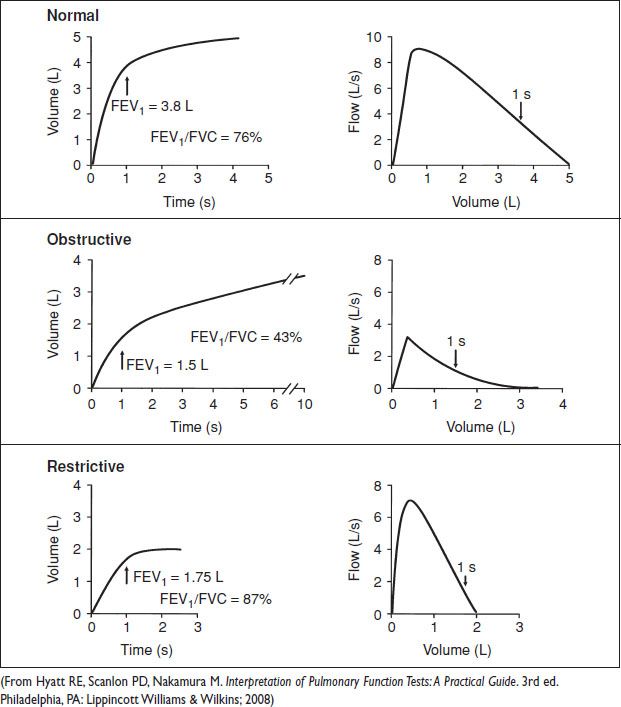
Spirometry (Am Fam Physician 2004;69(5):1107)
• Indicated for dx of pulm dz, follow-up of known dz, preoperative eval of pts w/ known pulm dz or prior to thoracic procedures
• Pt inhales maximally, then exhales w/ maximal effort as long as poss (at least 6 s). Contraindicated if Valsalva would be poorly tolerated. Time & vol vs. flow graphed. Rpt 3× for reliability/pt effort.
• FVC, FEV1, FEV1/FVC compare to % predicted values based on height/weight, age, sex, race
• Interpretation of spirometry: Ensure reliability & good pt effort (ie, valid study). If FVC, FEV1 nml & FEV1/FVC >70% → nml spirometry. If FVC nml or ↓, FEV1 ↓ & absolute FEV1/FVC <70% → obstructive physiology. If parameters correct after bronchodilator → reversible airway dz. If FVC ↓, FEV1 ↓ or nml & absolute FEV1/FVC >70% → restrictive physiology. Refer to pulm lab for lung volumes & DLCO.
• Obstructive diff dx: Asthma, chronic obstructive pulm dz (chronic bronchitis, emphysema)
• Restrictive diff dx: Intrinsic lung dz (acute pneumonitis, interstitial lung dz)
Extrinsic dz (mechanical abnormality of chest wall/pleura preventing expansion)
Neuromuscular d/o of respiratory muscles
Peak Flow Measurements
• Peak flow meter measures current PEFR; compare to personal best. Assesses relative obst & sx control. Does NOT establish dx – for surveillance only. Use in conjunction w/ asthma action plan.
• See http://www.perinatology.com/calculators/peakc.htm for expected peak flow calculator
Figure 13.2 Basic pulmonary function testing
RESPIRATORY CHANGES IN PREGNANCY
General (Clin Chest Med 2011;32:1)
• Upper airway: Mucosal hyperemia, edema, glandular hypersecretion. May contribute to disordered breathing in sleep from obst. ↑ Mallampati score, ↑ neck circumference. “Rhinitis of Preg” present during last 6 w of Preg, disappears postpartum in absence of allergy or other pulm pathology.
• Chest wall: Compliance decreased. Widened subcostal angle, increased anteroposterior dimension mediated hormonally by relaxin. Changes peak at 37 w. Diaphragmatic excursion increased. Max inspiration/expiration pressures same as prior to Preg.
Lung Function
• Minute ventilation ↑ 20–50% by term (most ↑ during 1st trimester). ↑ progesterone & ↑ CO2 production (VCO2) ↑ central stimuli for hyperventilation. Physiologic dyspnea of Preg may be awareness of ↑ stimulus to breathe. VT ↑.
• Oxygen consump (VO2) is increased; respiratory exchange rate (VCO2/VO2) unchanged vs. minimally increased
• FRC ↓ by diaphragm elevation, ↓ chest wall recoil, ↓ abd pull. (Note: Obesity → ↓ FRC & ↑ RV [air trapping]. In Preg, ↓ FRC w/ ↓ RV.) Airway resistance unchanged.
• (IC; IRV + VT) increases 5–10%. TLC is unchanged or ↓ minimally at term.
• FEV1, FEV1/FVC, flow/vol curve not significantly changed. Abn spirometry sugg pathology.
• DLCO no change. Increased cardiac outpt offset by decreased Hgb.
Intrapartum/Postpartum Changes
• Hyperventilation ↑ w/ pain/anxiety. Analgesia mitigates this. Minute ventilation varies widely.
• Hypocarbia can cause placental vasoconstriction → hypoperfusion
• Postpartum, all above changes resolve, except for widened subcostal angle.
ARTERIAL BLOOD GAS (ABG) ANALYSIS
Procedure
• Sterilely prep area overlying radial, femoral, brachial, dorsalis pedis, or axillary artery
• Consider local anesthesia over puncture site. Assess for collateral circulation.
• Obtain 2–3 mL bld in heparinized syringe. Remove air bubbles, place on ice for transport.
• Consider indwelling arterial catheter for serial ABGs.
Considerations in Pregnancy (Clin Chest Med 2011;32(1))
• ↓ pCO2 from hyperventilation. ↓ serum bicarb compens for chronic respiratory alkalosis. ↑ pH (7.42–7.46).
• Chronic alkalosis stimulates ↑ 2,3-DPG w/ shift of Hgb dissociation curve; aids in placental O2 exchange. ↑ pO2 facilitates placental O2 exchange. PO2 significantly lower supine vs. sitting. High metabolic rate can cause rapid desaturation if apneic.
Definitions
• Acidemia: Arterial pH lower than nml (<7.35)
• Alkalemia: Arterial pH higher than nml (>7.45)
• Metabolic acidosis: Process that decreases serum HCO3 → ↓ pH (bicarb consump)
• Respiratory acidosis: Process that increases serum pCO2 → ↓ pH (hypoventilation)
• Metabolic alkalosis: Process that increases serum HCO3 → ↑ pH (bicarb excess)
• Respiratory alkalosis: Process that decreases serum pCO2 → ↑ pH (hyperventilation)
Normal Values
• Nonpregnant: pH, 7.35–7.45; pCO2, 32–45 mmHg; pO2, 72–104 mmHg; HCO3, 22–30 mEq/L
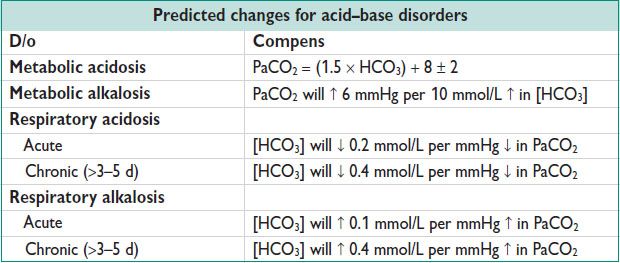
Diagnosis (Harrison’s Principles of Internal Medicine, 18th ed)
• Obtain ABG & electrolytes simultaneously. Use HCO3 from electrolytes.
• Determine whether simple or mixed d/o by assessing whether expected compensatory resp is present. “Compens” cannot change alkalemia to acidemia or vice versa. If apparent insuff or overexuberant compens, mixed d/o likely exists.
• If acidosis present, calculate AG: (Na − [Cl + HCO3]) w/ adjustment for albumin (nml AG ≈ 2.5 × albumin)
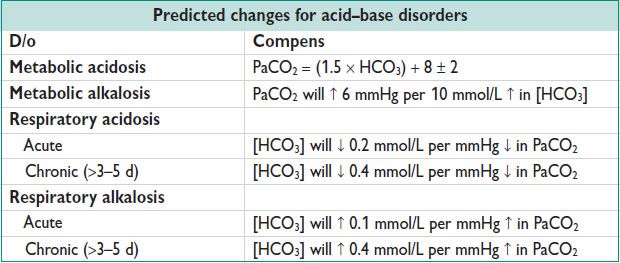
• Consider ΔAG/ΔHCO3 ratio to determine if simple high AG metabolic acidosis (ratio btw 1 & 2). If ratio >2, likely additional metabolic alkalosis. If <1, likely additional nongap metabolic acidosis.
• Ddx guides clinical assessment & final dx:
For high AG metabolic acidosis: Renal failure, lactic acidosis, toxins, ketoacidosis. W/o high AG: Renal tubular acidosis, GI loss.
For metabolic alkalosis: Exogenous alkali, extracellular fluid contraction w/ hypoK, extracellular fluid expansion w/ hypoK/Mineralocort excess
For respiratory acidosis: Hypoventilation (obst, CNS depression, neuromuscular d/o, impaired gas exchange)
For respiratory alkalosis: Hyperventilation (secondary to hypoxia, Preg, pain, sepsis, drugs)
PNEUMONIA
Definitions (Am J Respir Crit Care Med 2005;171:388; Clin Infect Dis 2007;44 Suppl 2:S27)
• CAP: PNA Acq as outpt; no risk factors for HCAP
• HAP: PNA developing >48 h after admission, not incubating at time of admission
• VAP: PNA developing >48–72 h after intubation
• HCAP: PNA in pt w/ any 1 of the following:
Hospitalized >2 d in last 90 d
Resides in long-term care facility
Received IV Abx, chemo, wound care w/i last 30 d
Attended hospital or hemodialysis clinic in last 30 d
• Risk factors for MDR infxn: Any of the HCAP factors above
High prevalence of MDR pathogens in community or inpt unit; chronic heart, lung, liver, renal dz; functional or surgical asplenia; malig; immunocompromise or immunosuppression; recent use of Abx (PO or IV) w/i last 90 d
Diagnosis
• Signs & sx: Cough, dyspnea, pleuritic chest pain, sputum production (fewer reported by elderly); tachypnea, fever, decreased oxygen sat, abn lung exam. Imaging: New lung infiltrate on XR or CT
• Microbiology: Consider induced sputum, influenza assays, urine strep or legionella assays; bld cx if febrile (& prior to Abx); bronchoscopy/washings. Limited sens for cx; consider diff (include pt factors for uncommon causes) & often treat empirically.
• Multi decision tools to assess severity of dz on presentation; PSI may be most rigorous (N Engl J Med 1997;336(4):243). Calculator available at http://pda.ahrq.gov/clinic/psi/psicalc.asp.

Treatment: Antibiotic Selection
• For outpt rx of CAP w/o risk factors for MDR
Macrolide (erythro-/clarithro-/Azithro)
• For outpt rx of CAP w/ risk factors for MDR or for inpt CAP
Respiratory quinolone (moxi-/gemi-/Levo) OR β-lactam plus macrolide
• For HAP, early onset, w/o risk factors for MDR
Ceftriaxone OR levo-/moxi-/ciprofloxacin OR ampicillin/sulbactam OR ertapenem
• For HCAP/VAP/HAP, late onset w/ risk factors for MDR
Antipseudomonal cephalosporin (cefepime/ceftazidime) or carbapenem (imipenem/meropenem) or piperacillin/tazobactam &
Antipseudomonal fluoroquinolone (cipro-/Levo) or aminoglycoside (amikacin/gentamicin/tobramycin) &
Linezolid or Vanco for MRSA coverage
If Legionella is suspected, add macrolide or use quinolone instead of aminoglycoside
• For aspiration w/ concern for bact infxn
Clindamycin (preferred), ampicillin/sulbactam or imipenem; may use metronidazole if added on to an MDR regimen above. Consider d/c Abx if no infiltrate 48–72 h after aspiration event.
Treatment: Duration
• In outpts, 5 d w/ or w/o MDR risk factors; may dose Azithro × 3 d b/c of long half-life
• In inpts, reassess clinical status after 2–3 d of rx
If improved & neg cx, consider d/c Abx or continue for 7–8 d w/o pseudomonal/MRSA coverage. If cx +, tailor Abx & consider rx for 7–8 d (15 d if Pseudomonas, 21 d if S. aureus).
If no improv, consider broadening/adjusting Abx, search for alt infxn, dx, or pathogens
• Suspected PNA in Preg is rarely treated outpt given increased morbidity & mortality. Low threshold for inpt rx.
Prevention
• Avoid intubation & reintubation. Ensure ventilator circuit is well maintained.
• If risk for aspiration, keep head of bed >30 deg
• Enteral feeding preferred to parenteral feeding to ↓ risk of bact translocation from gut
• Minimize time w/ NGT in place to ↓ risk of nosocomial sinusitis
• Formal eval & diet changes for pts w/ difficulty speaking/swallowing
• Postoperatively, consider incentive spirometry, optimize pain control, avoid routine NGT.
• Pneumococcal vax if >65 yo or w/ high-risk medical illness. Splenectomy vax if indicated. Flu vax for all pts.
PULMONARY EDEMA
Definition/Diagnosis
• Inappropriate accum of fluid in pulm interstitium & alveoli
• Sx: Dyspnea, orthopnea. Signs: Tachypnea, desaturation, rales, rhonchi, wheezes, respiratory failure, S3 gallop. Imaging: Peribronchial thickening, prominent vascular markings, Kerley B lines, alveolar infiltrates.
Etiology
• Fluid accum/retention OR redistribution into tissues from vasoconstriction/dilation
• Cardiogenic: Left ventricular dysfxn → elevated hydrostatic pres in pulm veins, extravasation of fluid into lung tissue
• Noncardiogenic: Direct lung injury (chest trauma, aspiration, PNA, oxygen tox, smoke inhalation, reperfusion post PE); hematogenous lung injury (sepsis, pancreatitis, xfusion, IV drug use); elevated hydrostatic pressures (re-expansion, high altitude, neurogenic)
Treatment
• Target cause (eg, cardiogenic vs. noncardiogenic). Consider echocardiogram to diagnose new/worsening cardiac fxn. Initial measures: Supplemental oxygen, positive pres ventilation. ↓ preload w/ loop diuretics (furosemide), consider nitrates, morphine, ACEI (not in Preg), pt should be upright in bed if poss. Consider transition to intensive care.
Considerations in Pregnancy (Anaesthesia 2012;67:646)
• Increased incid 0.08–0.5%. Rapid appearance of flash pulm edema.
• Risk factors in Preg: Preeclampsia, preterm labor, sepsis, AFE, PE, β-adrenergic tocolytics, magnesium sulfate, corticosteroids, positive fluid balance, multifetal gest
INFLUENZA IN PREGNANCY
Vaccination and Prevention
• Pregnant women are at ↑ risk for sev infxn & death than the general pop (Obstet Gynecol 2010;116:1006)
• ACOG & the CDC’s Advisory Committee on Immunization Practices recommend that all pregnant women be vaccinated against influenza, regardless of trimester (MMWR 2010;59(rr08)) mat/fetal safety of influenza vaccination in Preg is well established (Am J Obstet Gynecol 2012;207(3 Suppl)). Antepartum vaccination → decreased stillbirth, neonat death & premature deliv, w/ no ↑ in congen anomalies (Obstet Gynecol 2012;120:532).
• Mat vaccination provides passive immunity to the neonate through 6 mo of age (N Engl J Med 2008;359(15):1555). Pregnant women should receive the trivalent inactivated (killed) injection vaccine only, & not the LAIV; FluMist.
• Pregnant/postpartum women do not need to avoid contact w/ those who have received LAIV. Postpartum/breastfeeding women can receive LAIV.
• Data do not support adverse effects attributable to preservative thimerosal (MMWR 2010;59(rr08)). Preservative eliminated or reduced in most preparations. Proven protection against serious dz outweighs theoretical concerns regarding preservative.
Prophylaxis and Treatment (MMWR 2011;60(1):1)
• Clinical dx is preferred (abrupt onset fever, cough, myalgia) to lab dx for rapid rx
• Oseltamivir & zanamivir are both Preg Category C. Zanamivir may be preferable in Preg b/c of limited systemic Absorp, but avoid in pts w/ comorbid respiratory dz. Most effective if ≤48 h of sx (Obstet Gynecol 2010;115(4):717).
• For ppx after exposure during Preg or up to 2 w postpartum:
Zanamivir 10 mg (2 puffs inhaled) daily
Oseltamivir 75 mg PO daily
Duration: 10 d (household exposure), 14 d (hospital exposure), 7 d (other)
• For rx w/ onset of sx
Zanamivir 10 mg (2 puffs inhaled) daily × 5 d
Oseltamivir 75 mg PO twice daily × 5 d
Can consider longer rx for severely ill pts
Additional Considerations
• Women w/ influenza hospitalized on labor & deliv wards should have respiratory precautions per hospital std for influenza
• Discuss the need for neonat antivirals or mat–neonat separation w/ pediatricians
• Postpartum, women w/ influenza should express breast milk, rather than breastfeed. Milk may still go to the infant, as oseltamivir is poorly excreted (Int J Infect Dis 2008;12:451).
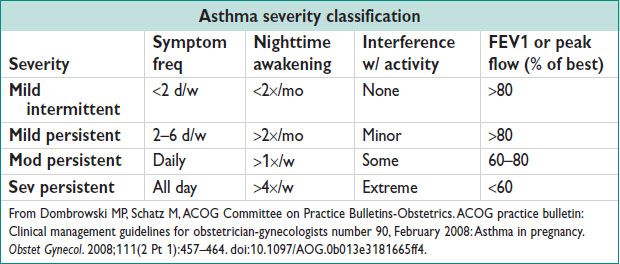
ASTHMA AND PREGNANCY
(Obstet Gynecol 2008;111:457; NIH pub no. 08-4051)
Definitions/Pathophysiology
• Chronic airway inflammation w/ hyperresponsiveness to various stimuli & partially reversible airway obst
• Sev cases a/w increased prematurity, cesarean deliv, preeclampsia, growth restriction, & mat morbidity/mortality
• Mat–fetal pathology caused by mat hypoxia. Decreased FEV1 → ↑ low birth weight/prematurity.
Diagnosis
• Wheeze, cough, SOB, chest tightness; fluctuating; often worse at night; worse w/ known triggers (allergens, exercise, infections). Consider GERD, postnasal drip w/ cough, bronchitis in diff
• Airway obst on spirometry, reversible w/ bronchodilator therapy
• Document h/o hospitalization, ICU stay, intubation, & steroid rx. Preg may improve, worsen or have no effect on asthma severity (rule of 1⁄³’s). Past pregnancies may better predict course of subseq pregnancies.
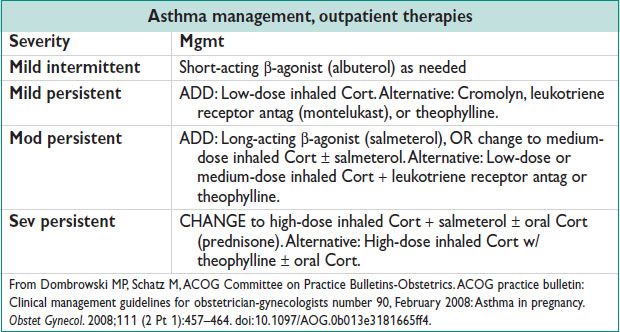
Treatment
• Rx for acute asthma exacerbation
Supplemental O2 to maintain sat >95% (important for fetal oxygenation)
Albuterol nebulizer q20min × 3, then q4h
Consider inhaled ipratropium on presentation (0.5 mg neb/8 puffs MDI)
Systemic corticosteroids; prednisone 40–80 mg PO × 5–10 d (until PEFR >70%)
• Triage for acute presentation of asthma in Preg
FEV1 or PEFR >70% after rx, no distress, reassuring fetal status → discharge
FEV1 or PEFR 50–70% after rx → individualize disposition
FEV1 or PEFR <50% after rx → hospitalize
If poor resp/sev sx, drowsiness, confusion, pCO2 >40 mmHg consider ICU admission ± intubation
Arrange follow-up w/i 5 d postdischarge
Surveillance During Pregnancy
• Assess asthma status w/ PEFR at each prenatal visit; adjust maint regimen
• Prepare Asthma Action Plan & instruct on use. Eg, www.nhlbi.nih.gov/health/public/lung/asthma/asthma_actplan.pdf.
• Focus on avoidance of allergens/irritants (eg, tobacco smoke, GERD, mold, dust mites, dander, cockroaches)
• Albuterol & budesonide are preferred short-acting β-agonist/inhaled steroid in Preg. Consider weekly fetal testing (NST, AFI, or BPP) from 32–34 w if mod–sev asthma or poor control.
Intrapartum Considerations
• Maintain hydration, continue asthma meds, including systemic steroids
• Consider cesarean deliv if unstable asthma & mature fetus
• Avoid carboprost tromethamine (Hemabate)
• ASA, indocin, other NSAIDs can cause asthmatic bronchospasm
• No contraindication to breastfeeding postpartum for asthma meds above
ANAPHYLAXIS
Definition and Diagnosis
(J Allergy Clin Immunol 2006;117(2):391)
• Sev, potentially fatal, systemic allergic (IgE mediated) rxn, occurring suddenly after exposure to an allergen. Dx requires 1 of the following:
Acute onset w/ involvement of the skin, mucosae, or both & compromise of respiratory, CV, or other end-organ fxn;
Acute onset of compromise of fxn of at least 2 organ systems (skin, GI, respiratory, CV) after exposure to likely allergen;
HoTN after exposure to known allergen.
• Skin sx present in ≥80% of cases. Consider total tryptase level (drawn when pt symptomatic) to confirm dx.
Treatment
• Removal of potential allergen(s). Mobilize resources (EMS, ICU, or Code team)
• Prompt dosing of 0.3–0.5 mg (at 1:1000 dilution) epi intramuscularly. May rpt q5–15min.
• Position supine, apply oxygen, monit vital signs, obtain IV access w/ crystalloid support as needed. Consider albuterol, H2/H1 blockers, methylprednisolone (1–2 mg/kg q6h). Consider glucagon if refrac sx in pt on β-blocker.
• Consider observation for biphasic rxn (recurrence of sx w/i 72 h in 1–20% of cases)
• Ensure appropriate follow-up w/ allergist; discharge w/ >1 epi autoinjector if appropriate
Considerations in Obstetric and Gynecologic Populations
• Sx & rx in Preg are generally the same as for nonpregnant women. Consider AFE (bronchospasm more likely w/ anaphylaxis, coagulopathy more likely w/ AFE), or preeclampsia-related airway/subcutaneous edema depending on clinical setting. Breastfeeding reported as a rare cause of anaphylaxis (Obstet Gynecol 2009;114(2 Pt 2):415).
• Monit fetal cardiac activity continuously, w/ deliv for persistent category III tracings despite aggressive mat intervention. Consider hospital exposures when anaphylaxis is diagnosed inpt (latex, perioperative Abx, oxytocin, laminaria, chemotherapeutic agents).
< div class='tao-gold-member'>



