Chapter 5. Problems with prematurity
Although there are separate chapters in the book for X-rays and other images, some pictures of scans are included in this chapter to help build up a more realistic representation of the difficulties that commonly accompany the day-to-day management of the premature infant.
QUESTION 1
A 27 week baby is brought to the neonatal unit. He was born in good condition, requiring minimal resuscitation and is put on to nasal CPAP in 25% oxygen. Over the next four hours, his condition deteriorates. Oxygen requirement increases, there is obvious recession and he is having recurrent apnoeas. A capillary gas at this point shows a mixed acidosis.
i) Which of the following actions would you consider? Choose the three most appropriate answers.
a. Continue and reassess in an hour
b. Increase CPAP pressure
c. Intubate and give surfactant, and extubate back onto CPAP
d. Intubate, give surfactant, and ventilate
e. Give antibiotics
f. Load with caffeine
g. CXR
h. Change to trigger assist CPAP.
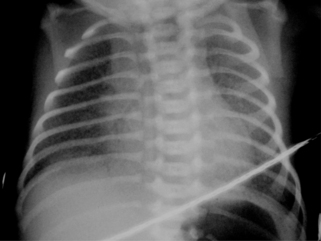 |
| Figure 5.1. |
A CXR is obtained.
ii) Describe the CXR.
The baby is given surfactant and antibiotics and is ventilated but pressures and oxygen requirement continue to increase. Arterial blood gases are just acceptable at pressures of 26/4 in 80% oxygen. The baby suddenly becomes profoundly bradycardic and oxygen saturations fall to below 50%.
iii) What four options would you immediately investigate?
Transillumination shows a very bright hemithorax, and there is some improvement following insertion of a chest drain. Two hours later, there is further deterioration and a pneumothorax is detected on the opposite side. A chest drain results in re-inflation but the clinical condition does not improve significantly.
12 hours after the first pneumothorax he is in 100% oxygen, with pressures 32/4 and an arterial blood gas shows the following:
| pH | 7.18 |
| pO 2 | 2.4 kPa |
| pCO 2 | 9.8 kPa |
| BE | –4 mEq/L |
| HCO 3 | 28 mmol/L |
CXR shows relatively solid lungs with an air bronchogram. The pneumothoraces are well drained.
iv) Which of the following actions would you consider?
a. Increase PIP
b. Increase PEEP
c. Repeat surfactant
d. HFOV
e. Nitric oxide
f. Discuss palliative care with parents
g. Diuretics
h. Tolazoline.
The baby stabilises on HFOV over the next few days and returns to conventional ventilation when MAP falls to 12. He remains on conventional ventilation for the next 21 days, at the end of which pressure is 20/4 and he is in 60% oxygen. A CXR is obtained (Figure 5.2).
v) Describe the CXR.
vi) Which of the following treatments would you consider? Choose two answers.
a. Antibiotics
b. Diuretics
c. Aminophylline
d. Dexamethasone
e. Indomethacin
f. Inhaled corticosteroids
g. Inhaled bronchodilators
h. Disodium cromoglycate.
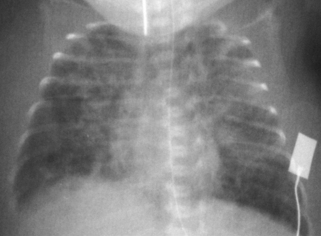 |
| Figure 5.2 |
As part of the assessment of this infant, an echocardiogram has been performed which shows a large and clinically significant duct. The infant is now 4 weeks old (CGA 31 weeks).
vii) Which of the following interventions would you consider?
a. Fluid restriction
b. Digoxin
c. Indomethacin
d. Ibuprofen
e. Surgical ligation
f. Diuretics
g. Expectant treatment
h. Prostacycline
i. ACE inhibitors.
After duct ligation and a course of dexamethasone, the baby is weaned off all ventilation and progresses onto low flow oxygen. He is ready to go home, gaining weight but still requiring 0.5 L low flow oxygen.
viii) What advice would you give the parents and what extra medication might you consider?
QUESTION 2
QUESTION 3
Proliferative retinopathy of prematurity (ROP) has developed and the ophthalmologists feel laser therapy is essential. Which of the following statements are correct?
i) Laser therapy prevents progression of ROP in more than 75% cases.
ii) Laser therapy is necessary if there are 5 continuous or 8 cumulative clock hours of stage 3 ROP in zones 1 or 2 in the presence of plus disease.
iii) Immediate laser therapy is essential for any stage of ROP with plus disease in zone 1.
iv) Laser therapy is essential for any stage of ROP in zone 1 whether or not plus disease is present.
v) Laser treatment can be performed up to 4 weeks after detection of threshold criteria.
vi) Laser therapy is more effective than cryotherapy at prevention of proliferative ROP.
vii) Laser therapy is preferred to cryotherapy for treatment of ROP.
viii) Laser therapy must be done under general anaesthetic.
ix) In infants where laser therapy has successfully treated retinopathy, long-term visual prognosis is excellent.
QUESTION 4
A 29 week infant is now 2 weeks old and has been off CPAP for five days. He is noticed to have bradycardias which are often associated with a fall in oxygen saturations. He has had several apnoeas and recently has required brief respiratory support (mask ventilation) until he started to breathe again. Caffeine was started 8 days ago and is being continued. Which of the following statements are correct?
i) Apnoea of prematurity is uncommon after 30 weeks’ gestation and further investigation is essential.
ii) There should be a low threshold for septic screen and antibiotic treatment.
iii) There is a strong association between apnoea and gastro-oesophageal reflux (GOR).
iv) Central and obstructive apnoea are easily distinguishable and equally common.
v) The fact that this infant is receiving caffeine makes central apnoea unlikely as a diagnosis.
vii) Doxapram is useful as a first-line agent for the treatment of apnoea.
viii) Kinaesthetic stimulation may be useful in infants with troublesome apnoeas.
ix) Blood transfusion may be helpful in the treatment of apnoea if haemoglobin is low.
x) Recent immunisation could well be a precipitating event.
QUESTION 5
Which of the following statements are true about hypotension and its management?
i) Infants with RDS are often hypotensive.
ii) Infants whose mothers have received antenatal steroids are more likely to be hypotensive.
iii) A pneumothorax may cause an increase in the cerebral blood flow velocity and systemic hypotension.
iv) Hypotension is a risk factor for germinal matrix haemorrhage.
v) Dopamine works on alpha-adrenergic receptors only.
vi) Dobutamine works on alpha-adrenergic receptors only.
vii) Dopamine is more effective alone than dobutamine alone.
viii) Adrenaline increase the blood pressure by peripheral vasoconstriction.
ix) Adrenaline has a similar effect on the blood pressure to dopamine.
QUESTION 6
A chest X-ray is performed.
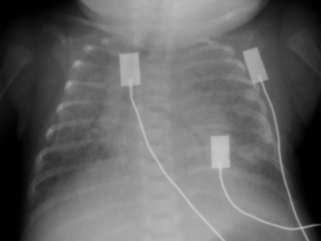 |
| Figure 5.3. |
i) Describe four abnormalities on the chest X-ray.
As a consequence of what you see a skeletal survey is also carried out. The X-ray of the legs as part of the skeletal survey is shown in Figure 5.4.
 |
| Figure 5.4 |
ii) Describe four abnormalities on the X-ray of the legs.
iv) Which of the following are likely to be associated with the diagnosis?
a. Indomethacin
b. Caffeine
c. Furosemide
d. Dexamethasone
e. Immobilisation
f. Alkaline phosphatase >500 IU/L
g. Urine calcium:phosphate ratio >1
h. Serum calcium level <2 mmol/L.
QUESTION 7
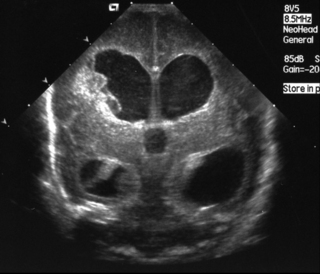
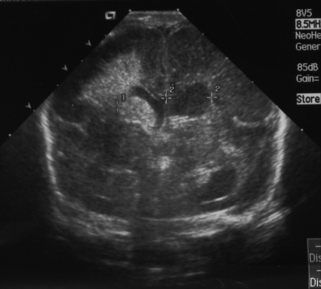
A 26 week gestation infant requires ventilation from birth for moderately severe respiratory distress syndrome. He is moderately stable in 40% oxygen, pressures 22/4, and dopamine has been needed to maintain a satisfactory blood pressure. A routine ultrasound scan performed on day 2 is shown in Figure 5.5.
 |
| Figure 5.5 |
i) What abnormality is shown?
ii) What is the likely prognosis?
iii) The parents want to know how common this is and why this has happened. What do you tell them?
QUESTION 8
A 25 week gestation baby has been ventilated for 4 days during which ventilatory requirements did not exceed a peak pressure of 20cmH 2O. Blood pressure is stable and inotropic support was not required. Bilateral small GMHs were noted on day one, which did not appear to increase in size on subsequent scans although there was thought to be a small amount of free blood within the ventricles. After 4 days of weaning ventilation, the baby is stable on CPAP.
On day 13, some abnormal movements are noted, and the baby is thought to have had a seizure. A repeat cranial ultrasound is performed, the first for five days. The scan is shown below.
 |
| Figure 5.6. |
i) What does the scan show?
ii) Why has it happened?
iii) What will you tell the parents?
iv) The parents have been studying the internet and have found reports on the use of acetazolamide, repeated ventricular taps and ventriculostomy, in the management of PHVD. What will you tell them about these treatment options and then explain to them what your plan will be?
QUESTION 9
A 26 week gestation infant has suffered from moderately severe respiratory distress and has required high frequency oscillation ventilation, requiring a mean airway pressure of 16 mmH 2O. A significant GMH/IVH is noted on day two with a smaller haemorrhage on the left. Despite the use of both dopamine and dobutamine blood pressure has remained unstable. The baby developed a tension pneumothorax on day three but responded well to prompt drainage. On day five, the baby deteriorates further with increasing ventilation requirements, coagulopathy, sudden fall in haemoglobin and marked hypotension. Sepsis is suspected and antibiotics are commenced. A cerebral ultrasound is performed 24 hours later.
 |
| Figure 5.7. |
i) Describe the scan.
ii) Why has this happened?
iii) What will you tell the parents?
iv) What is your next step in managing this baby?
QUESTION 10
A 28 week gestation baby was born following prolonged rupture of membranes. Mother had developed a pyrexia which had not responded to 24 hours of antibiotics and an emergency section was performed. pH at birth was 6.95 and prolonged resuscitation was required. Surprisingly, the baby stabilised relatively quickly and only a short period of ventilation was required. Initial cerebral ultrasound showed no evidence of GM-IVH but there was some debate over increased periventricular echogenicity. At 6 weeks postnatal age, a routine ultrasound scan was performed and is shown in Figure 5.8.
i) Describe the scan.
ii) Why has this happened?
iii) What will you tell the parents?
iv) What is your next step in managing this baby?
 |
| Figure 5.8 |
ANSWER 1
i) d, e and g are most appropriate.
a. This would not be advisable. An infant becoming progressively more symptomatic is extremely unlikely to show spontaneous improvement at this gestation.
b. If there is widespread atelectasis, increased CPAP pressure may help by recruiting more lung, but would not be a sensible first-line option. It should not be considered unless the CXR confirms the atelectasis, and unless surfactant replacement has been given.
c. Practice differs with respect to this option. There are some who believe this is appropriate and others who feel disturbance caused to the baby is likely to jeopardise stability and it is far more rational to continue gentle ventilation for some hours after administration. Some fairly strong opinions are held in the face of an extremely limited evidence base.
d. As mentioned above practice varies but this is probably the safest option. It is important that surfactant is given properly and that the most minimal ventilation possible is provided, and the infant is weaned as quickly as possible.
f. This might be appropriate in due course but a lack of respiratory drive is unlikely to be the main component of this infant’s respiratory difficulties.
g. A CXR is essential in this situation as, although respiratory distress syndrome is the most likely diagnosis, other possibilities cannot be excluded, such as a pneumothorax.
h. Newer advanced CPAP modes, e.g. trigger assist and pressure trigger assist, are becoming increasingly popular. However, the exact circumstances in which use is most beneficial are unclear. In this particular situation, surfactant would seem to be the most important component of immediate management.
ii) The chest X-ray shows changes which are consistent with moderate respiratory distress syndrome. There is a homogeneous ground-glass appearance with an air bronchogram. The air bronchogram is more prominent behind the heart which can be a normal observation. The X-ray is slightly rotated making comments about heart size unreliable.
iii) In the case of any sudden deterioration in an infant, think DOPE:
Displacement – although much can be done to optimise the stability of endotracheal tubes, this still remains a common reason for deterioration.
Obstruction – many babies produce copious secretion of variable viscosity and tube obstruction is not uncommon.
Pneumothorax – although the incidence of pneumothorax has fallen significantly since the advent of surfactant replacement therapy, it is still an important and potentially lethal reason for sudden deterioration.
Equipment – equipment failure may be a cause with tube disconnection being the commonest mechanical problem.
iv)
a. Although increasing PIP may improve oxygenation, it is unlikely to be highly effective while continuing to ventilate conventionally as the elevated pressure is not sustained for long enough to recruit atelectatic alveoli.
b. Increasing PEEP may help recruit alveoli but very high pressure may be needed in a very sick infant. Research has shown this may be effective but the pressures required are usually outside the comfort zone for many practising neonatologists. Increasing PEEP will improve mean airway pressure but at the cost of decreased tidal volume, and the acidosis may worsen.
c. This may be worth a trial, particularly if insufficient treatment has been given previously. Although randomised controlled trials do not show any evidence of benefit from more than two doses, it must be remembered that this refers to a large group with heterogeneous conditions, and does not preclude the possibility of a response in selected individuals. Surfactant is inactivated by the inflammatory exudate that develops in RDS, and it may therefore be necessary to use higher than normal doses.
There still remains some debate about the most appropriate use of HFOV but there is good evidence to support its use for rescue ventilation, when the higher sustained MAP will assist in the recruitment of alveoli, but may require several hours in which to do so.




Get Clinical Tree app for offline access
e. Although it is tempting to try nitric oxide when oxygen requirements are high, the currently available evidence does not support use in preterm infants. Nitric oxide is indicated when there is evidence of pulmonary hypertension. In this case the primary problem is alveolar collapse. 1
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


