Puerperal Fever
A number of factors can cause fever—a temperature of 38.0°C (100.4°F) or higher—in the puerperium. Most persistent fevers after childbirth are caused by genital tract infection. Using this conservative definition of fever, Filker and Monif (1979) reported that only about 20 percent of women febrile within the first 24 hours after giving birth vaginally were subsequently diagnosed with pelvic infection. This was in contrast to 70 percent of those undergoing cesarean delivery. It must be emphasized that spiking fevers of 39°C or higher that develop within the first 24 hours postpartum may be associated with virulent pelvic infection caused by group A streptococcus and is discussed on page 683.
Other causes of puerperal fever include breast engorgement, urinary infections, episiotomy and abdominal incisions, perineal lacerations, and respiratory complications after cesarean delivery (Maharaj, 2007). Approximately 15 percent of women who do not breast feed develop postpartum fever from breast engorgement. As discussed in Chapter 36 (p. 675), the incidence of fever is lower in breast-feeding women. “Breast fever” rarely exceeds 39°C in the first few postpartum days and usually lasts < 24 hours. Urinary infections are uncommon postpartum because of the normal diuresis encountered then. That said, acute pyelonephritis has a variable clinical picture. The first sign of renal infection may be fever, followed later by costovertebral angle tenderness, nausea, and vomiting. Atelectasis following abdominal delivery is caused by hypoventilation and is best prevented by coughing and deep breathing on a fixed schedule following surgery. Fever associated with atelectasis is thought to follow infection by normal flora that proliferate distal to obstructing mucus plugs.
 Uterine Infection
Uterine Infection
Postpartum uterine infection or puerperal sepsis has been called variously endometritis, endomyometritis, and endoparametritis. Because infection involves not only the decidua but also the myometrium and parametrial tissues, we prefer the inclusive term metritis with pelvic cellulitis.
Predisposing Factors
The route of delivery is the single most significant risk factor for the development of uterine infection (Burrows, 2004; Conroy, 2012; Koroukian, 2004). In the French Confidential Enquiry on Maternal Deaths, Deneux-Tharaux and coworkers (2006) cited a nearly 25-fold increased infection-related mortality rate with cesarean versus vaginal delivery. Rehospitalization rates for wound complications and endometritis were increased significantly in women undergoing a planned primary cesarean delivery compared with those having a planned vaginal birth (Declercq, 2007).
Vaginal Delivery. Compared with cesarean delivery, metritis following vaginal delivery is relatively infrequent. Women delivered vaginally at Parkland Hospital have a 1- to 2-percent incidence of metritis. Women at high risk for infection because of membrane rupture, prolonged labor, and multiple cervical examinations have a 5-to 6-percent frequency of metritis after vaginal delivery. If there is intrapartum chorioamnionitis, the risk of persistent uterine infection increases to 13 percent (Maberry, 1991). Finally, in one study, manual removal of the placenta, discussed in Chapter 41 (p. 784), increased the puerperal metritis rate threefold (Baksu, 2005).
Cesarean Delivery. Single-dose perioperative antimicrobial prophylaxis is recommended for all women undergoing cesarean delivery (American College of Obstetricians and Gynecologists, 2011). Such single-dose antimicrobial prophylaxis has done more to decrease the incidence and severity of postcesarean delivery infections than any other intervention in the past 30 years. Such practices decrease the puerperal pelvic infection risk by 65 to 75 percent (Smaill, 2010).
The magnitude of the risk is exemplified from reports that predate antimicrobial prophylaxis. Cunningham and associates (1978) described an overall incidence of 50 percent in women undergoing cesarean delivery at Parkland Hospital. Important risk factors for infection following surgery included prolonged labor, membrane rupture, multiple cervical examinations, and internal fetal monitoring. Women with all these factors who were not given perioperative prophylaxis had a 90-percent serious postcesarean delivery pelvic infection rate (DePalma, 1982).
Other Risk Factors. It is generally accepted that pelvic infection is more frequent in women of lower socioeconomic status (Maharaj, 2007). Except in extreme cases usually not seen in this country, it is unlikely that anemia or poor nutrition predispose to infection. Bacterial colonization of the lower genital tract with certain microorganisms—for example, group B streptococcus, Chlamydia trachomatis, Mycoplasma hominis, Ureaplasma urealyticum, and Gardnerella vaginalis—has been associated with an increased postpartum infection risk (Andrews, 1995; Jacobsson, 2002; Watts, 1990). Other factors associated with an increased infection risk include general anesthesia, cesarean delivery for multifetal gestation, young maternal age and nulliparity, prolonged labor induction, obesity, and meconium-stained amnionic fluid (Acosta, 2012; Jazayeri, 2002; Kabiru, 2004; Leth, 2011; Siriwachirachai, 2010; Tsai, 2011).
Microbiology
Most female pelvic infections are caused by bacteria indigenous to the genital tract. Over the past 20 years, there have been reports of group A β-hemolytic streptococcus causing toxic shock-like syndrome and life-threatening infection (Aronoff, 2008; Castagnola, 2008; Nathan, 1994; Palep-Singh, 2007). Prematurely ruptured membranes are a prominent risk factor in these infections (Anteby, 1999). In reviews by Crum (2002) and Udagawa (1999) and their colleagues, women in whom group A streptococcal infection was manifested before, during, or within 12 hours of delivery had a maternal mortality rate of almost 90 percent and fetal mortality rate > 50 percent. In the past 10 years, skin and soft-tissue infections due to community-acquired methicillin-resistant Staphylococcus aureus—CA-MRSA—have become common (Chap. 64, p. 1251). Although this variant is not a frequent cause of puerperal metritis, it is commonly implicated in abdominal incisional infections (Anderson, 2007; Patel, 2007). Rotas and coworkers (2007) reported a woman with episiotomy cellulitis from CA-MRSA and hematogenously spread necrotizing pneumonia.
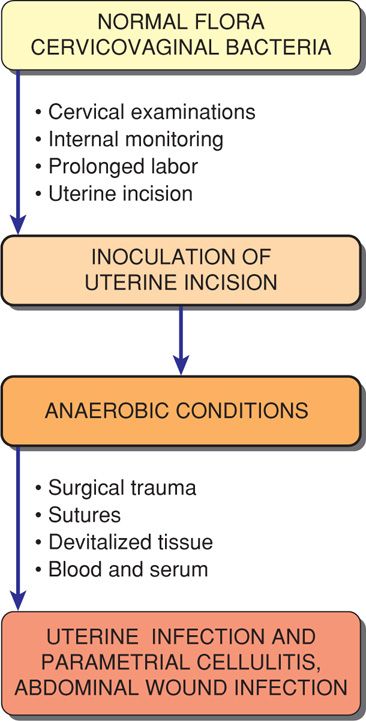
Common Pathogens. Bacteria commonly responsible for female genital tract infections are listed in Table 37-1. Generally, infections are polymicrobial, which enhances bacterial synergy. Other factors that promote virulence are hematomas and devitalized tissue. Although the cervix and vagina routinely harbor such bacteria, the uterine cavity is usually sterile before rupture of the amnionic sac. As the consequence of labor and delivery and associated manipulations, the amnionic fluid and uterus become contaminated with anaerobic and aerobic bacteria (Fig. 37-1). Intraamnionic cytokines and C-reactive protein are also markers of infection (Combs, 2013; Marchocki, 2013). In studies done before the use of antimicrobial prophylaxis, Gilstrap and Cunningham (1979) cultured amnionic fluid obtained at cesarean delivery in women in labor with membranes ruptured more than 6 hours. All had bacterial growth, and an average of 2.5 organisms was identified from each specimen. Anaerobic and aerobic organisms were identified in 63 percent, anaerobes alone in 30 percent, and aerobes alone in only 7 percent. Anaerobes included Peptostreptococcus and Peptococcus species in 45 percent, Bacteroides species in 9 percent, and Clostridium species in 3 percent. Aerobes included Enterococcus in 14 percent, group B streptococcus in 8 percent, and Escherichia coli in 9 percent of isolates. Sherman and coworkers (1999) later showed that bacterial isolates at cesarean delivery correlated with those taken from women with metritis at 3 days postpartum.
TABLE 37-1. Bacteria Commonly Responsible for Female Genital Infections
Aerobes
Gram-positive cocci—group A, B, and D streptococci, enterococcus, Staphylococcus aureus, Staphylococcus epidermidis
Gram-negative bacteria—Escherichia coli, Klebsiella, Proteus species
Gram-variable—Gardnerella vaginalis
Others
Mycoplasma and Chlamydia species, Neisseria gonorrhoeae
Anaerobes
Cocci—Peptostreptococcus and Peptococcus species
Others—Clostridium, Bacteroides, and Fusobacterium species, Mobiluncus species
The role of other organisms in the etiology of these infections is unclear. Chlamydial infections have been implicated in late-onset, indolent metritis (Ismail, 1985). Observations of Chaim and colleagues (2003) suggest that when cervical colonization of U urealyticum is heavy, it may contribute to the development of metritis. Finally, Jacobsson and associates (2002) reported a threefold risk of puerperal infection in a group of Swedish women in whom bacterial vaginosis was identified in early pregnancy (Chap. 65, p. 1276).
Bacterial Cultures. Routine pretreatment genital tract cultures are of little clinical use and add significant costs. Similarly, routine blood cultures seldom modify care. In two earlier studies done before perioperative prophylaxis was used, blood cultures were positive in 13 percent of women with postcesarean metritis at Parkland Hospital and 24 percent in those at Los Angeles County Hospital (Cunningham, 1978; DiZerega, 1979). In a later Finnish study, Kankuri and associates (2003) confirmed bacteremia in only 5 percent of almost 800 women with puerperal sepsis.
Pathogenesis and Clinical Course
Puerperal infection following vaginal delivery primarily involves the placental implantation site, decidua and adjacent myometrium, or cervicovaginal lacerations. The pathogenesis of uterine infection following cesarean delivery is that of an infected surgical incision (see Fig. 37-1). Bacteria that colonize the cervix and vagina gain access to amnionic fluid during labor. Postpartum, they invade devitalized uterine tissue. Parametrial cellulitis next follows with infection of the pelvic retroperitoneal fibroareolar connective tissue. With early treatment, infection is contained within the parametrial and paravaginal tissue, but it may extend deeply into the pelvis.
Fever is the most important criterion for the diagnosis of postpartum metritis. Intuitively, the degree of fever is believed proportional to the extent of infection and sepsis syndrome. Temperatures commonly are 38 to 39°C. Chills that accompany fever suggest bacteremia or endotoxemia. Women usually complain of abdominal pain, and parametrial tenderness is elicited on abdominal and bimanual examination. Leukocytosis may range from 15,000 to 30,000 cells/μL, but recall that cesarean delivery itself increases the leukocyte count (Hartmann, 2000). Although an offensive odor may develop, many women have foul-smelling lochia without evidence for infection, and vice versa. Some other infections, notably those caused by group A β-hemolytic streptococci, may be associated with scant, odorless lochia.
Treatment
If nonsevere metritis develops following vaginal delivery, then treatment with an oral antimicrobial agent is usually sufficient. For moderate to severe infections, however, intravenous therapy with a broad-spectrum antimicrobial regimen is indicated. Improvement follows in 48 to 72 hours in nearly 90 percent of women treated with one of several regimens. Persistent fever after this interval mandates a careful search for causes of refractory pelvic infection. These include a parametrial phlegmon—an area of intense cellulitis; an abdominal incisional or pelvic abscess or infected hematoma; and septic pelvic thrombophlebitis. In our experience, persistent fever is seldom due to antimicrobial-resistant bacteria or due to drug side effects. The woman may be discharged home after she has been afebrile for at least 24 hours, and further oral antimicrobial therapy is not needed (Dinsmoor, 1991; French, 2004).
Choice of Antimicrobials. Although therapy is empirical, initial treatment following cesarean delivery is directed against elements of the mixed flora shown in Table 37-1. For infections following vaginal delivery, as many as 90 percent of women respond to regimens such as ampicillin plus gentamicin. In contrast, anaerobic coverage is included for infections following cesarean delivery (Table 37-2).
TABLE 37-2. Antimicrobial Regimens for Intravenous Treatment of Pelvic Infection Following Cesarean Delivery
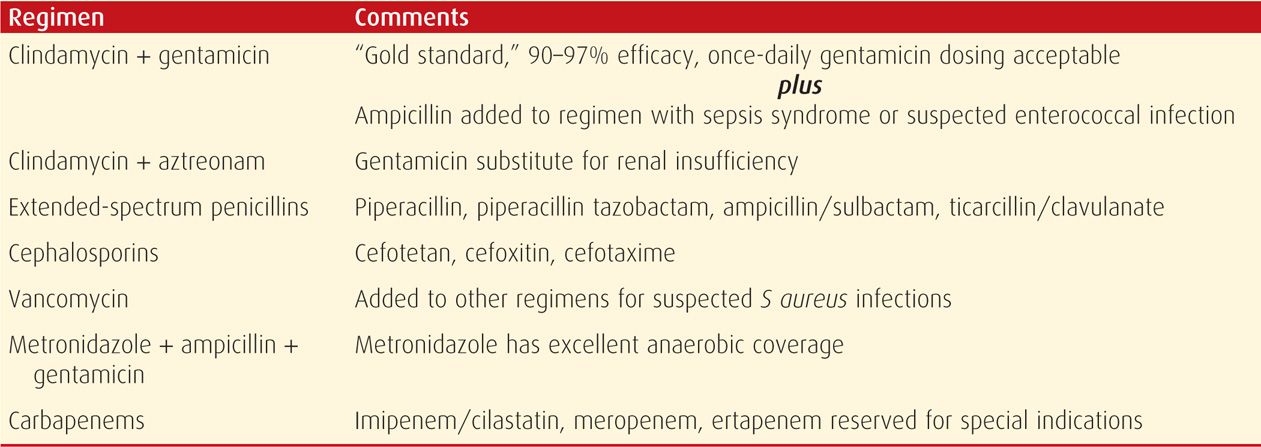
In 1979, DiZerega and colleagues compared the effectiveness of clindamycin plus gentamicin with that of penicillin G plus gentamicin for treatment of pelvic infections following cesarean delivery. Women given the clindamycin-gentamicin regimen had a 95-percent response rate, and this regimen is still considered by most to be the standard by which others are measured (French, 2004). Because enterococcal cultures may be persistently positive despite this standard therapy, some add ampicillin to the clindamycin-gentamicin regimen, either initially or if there is no response by 48 to 72 hours (Brumfield, 2000).
Many authorities recommend that serum gentamicin levels be periodically monitored. At Parkland Hospital, we do not routinely do so if the woman has normal renal function. Once-daily dosing versus multiple-dosing with gentamicin provides adequate serum levels, and either method has similar cure rates (Livingston, 2003).
Because of potential nephrotoxicity and ototoxicity with gentamicin in the event of diminished glomerular filtration, some have recommended a combination of clindamycin and a second-generation cephalosporin to treat such women. Others recommend a combination of clindamycin and aztreonam, which is a monobactam compound with activity similar to the aminoglycosides.
The spectra of β-lactam antimicrobials include activity against many anaerobic pathogens. Some examples include cephalosporins such as cefoxitin, cefotetan, cefotaxime, and ceftriaxone, as well as extended-spectrum penicillins such as piperacillin, ticarcillin, and mezlocillin. β-Lactam antimicrobials are inherently safe and except for allergic reactions, are free of major toxicity. The β-lactamase inhibitors, clavulanic acid, sulbactam, and tazobactam, have been combined with ampicillin, amoxicillin, ticarcillin, and piperacillin to extend their spectra. Metronidazole has superior in vitro activity against most anaerobes. This agent given with ampicillin and an aminoglycoside provides coverage against most organisms encountered in serious pelvic infections. It is also used to treat Clostridium difficile colitis.
Imipenem and similar antimicrobials are in the carbapenem family. These offer broad-spectrum coverage against most organisms associated with metritis. Imipenem is used in combination with cilastatin, which inhibits its renal metabolism. Preliminary findings with ertapenem indicated suboptimal outcomes (Brown, 2012). It seems reasonable from both a medical and an economic standpoint to reserve these drugs for serious nonobstetrical infections.
Vancomycin is a glycopeptide antimicrobial active against gram-positive bacteria. It is used in lieu of β-lactam therapy for a patient with a type 1 allergic reaction and given for suspected infections due to Staphylococcus aureus and to treat C difficile colitis (Chap. 54, p. 1074).
Perioperative Prophylaxis
As discussed, administration of antimicrobial prophylaxis at the time of cesarean delivery has remarkably reduced the postoperative pelvic and wound infection rates. Numerous studies have shown that prophylactic antimicrobials reduce the pelvic infection rate by 70 to 80 percent (Chelmow, 2001; Dinsmoor, 2009; Smaill, 2010; Witt, 2011). The observed benefit applies to both elective and nonelective cesarean delivery and also includes a reduction in abdominal incisional infection rates.
Single-dose prophylaxis with ampicillin or a first-generation cephalosporin is ideal, and both are as effective as broad-spectrum agents or a multiple-dose regimen (American College of Obstetricians and Gynecologists, 2011). Extended-spectrum prophylaxis with azithromycin added to standard single-dose prophylaxis has shown a further reduction in postcesarean metritis rates (Tita, 2008). These findings need to be verified. Women known to be colonized with methicillin-resistant Staphylococcus aureus—MRSA—are given vancomycin in addition to a cephalosporin (Chap. 64, p. 1251). Finally, it is controversial whether the infection rate is lowered more if the selected antimicrobial is given before the skin incision compared with after umbilical cord clamping (Baaqeel, 2012; Macones, 2012; Sun, 2013). The American College of Obstetricians and Gynecologists (2011) has concluded that the evidence favors predelivery administration. There may be additive salutary effects of preoperative vaginal cleansing with povidone-iodine rinse or application of metronidazole gel (Haas, 2013; Reid, 2011; Yildirim, 2012).
Other Methods of Prophylaxis. Several studies have evaluated the value of prenatal cervicovaginal cultures. These are obtained in the hope of identifying pathogens that might be eradicated to decrease incidences of preterm labor, chorioamnionitis, and puerperal infections. Unfortunately, treatment of asymptomatic vaginal infections has not been shown to prevent these complications. Carey and coworkers (2000) reported no beneficial effects for women treated for asymptomatic bacterial vaginosis. Klebanoff and colleagues (2001) reported a similar postpartum infection rate in women treated for second-trimester asymptomatic Trichomonas vaginalis infection compared with that of placebo-treated women.
Technical maneuvers done to alter the postpartum infection rate have been studied with cesarean delivery. For example, allowing the placenta to separate spontaneously compared with removing it manually lowers the infection risk. However, changing gloves by the surgical team after placental delivery does not (Atkinson, 1996). Exteriorizing the uterus to close the hysterotomy may decrease febrile morbidity (Jacobs-Jokhan, 2004). Postdelivery mechanical lower segment and cervical dilatation have not been shown to be effective (Liabsuetrakul, 2011). No differences were found in postoperative infection rates when single- versus two-layer uterine closure was compared (Hauth, 1992). Similarly, infection rates are not appreciatively affected by closure versus nonclosure of the peritoneum (Bamigboye, 2003; Tulandi, 2003). Importantly, although closure of subcutaneous tissue in obese women does not lower the wound infection rate, it does decrease the wound separation incidence (Chelmow, 2004; Magann, 2002; Naumann, 1995). Similarly, skin closure with staples versus suture has a higher incidence of noninfectious skin separation (Mackeen, 2012; Tuuli, 2011).
Complications of Uterine and Pelvic Infections
In more than 90 percent of women, metritis responds to treatment within 48 to 72 hours. In some of the remainder, any of several complications may arise. These include wound infections, complex pelvic infections such as phlegmons or abscesses, and septic pelvic thrombophlebitis (Jaiyeoba, 2012). As with other aspects of puerperal infections, the incidence and severity of these complications are remarkably decreased by perioperative antimicrobial prophylaxis.
 Abdominal Incisional Infections
Abdominal Incisional Infections
Wound infection is a common cause of persistent fever in women treated for metritis. Other wound infection risk factors include obesity, diabetes, corticosteroid therapy, immunosuppression, anemia, hypertension, and inadequate hemostasis with hematoma formation. If prophylactic antimicrobials are given as described above, the incidence of abdominal wound infection following cesarean delivery ranges from 2 to 10 percent depending on risk factors (Andrews, 2003; Chaim, 2000).
Incisional abscesses that develop following cesarean delivery usually cause persistent fever or fever beginning about the fourth day. In many cases, antimicrobials had been given to treat pelvic infection, yet fever persisted. There is wound erythema and drainage. Although organisms that cause wound infections are generally the same as those isolated from amnionic fluid at cesarean delivery, hospital-acquired pathogens may also be causative (Emmons, 1988; Owen, 1994). Treatment includes antimicrobials, surgical drainage, and debridement of devitalized tissue. The fascia is carefully inspected to document integrity.
Local wound care is typically completed twice daily. Before each dressing change, procedural analgesia is tailored to wound size and location, and oral, intramuscular, or intravenous dosage routes are suitable. Topical lidocaine may also be added. Necrotic tissue is removed, and the wound is repacked with moist gauze. At 4 to 6 days, healthy granulation tissue is typically present, and secondary en bloc closure of the open layers can usually be accomplished (Wechter, 2005). With this closure, a polypropylene or nylon suture of appropriate gauge enters 3 cm from one wound edge. It crosses the wound to incorporate the full wound thickness and emerges 3 cm from the other wound edge. These are placed in series to close the opening. In most cases, sutures may be removed on postprocedural day 10. Wound vacuum device use is gaining popularity. However, its efficacy remains unproven in randomized trials.
Wound Dehiscence
Wound disruption or dehiscence refers to separation of the fascial layer. This is a serious complication and requires secondary closure of the incision in the operating room. McNeeley and associates (1998) reported a fascial dehiscence rate of approximately 1 per 300 operations in almost 9000 women undergoing cesarean delivery. Most disruptions manifested on about the fifth postoperative day and were accompanied by a serosanguineous discharge. Two thirds of 27 fascial dehiscences identified in this study were associated with concurrent fascial infection and tissue necrosis.
Necrotizing Fasciitis
This uncommon, severe wound infection is associated with high mortality rates. In obstetrics, necrotizing fasciitis may involve abdominal incisions, or it may complicate episiotomy or other perineal lacerations. As the name implies, there is significant tissue necrosis. Of the risk factors for fasciitis summarized by Owen and Andrews (1994), three of these—diabetes, obesity, and hypertension—are relatively common in pregnant women. Like pelvic infections, these wound complications usually are polymicrobial and are caused by organisms that make up the normal vaginal flora. In some cases, however, infection is caused by a single virulent bacterial species such as group A β-hemolytic streptococcus. Occasionally, necrotizing infections are caused by rarely encountered pathogens (Swartz, 2004).
Goepfert and coworkers (1997) reviewed their experiences with necrotizing fasciitis at the University of Alabama Birmingham Hospital. Nine cases complicated more than 5000 cesarean deliveries—frequency of 1.8 per 1000. In two women, the infection was fatal. In a report from Brigham and Women’s and Massachusetts General Hospitals, Schorge and colleagues (1998) described five women with fasciitis following cesarean delivery. None of these women had predisposing risk factors, and none died.
Infection may involve skin, superficial and deep subcutaneous tissues, and any of the abdominopelvic fascial layers (Fig. 37-2). In some cases, muscle is also involved—myofasciitis. Although some virulent infections, for example, from group A β-hemolytic streptococci, develop early postpartum, most of these necrotizing infections do not cause symptoms until 3 to 5 days after delivery. Clinical findings vary, and it is frequently difficult to differentiate more innocuous superficial wound infections from an ominous deep fascial one. A high index of suspicion, with surgical exploration if the diagnosis is uncertain, may be lifesaving. We aggressively pursue early exploration. Certainly, if myofasciitis progresses, the woman may become ill from septicemia. Profound hemoconcentration from capillary leakage with circulatory failure commonly occurs, and death may soon follow as described in Chapter 47 (p. 947).
FIGURE 37-2 Necrotizing fasciitis involving the abdominal wall and Pfannenstiel incision. The skin rapidly became dusky and gangrenous, and pus is seen exuding from the left angle of the incision. Extensive debridement and supportive therapy were lifesaving.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree