Chapter 29 Preparticipation Physical Evaluation
Speaking Intelligently
The preparticipation physical evaluation should be designed specifically to ensure the health and well-being of young athletes; that is, to identify medical conditions that put the athlete at risk for sudden death or life-threatening complications. In addition, it strives to identify and rehabilitate prior injuries, as well as provide strategies to prevent these injuries in the future. Currently, 49 of 50 states require a preparticipation physical evaluation (PPE).1 The requirements of these evaluations, however, vary widely from state to state. For example, some states allow for the PPE to be completed by nonphysician extenders, chiropractors, or even athletic trainers.
Medical Knowledge and Patient Care
Background and Definitions
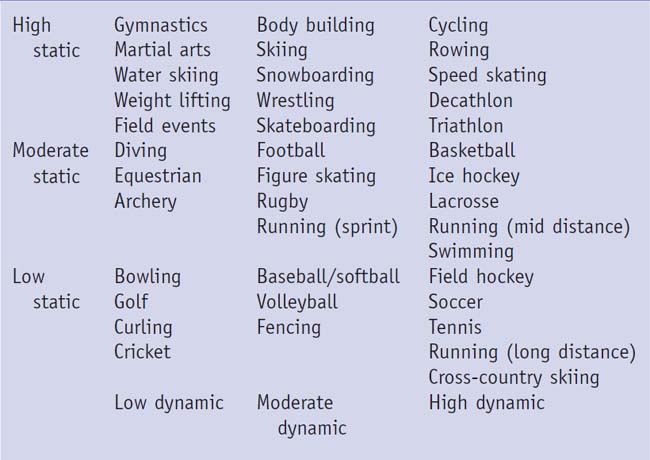
The history should begin with an understanding of what sport the athlete intends to play. Sports have been categorized according to a grade of contact—low, moderate, or high (Table 29-1). In addition, activities have been classified based on dynamic (volume load) or static (pressure load) on the heart (Table 29-2).2 Understanding these classifications will allow the pediatrician to consider the risks associated with each sport.
Table 29-1 Classification of Sport by Degree of Contact
| High Contact/Collision | Limited Contact | Low-Noncontact |
|---|---|---|
| Football | Baseball | Badminton |
| Ice hockey | Bicycling | Bowling |
| Basketball | Gymnastics | Golf |
| Field hockey | Skating | Running |
| Lacrosse | Skiing | Strength training |
| Martial arts | Volleyball | Crew |
| Rugby | Cheerleading | Tennis |
| Soccer | Swimming | |
| Wrestling | ||
| Diving |
Data from American Academy of Pediatrics, Committee on Sports Medicine and Fitness: Medical conditions affecting sports participation, Pediatrics 2001;107:1205.
History
A review of the general medical history is appropriate, including the use of any medication or supplement that may affect performance. A few conditions deserve special attention. A prior history of syncope or near-syncope during exercise or palpitations is especially concerning and should prompt further workup, including evaluation by a pediatric cardiologist. The risk for sudden death in young athletes is estimated to be 1 in 200,000.3 Hypertrophic cardiomyopathy is the most common cause, followed by congenital coronary artery abnormalities.4 Guidelines for athletes with known cardiovascular abnormalities have been supported by the American Heart Association and are based on the 36th Bethesda Conference Guidelines for Participation.5 Exercise-induced bronchospasm and/or asthma is relatively common, and a history of wheezing during exercise may need further treatment. Concussions occur most commonly with high-impact sports and need to be taken seriously, as does a history of “stingers” or “burners.” A seizure disorder may not result in disqualification, depending on the sport, but it must be well controlled. Inquiring specifically about a female athlete’s menstrual history may uncover primary or secondary amenorrhea and raise concern for the female athlete triad. Athletes should be questioned about recent illness, particularly infectious mononucleosis. Previous musculoskeletal injury is the strongest predictor of sports injury,6 and up to 20% of high school athletes will have a musculoskeletal injury that requires medical attention.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree