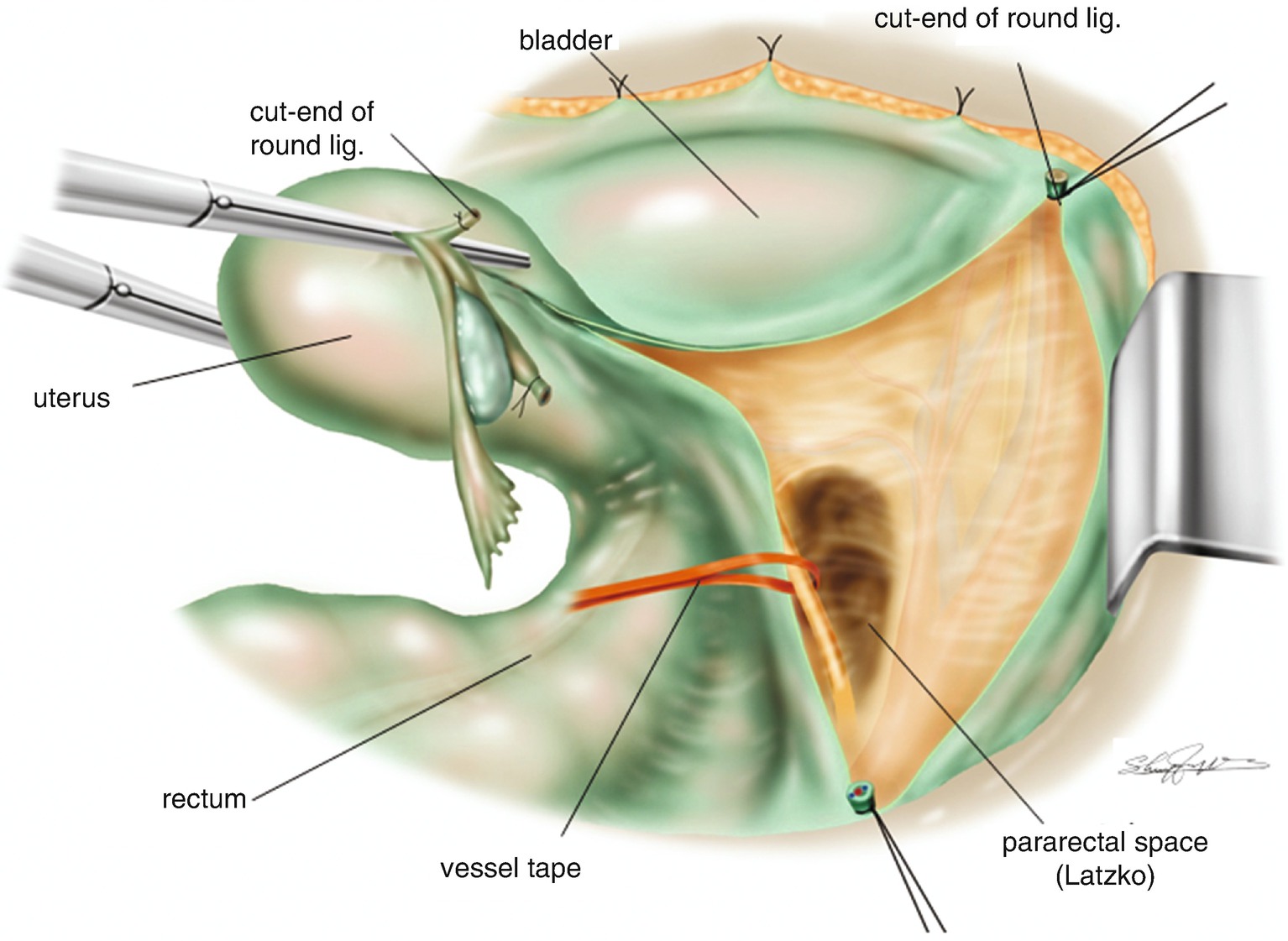
Tentative development of the pararectal space (Latzko)
6.1.11 Definition of the Pararectal Space (Figures 6.8 and 6.9)
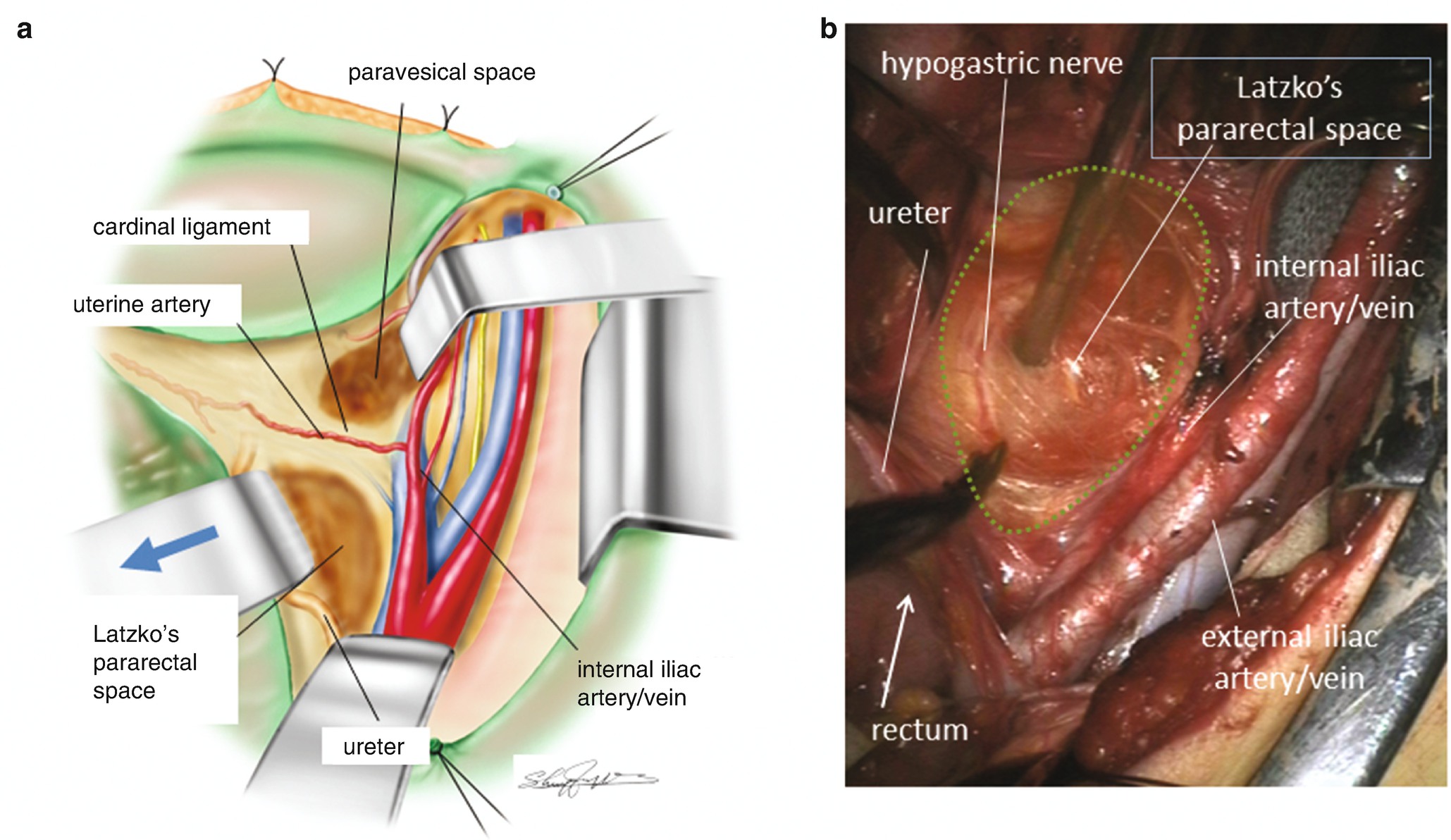
Definition of the pararectal space. (a) The relationship among the paravesical space, the cardinal ligament and the pararectal space (Latzko). (b) A surgical photo of the developed pararectal space between the rectal sidewall with the ureter and the internal iliac artery/vein. On the rectal sidewall of the pararectal space the hypogastric nerve accompanied by a small blood vessel is appreciated
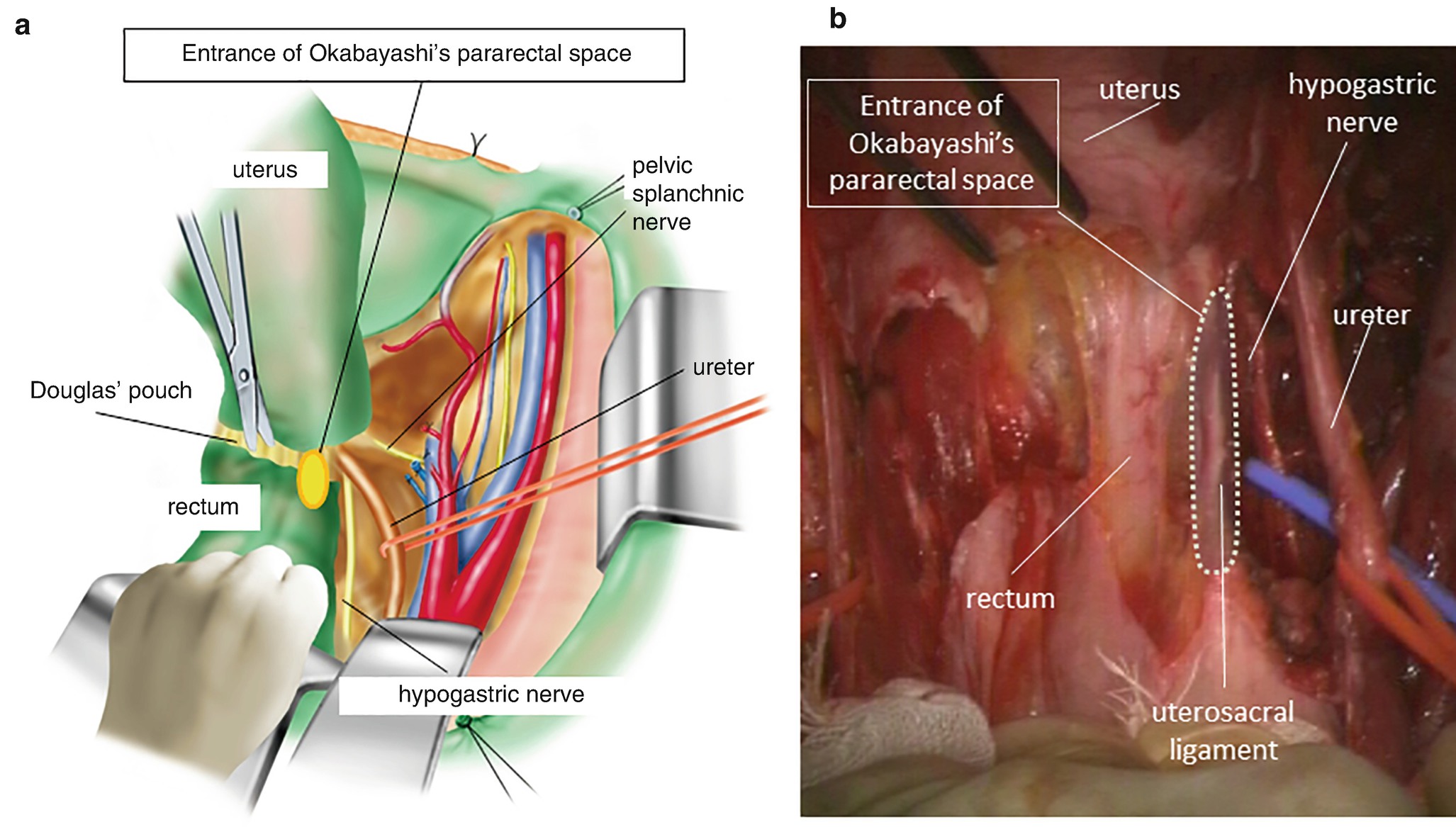
Anatomical location of Okabayashi’s pararectal space. (a) An oval-shaped orange circle filled with yellow color on the uterosacral ligament is the landmark of the entrance of Okabayashi’s pararectal space. (b) A surgical photo of Okabayashi’s pararectal space developed just between the rectal sidewall and the connective tissue plane that includes the ureter and the hypogastric nerve. This connective tissue plane resides between Okabayashi’s pararectal and Latzko’s pararectal space
In contrast, Okabayashi opened the pararectal space by the division of the uterosacral ligament and usually divided the hypogastric nerve. Therefore, Okabayashi’s pararectal space is developed just close to the rectal sidewall retracting the isolated ureter to the pelvic sidewall (Figure 6.9a, b). In order to increase the mobility of the uterus, Okabayashi preferred to open the space from the uterosacral ligament. Between Latzko’s and Okabayashi’s pararectal space, the hypogastric nerve is appreciated parallel to the ureter as shown in Figure 6.8b. In order to extend Okabayashi’s pararectal space toward Latzko’s pararectal space, it is necessary to divide the hypogastric nerve, which in turn increases the mobility of the uterus.
6.1.12 The Ureter and the Hypogastric Nerve Are on the Same Connective Tissue Plane (Figure 6.10)
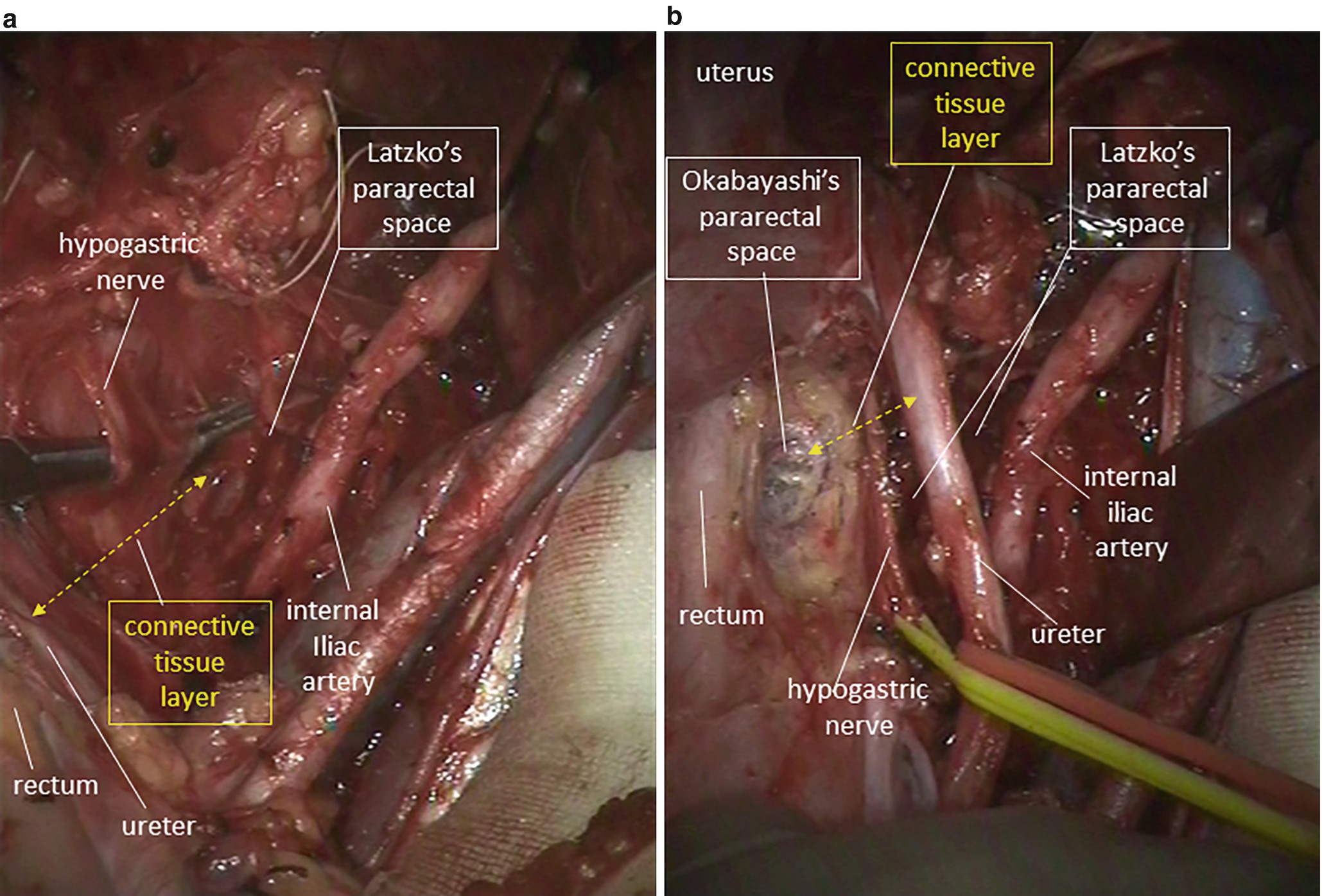
Anatomical relationship between Okabayashi’s pararectal space and Latzko’s pararectal space. (a) On the rectal sidewall of Latzko’s pararectal space, the ureter and the hypogastric nerve are appreciated on the same connective tissue plane (a dotted line with bidirectional arrow). (b) Okabayashi’s pararectal space is medially developed between the rectum and the connective tissue plane of the ureter and hypogastric nerve that was the rectal sidewall of Latzko’s pararectal space
6.1.13 Division of the Peritoneum at Pouch of Douglas (Figure 6.11)
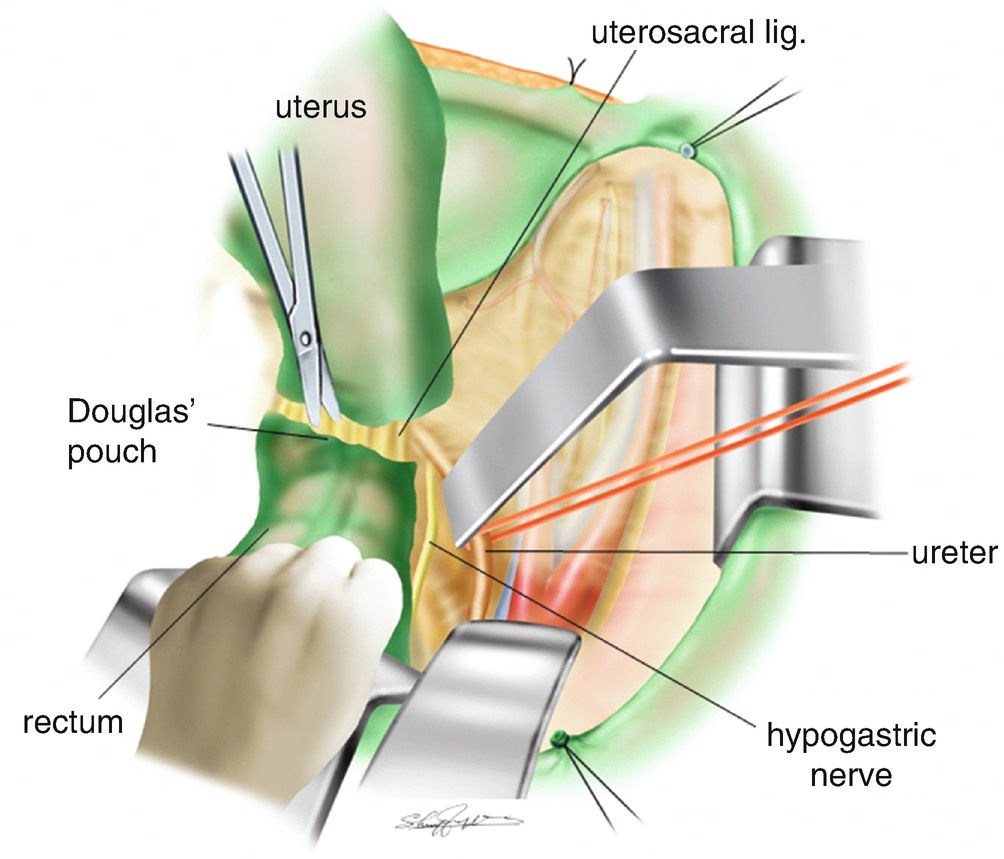
Division of the peritoneum of the Douglas’ pouch
6.1.14 Separation of the Peritoneum of the Vesicouterine Pouch (Figure 6.12)
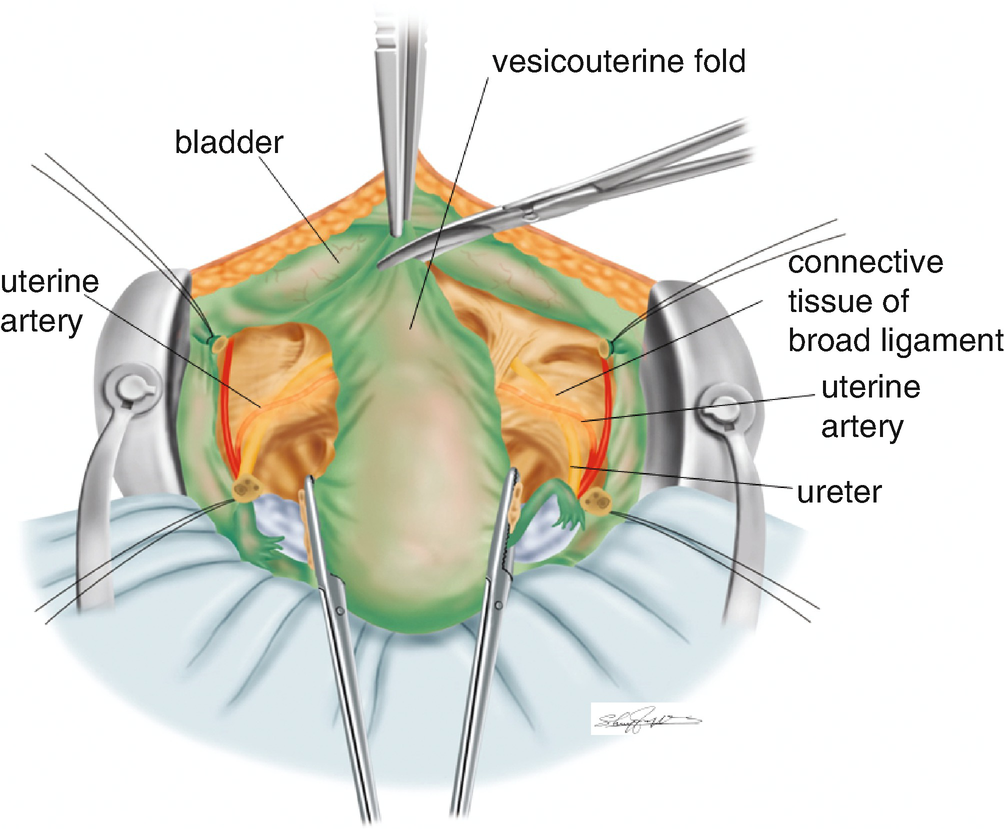
Separation of the peritoneum of the vesicouterine pouch
6.2 Pelvic Lymphadenectomy
6.2.1 Lymph Nodes in the Pelvis (Figure 6.13)
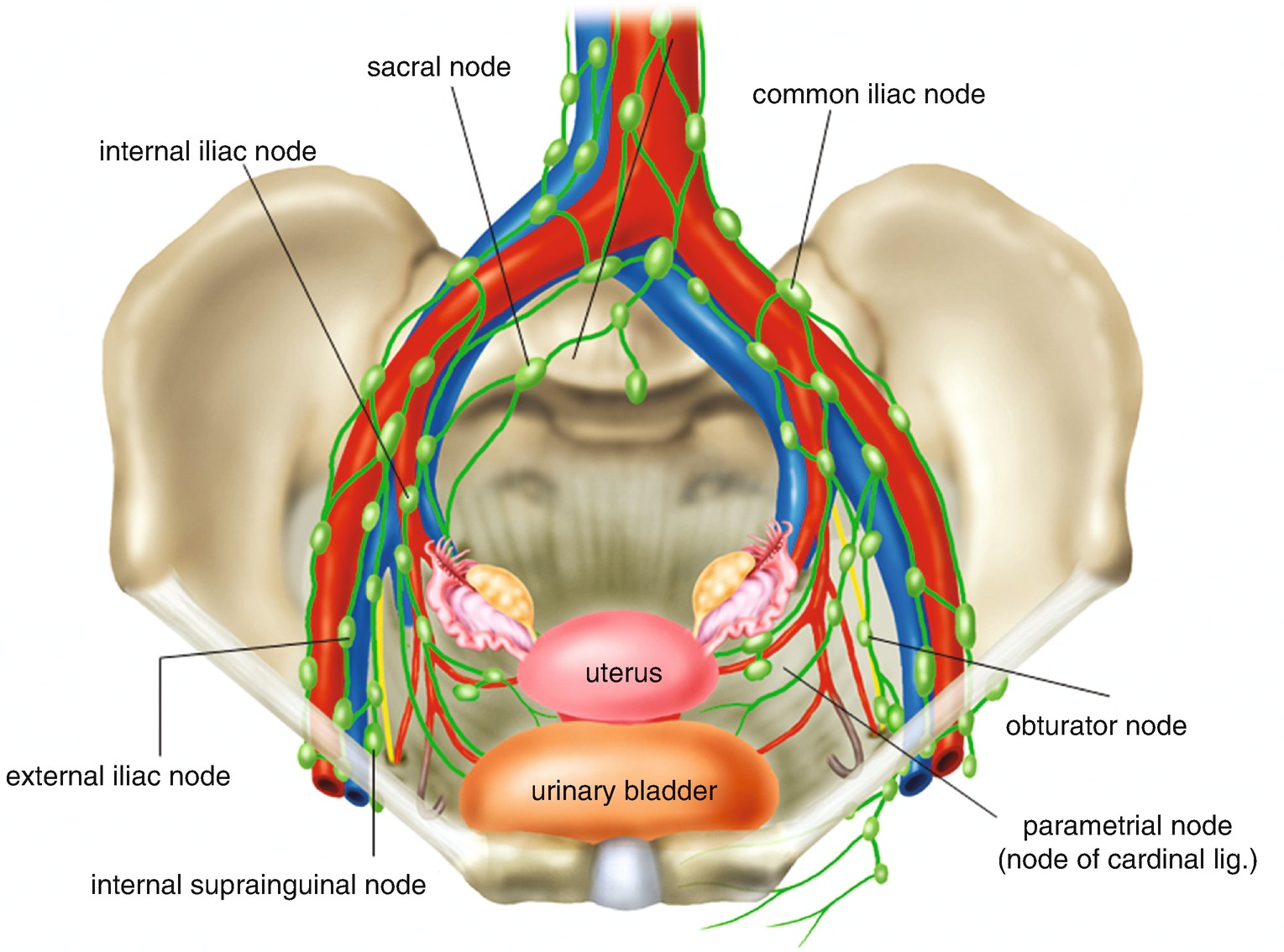
Lymph nodes in the pelvis
6.2.2 Exposure of the Adipose Tissue in the Supra-Inguinal Area (Figure 6.14)
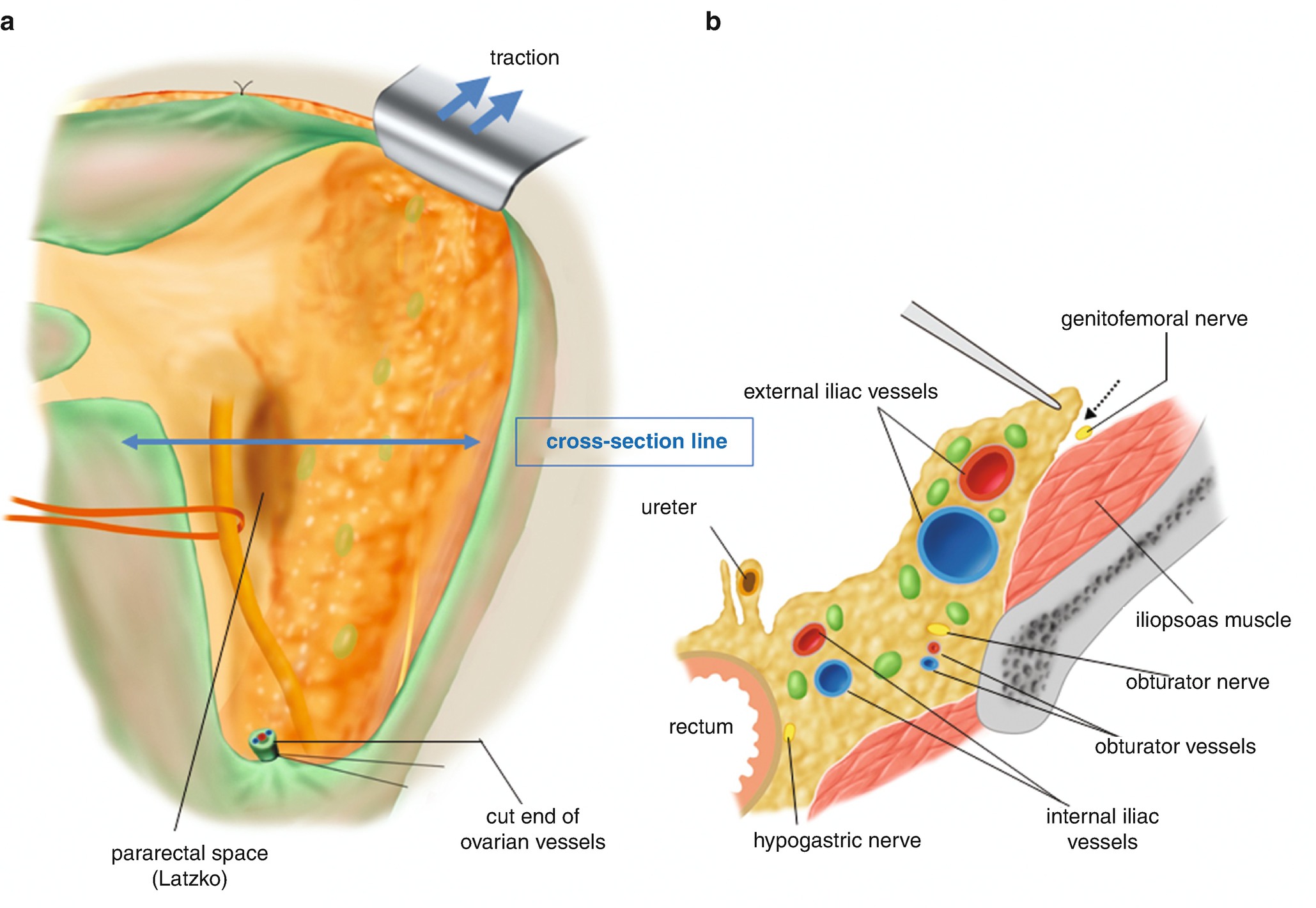
Exposure of the adipose tissues in the supra-inguinal area. (a) Exposed retroperitoneal adipose tissues of the broad ligament. (b) A cross-sectional view of the retroperitoneal structures in the pelvis at the level of a two-directional arrow (cross-sectional line) drawn in Figure 6.14a. A dotted arrow line indicates the separation point of the connective tissue from the iliopsoas muscle
6.2.3 Exposure of the Iliopsoas Muscle (Figure 6.15)
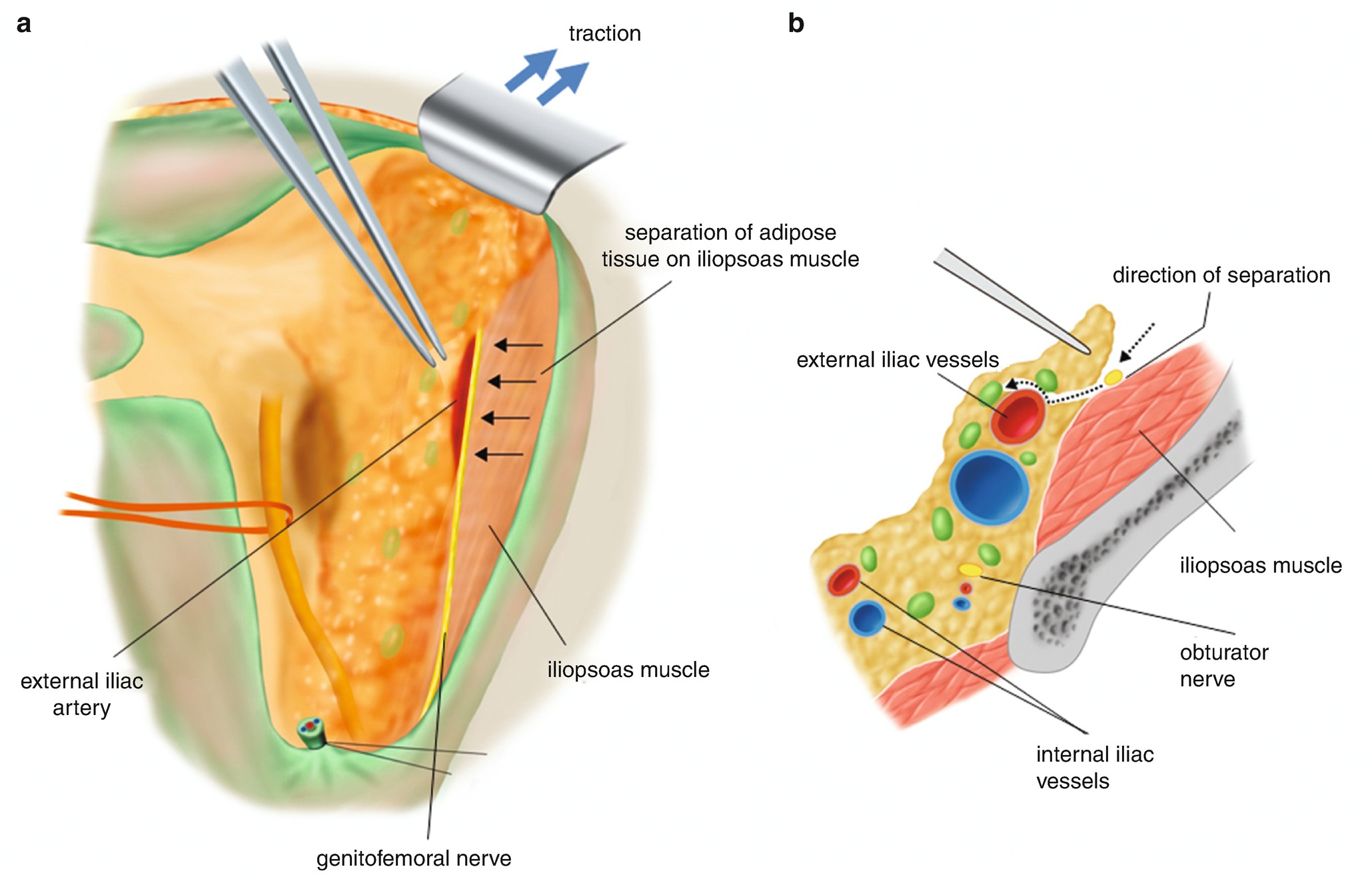
Exposure of the iliopsoas muscle. (a) Four small arrows on the iliopsoas muscle are indicating the direction of the separation of the adipose tissues toward the external iliac artery. (b) Two dotted arrow lines are showing direction of the separation of the adipose tissues toward the external iliac artery
6.2.4 Separation of the External Supra-Inguinal Nodes from the Ventral Surface of the External Iliac Artery (Figure 6.16)
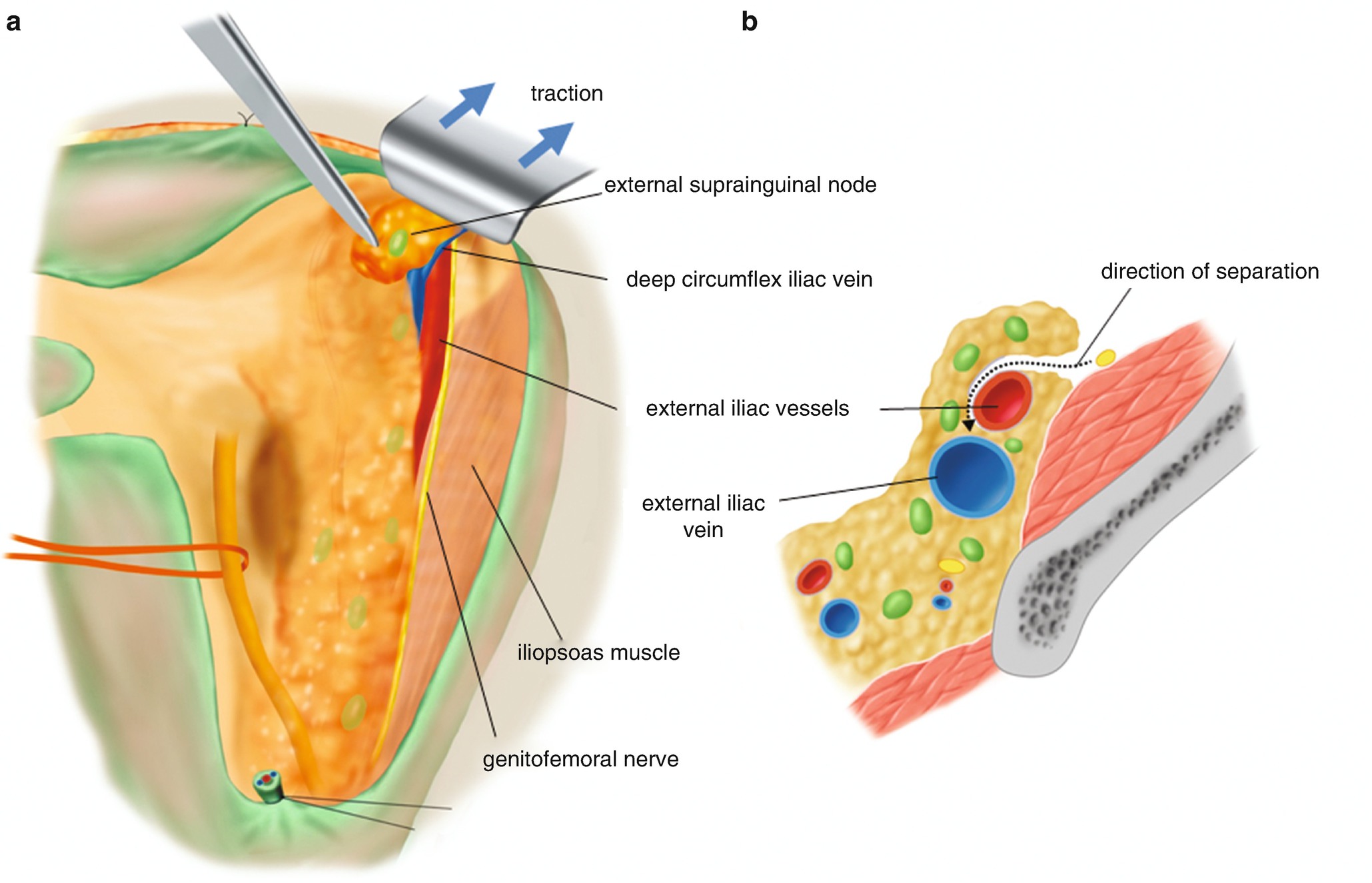
Separation of the external supra-inguinal nodes from the ventral surface of the external iliac artery. (a) By the traction of the abdominal wall of the supra-inguinal area distally (arrow), the adipose tissue including supra-inguinal nodes is separated from the ventral surface of the external iliac artery. (b) A dotted arrow line indicates the direction of separation of the adipose tissues that reaches to the ventral surface of the external iliac vein
6.2.5 Tentative Development of the Paravesical Space (Figure 6.17)
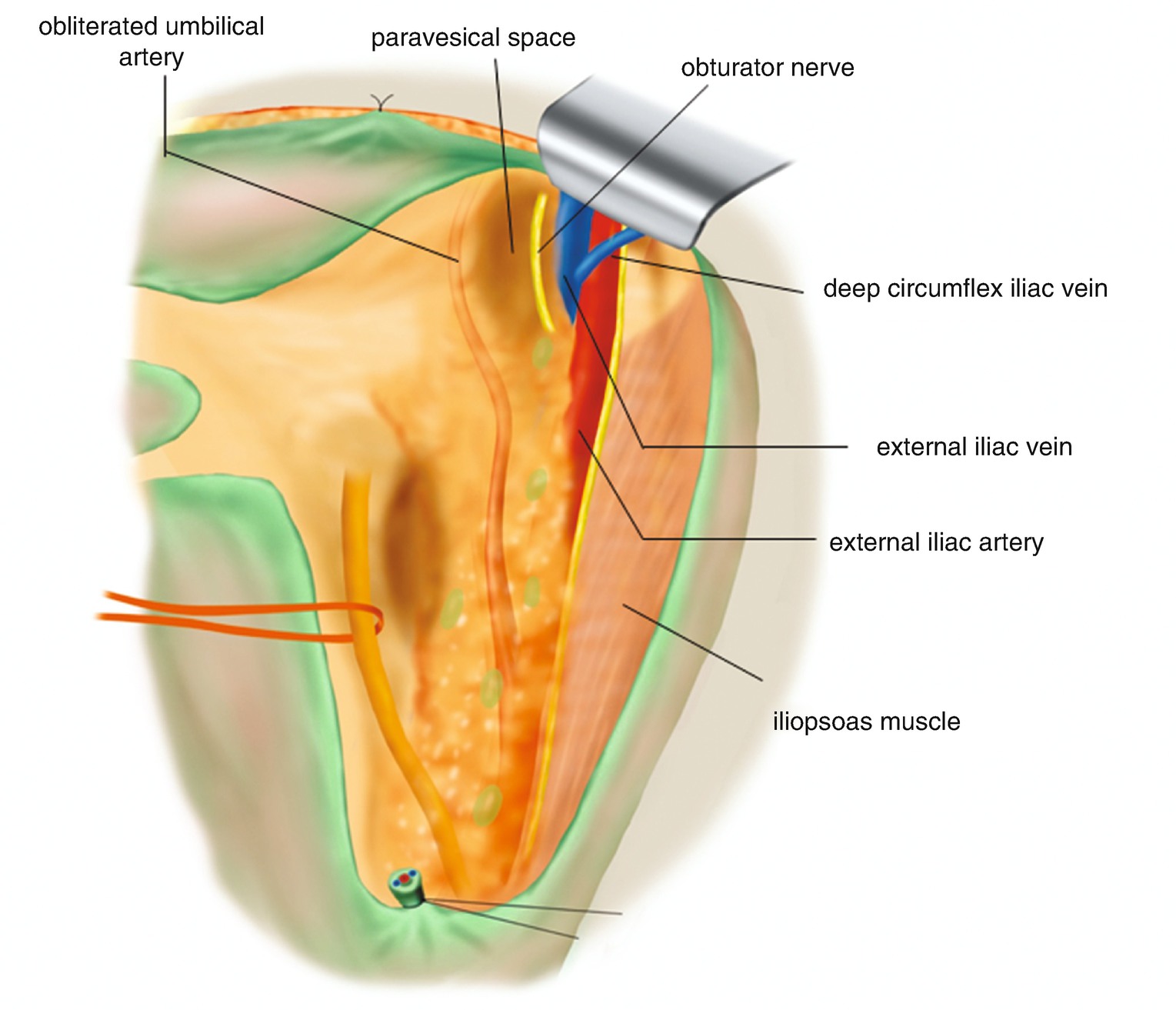
Tentative development of the paravesical space
6.2.6 Separation of the Connective Tissue Between the External Iliac Artery and Iliopsoas Muscle (Figure 6.18)
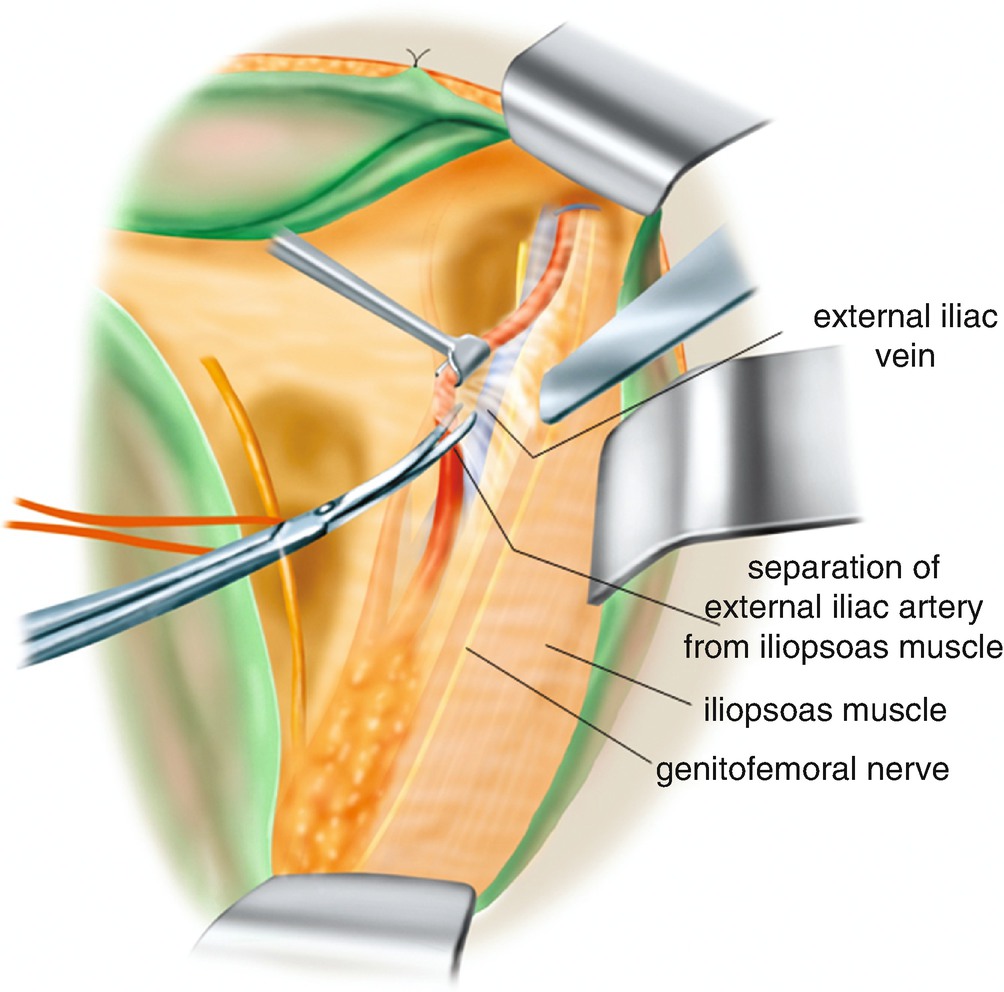
Separation of the connective tissue between the external iliac artery and iliopsoas muscle
6.2.7 Separation of the Uterine Side Connective Tissue of the External Iliac Artery and Vein (Figure 6.19)
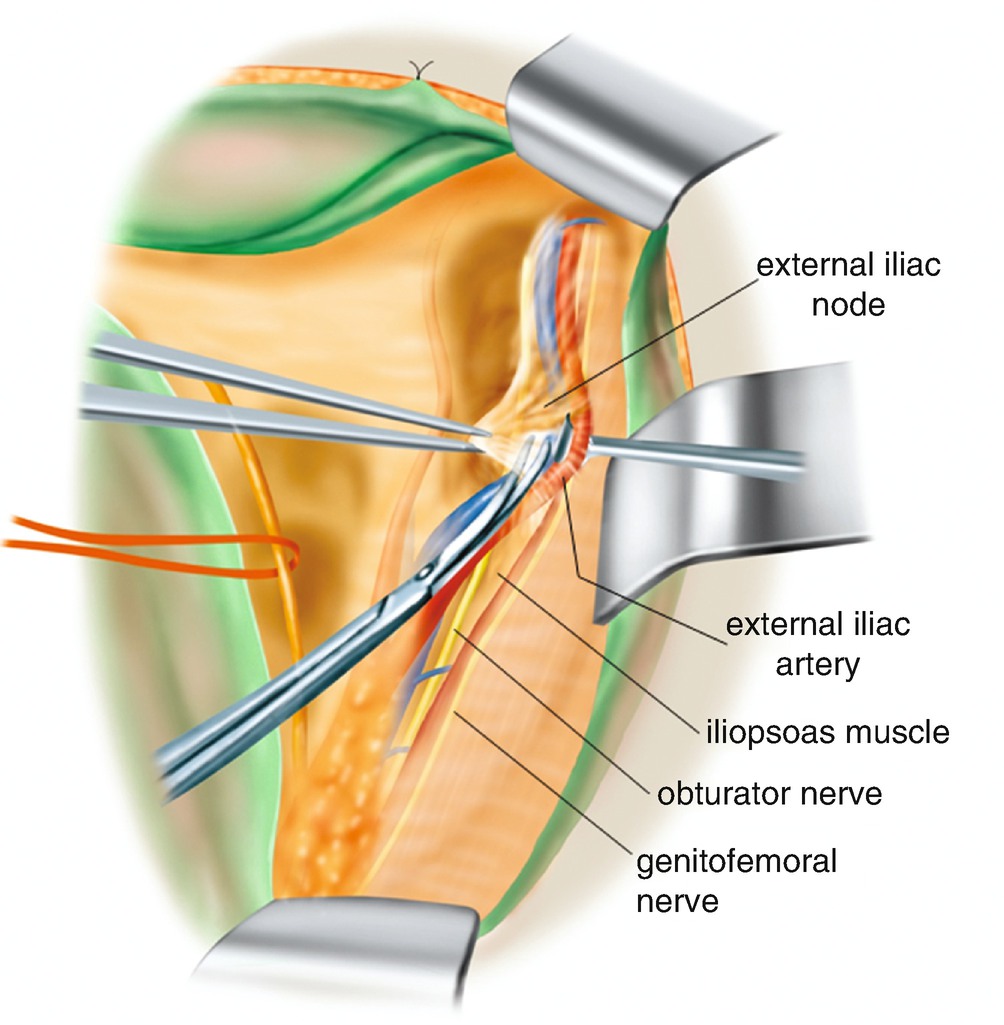
Separation of the uterine side connective tissue of the external iliac artery and vein
6.2.8 Lymphadenectomy of the External Iliac Nodes of the Uterine Side (Figure 6.20)
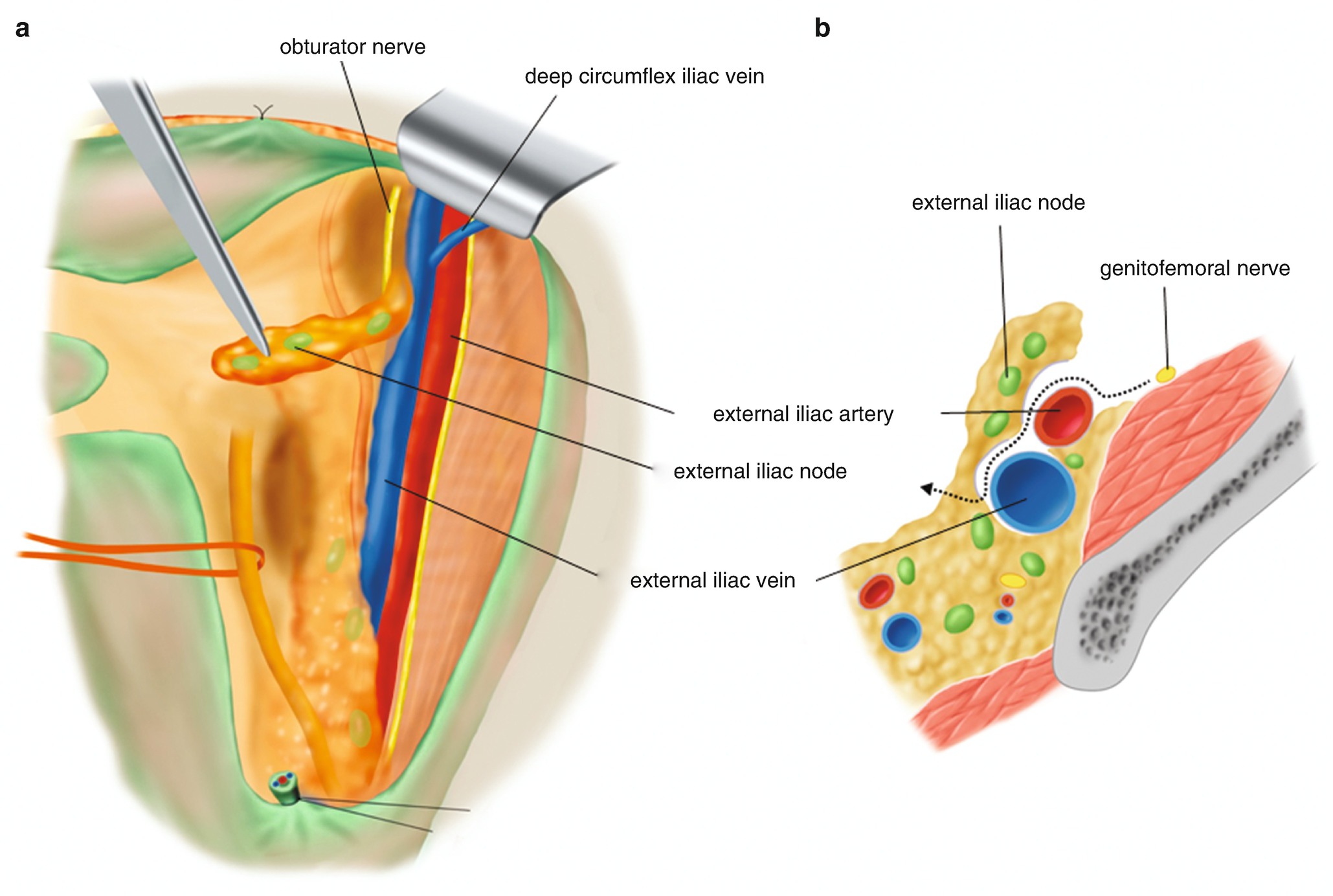
Lymphadenectomy of the external iliac nodes of the uterine side. (a) Picking up the adipose tissue on the medial side, the external iliac lymph nodes are dissected from the external iliac artery and vein. (b) A dotted arrow line is the direction of the separation
6.2.9 Separation of the Connective Tissue Between the Iliopsoas Muscle and the External Iliac Vessels Toward the Pelvic Floor (Figure 6.21)
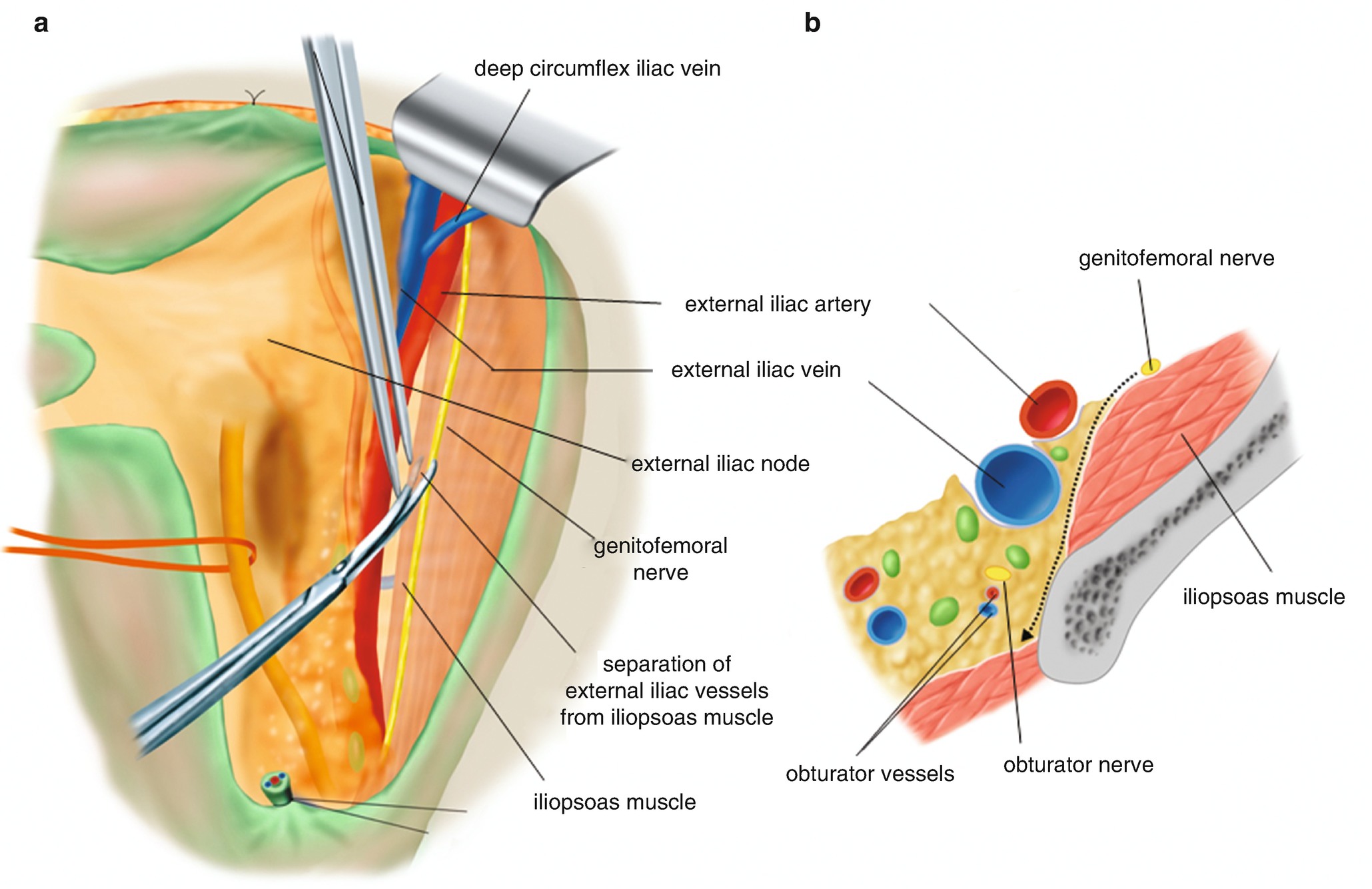
Separation of the connective tissue between the iliopsoas muscle and the external iliac vessels. (a) The connective tissue of the external iliac artery side is picked up and scissors are advanced into the connective tissue along the medial side of the iliopsoas muscle. (b) A dotted arrow line is the direction of the scissors dorsally into the obturator fossa deep enough to reach the base of the pelvic sidewall
6.2.10 Dissection of the External Iliac Nodes (Figure 6.22)
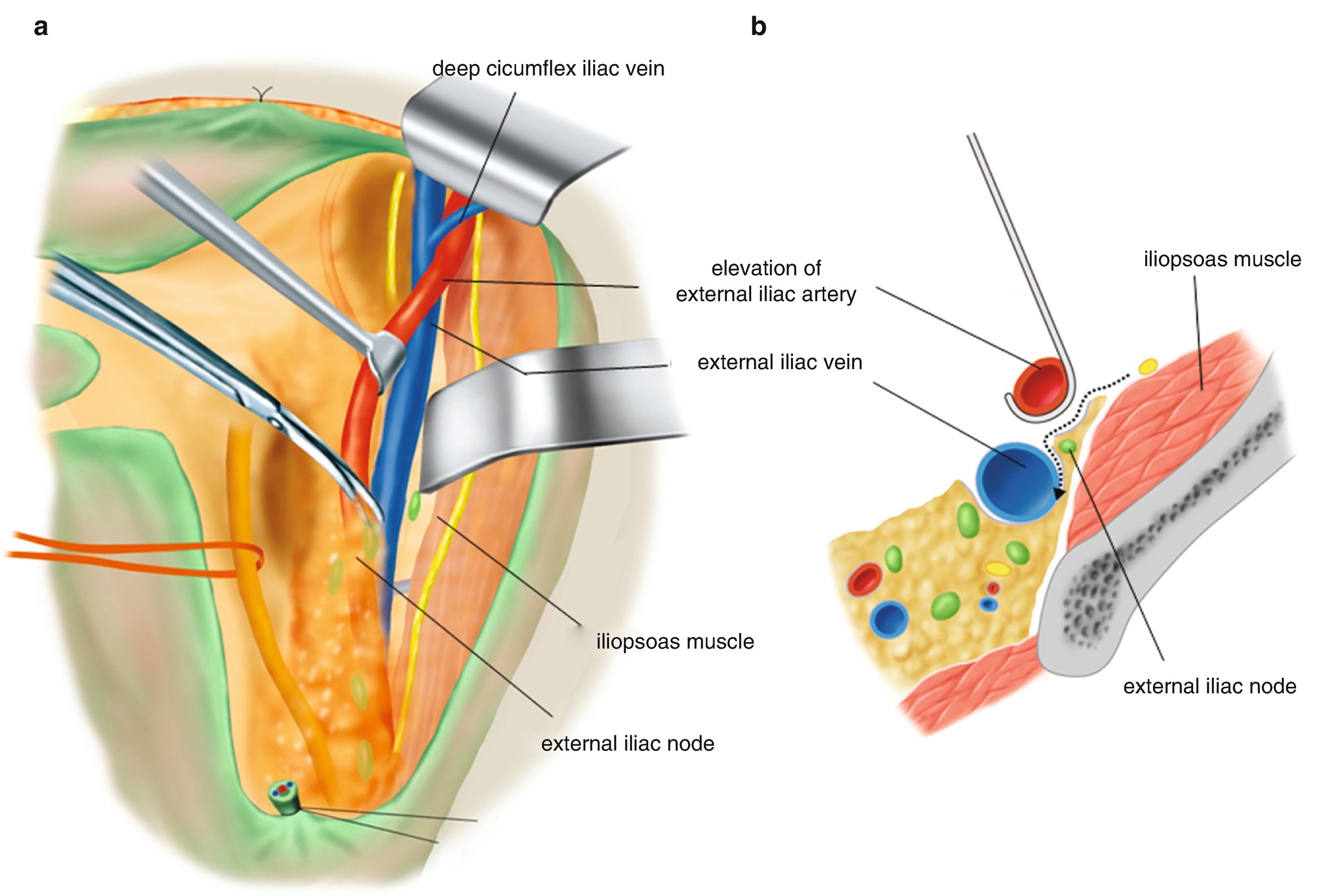
Dissection of the external iliac nodes. (a) Drawing the external iliac artery medially by a small retractor, the loose connective tissue sheath on the external iliac vein is separated toward the dorsal surface of the external iliac vein. (b) The connective tissue sheath with adipose tissue including the external iliac lymph nodes is separated from the external iliac vein as illustrated using a dotted arrow line
6.2.11 Separation of the Connective Tissue on the Internal Iliac Artery (Figure 6.23)
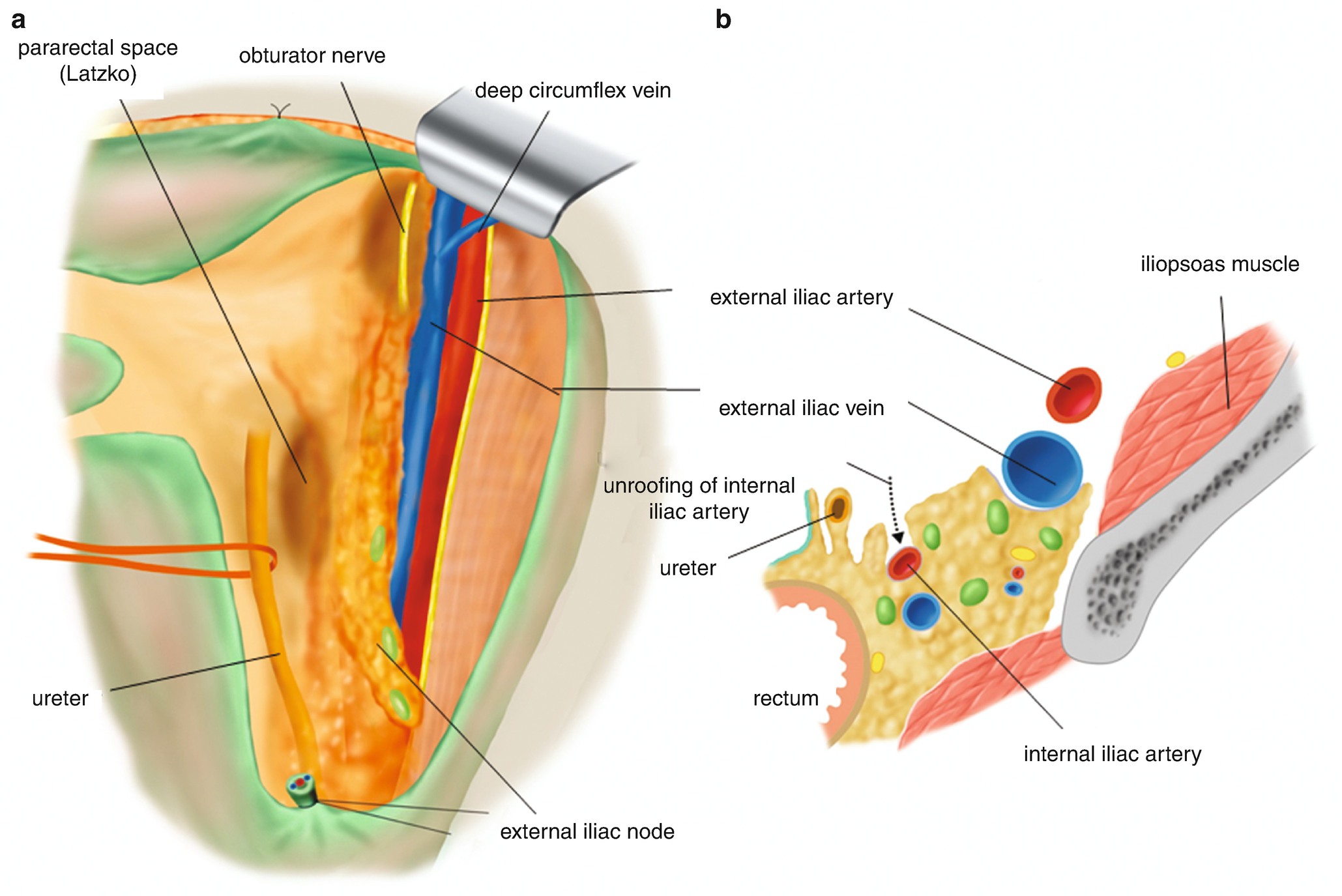
Separation of the connective tissue on the internal iliac artery. (a) The dissection is extended to both cranial side and caudal side of the external iliac vein. The adipose tissues with external iliac nodes are separated from the external iliac vein and are collected in the obturator fossa. (b) Once the internal iliac artery is found medially, the adipose and connective tissues are separated from the ventral side of the internal iliac artery as illustrated using a dotted arrow line
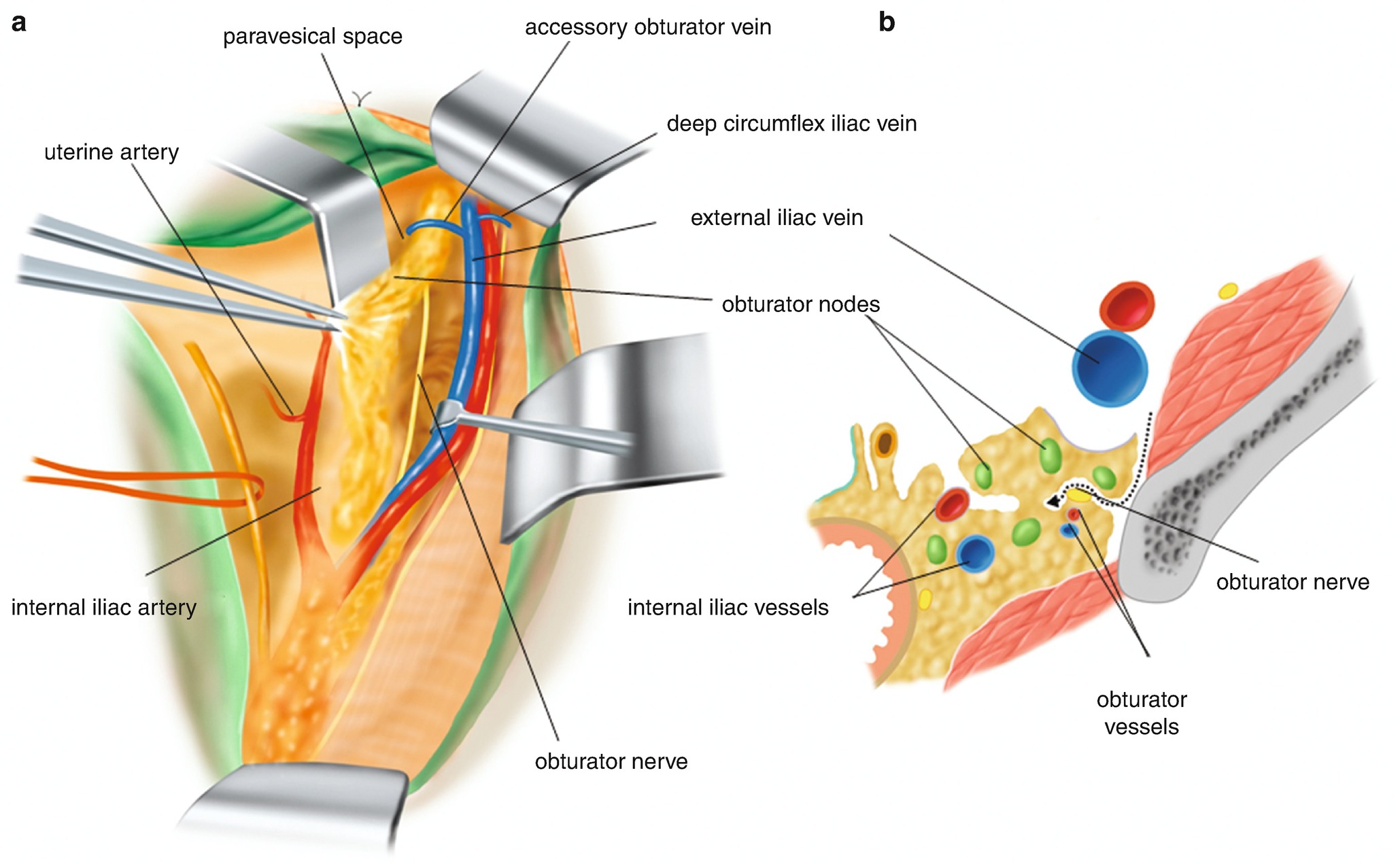
6.2.12 Confirmation of the Obturator Nerve in the Obturator Fossa (Figure 6.24)
Confirmation of the obturator nerve in the obturator fossa. (a) In the dorsal level of the external iliac vein, we usually appreciate a yellow-white solid string running in the obturator fossa. This is the obturator nerve. The obturator nerve becomes a landmark of the obturator fossa. (b) As illustrated using a dotted arrow line, the connective tissue with lymph nodes is separated toward the obturator nerve
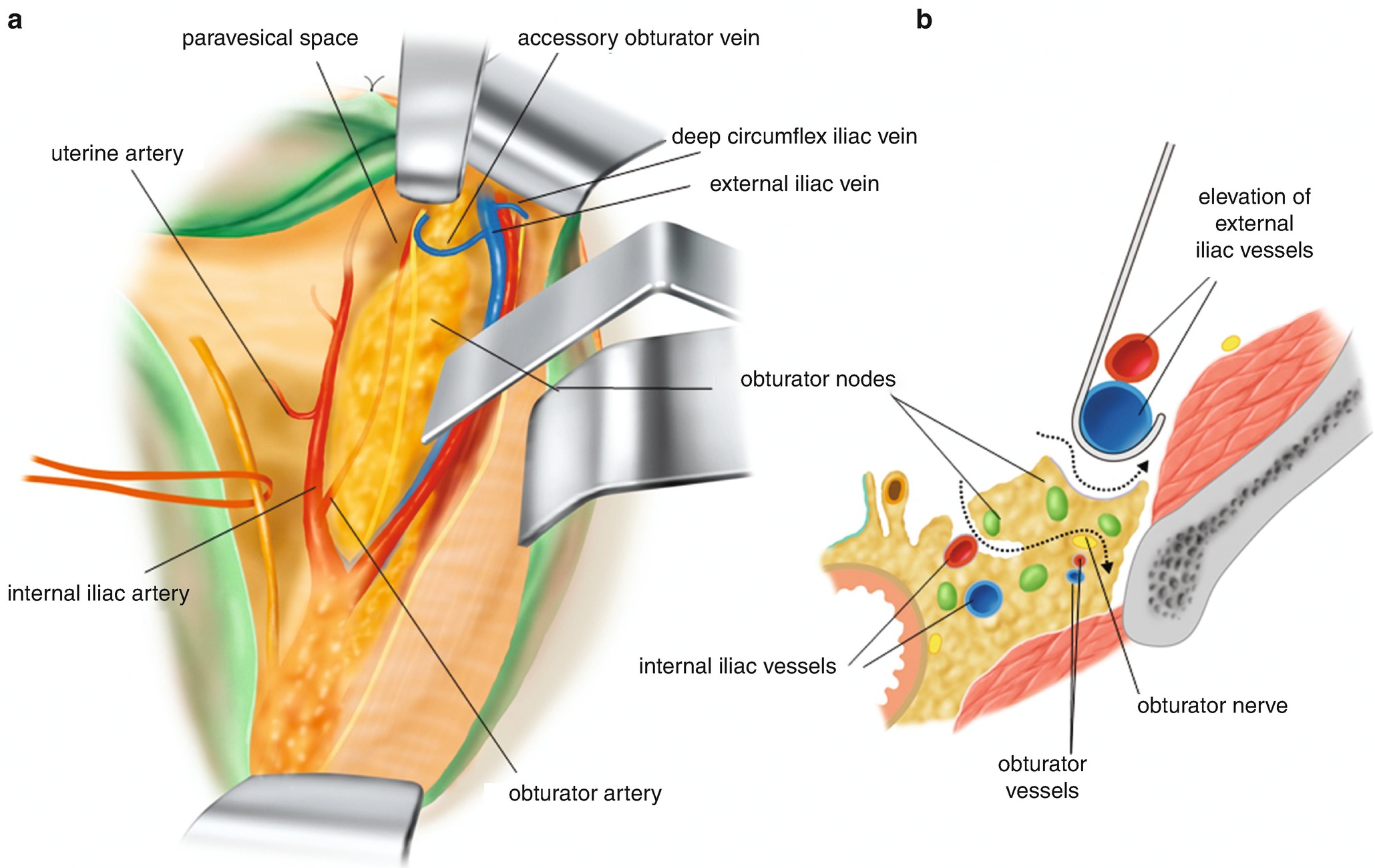
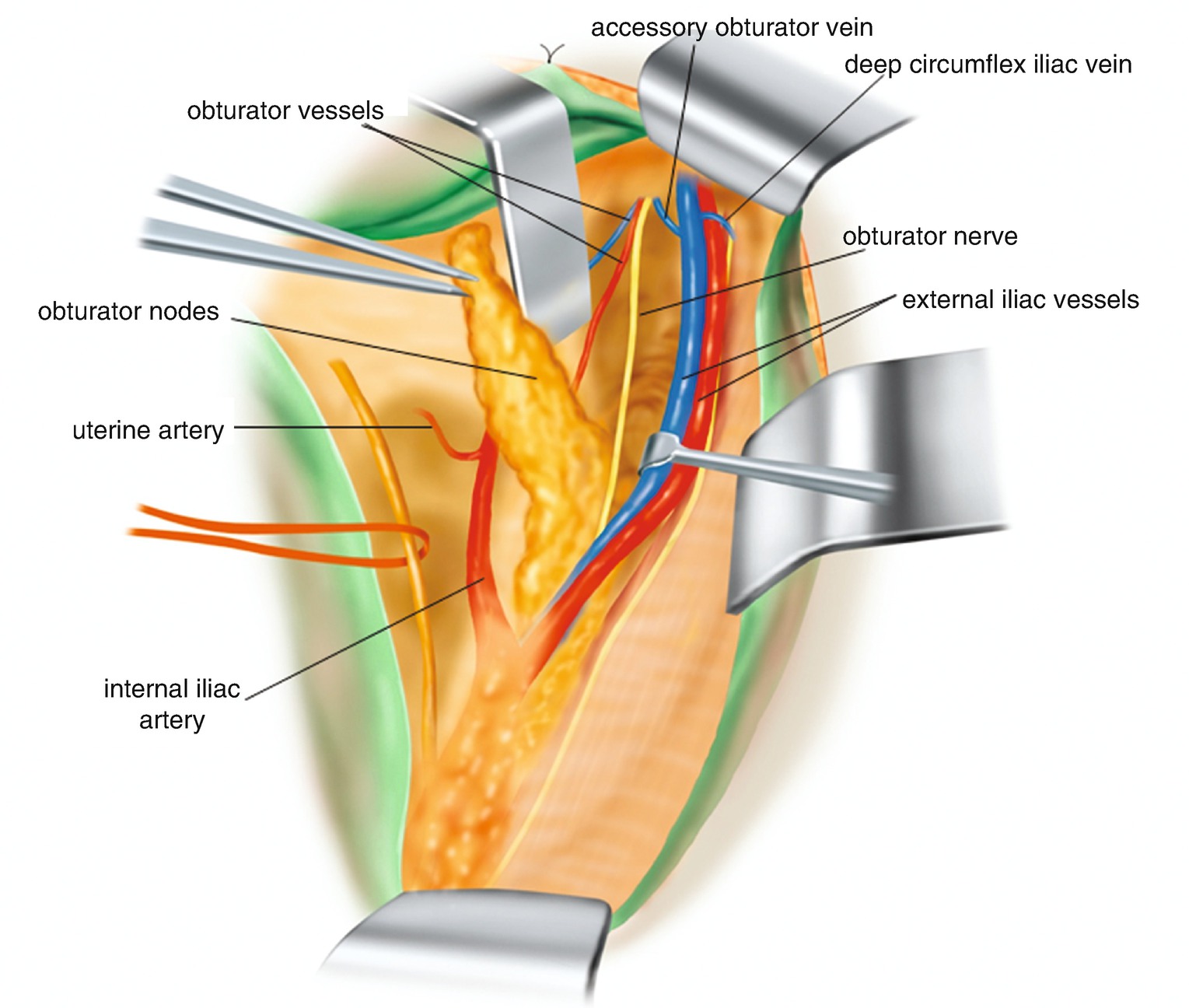
6.2.13 Lymphadenectomy of the Obturator Fossa [1] (Figure 6.25)
Lymphadenectomy of the obturator fossa. (a) Stripping of the adipose tissues surrounding the obturator nerve. (b) A dotted arrow is showing the separation line from the iliopsoas muscle side. The relationship between the obturator nerve and obturator vessels are also illustrated
6.2.14 Lymphadenectomy of the Obturator Fossa [2] (Figure 6.26)
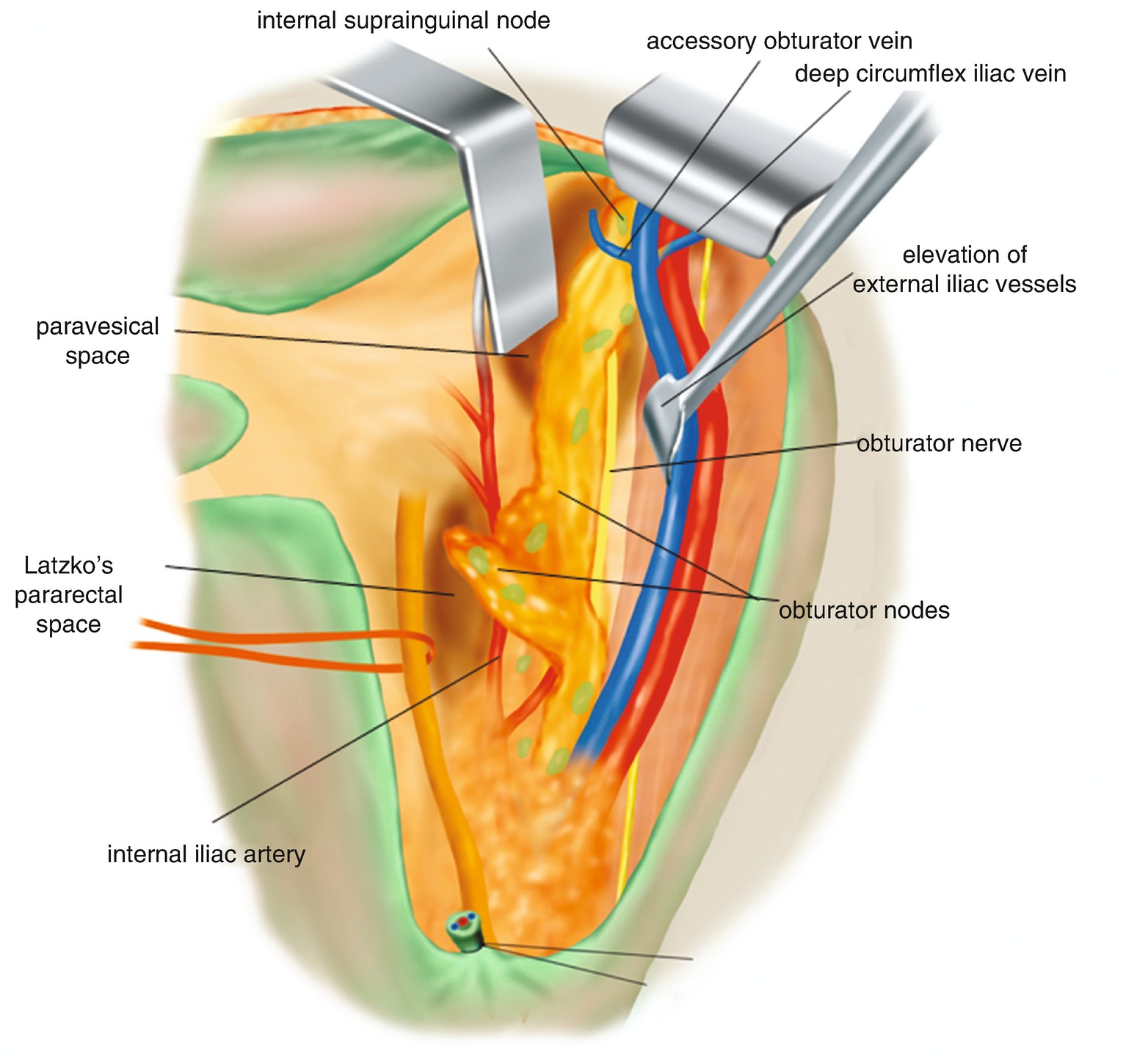
The internal supra-inguinal node is separated and passed to the dorsal side of the accessory obturator vein
6.2.15 Lymphadenectomy of the Obturator Fossa [3] (Figure 6.27)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


