Complications
• Almost all complications of Preg are more likely w/ multi gestations
• Discordance: One twin larger than the other; clinically signif when greater than 20%. Calculate discordance % as: [(larger EFW – smaller EFW) / larger EFW] × 100.
• Monochorionic monoamnionic twins: Cord entanglement & subseq cord accident; delivered early at 32–34 w
• Monochorionic diamnionic twins: Twin to twin transfusion syndrome (TTTS)
Due to bld vessel anastomoses w/i single placenta w/ pressure diff
Occurs in ∼15% of monochorionic diamniotic twin gestations
Donor twin: Bld shunted away
Recipient twin: Bld shunted toward
Stages of TTTS (J Perinatol 1999;19:550):
1. Polyhydramnios/oligohydramnios, donor bladder present
2. Poly/oli, donor bladder absent
3. Poly/oli, abn Dopplers
4. Poly/oli, hydrops of recipient
5. IUFD of one or both fetuses
Rx:
Laser photocoagulation of vessel anastomoses (Stage II or worse)
Serial amnioreduction
Selective reduction (termination) of one fetus
CERVICAL INSUFFICIENCY/SHORT CERVIX
Definition and Epidemiology (Obstet Gynecol 2012;120:964)
• Inability of cervix to maintain a Preg until term
• Weakened cervical tissue leading to loss of Preg, often 2nd trimester
Etiology
• Congen: Collagen dz, Müllerian fusion anomalies, h/o DES exposure in utero
• Acq: Cervical trauma, D&C, cervical manipulation (LEEP, cold knife cone)
• Abnormality in cervical remodeling (4 steps: Softening, ripening, dilation, repair)
Clinical Manifestation
• Asymptomatic/painless cervical dilation/effacement
• Often h/o painless dilation & deliv in the 2nd trimester w/ prior pregnancies
Physical Exam
• Speculum exam can show a dilated cervix
• Digital exam reveals soft, effaced, & possibly dilated cervix
Diagnostic Workup/Studies
• When performing fetal anatomy US at 18–22 w, can perform CL via transabdominal US. CL <25 mm on transabdominal → transvaginal US
Treatment and Medications
• For short cervix: Vaginal progesterone 200 mg micronized or 90 mg gel daily
• For short cervix or cervical insufficiency: Cervical Cerclage (Obstet Gynecol 2014;123:372)
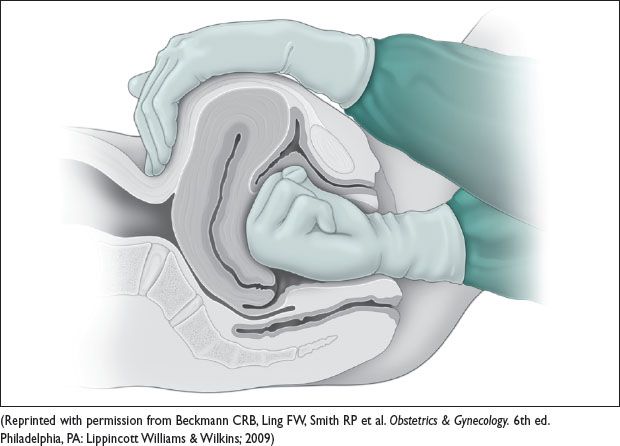
Surgical stitch placed circumferentially around the cervix
McDonald: “Purse-string” placed at cervicovaginal junction
Shirodkar: Requires dissection of the vesicovaginal & rectovaginal fascia to the level of the internal os
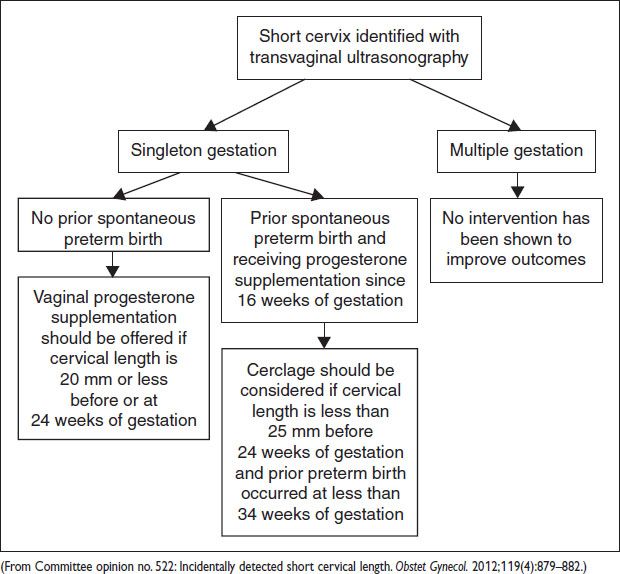
• When to treat:
Singleton Preg w/:
No prior spont preterm births → offer vaginal progesterone suppl if CL ≤20 mm at ≤24 w
Prior spont preterm birth (start progesterone injections weekly from 16–36 w) → consider cerclage if CL ≤25 mm at ≤24 w
Dilated cervix <24 w → consider rescue cerclage on individual basis
Multiples show no improv w/ progesterone & worse outcomes w/ cerclage
Figure 11.2 Management of short cervix
PRETERM PREMATURE RUPTURE OF MEMBRANES
Definition and Epidemiology (Obstet Gynecol 2013;122:918)
• PROM: Rupture of membranes before the onset of active labor (“premature” to labor)
• PPROM: Premature rupture of membranes <37 w (preterm GA and prior to labor)
• Occurs prior to 1/3 of preterm births
Etiology
• No consensus on the cause of PPROM – thought to be on spectrum of preterm labor
• Risk factors include intra-amniotic infxn, uterine over distension, smoking, connective tissue disorders, 2nd & 3rd trimester bleeding, nutritional deficiency, prior preterm deliv, symptomatic contractions, amniocentesis (leakage after amniocentesis more likely to stop & not lead to deliv)
Clinical Manifestation
• Leakage of amniotic fluid prior to labor
• If accompanied by mat fever or tachy, uterine fundal tenderness, fetal tachy, purulent or malodorous fluid there should be concern for intra-amniotic infxn
Physical Exam
• Sterile speculum exam (Obstet Gynecol. 1992;80:630; Am J Obstet Gynecol. 2000;183:1003)
• Avoid digital exam, esp if preterm. Single digital exam decreases latency to deliv.
Diagnostic Workup/Studies
• Clinical dx:
Leakage of fluid per vagina that is consistent w/ amniotic fluid (see below)
Signs of infxn should prompt deliv, regardless of prematurity, to ↓ risk of mat & neonat sepsis
Sterile speculum exam: Pooling of fluid in the vaginal vault sugg ROM
US: Oligohydramnios is often present, though not diagnostic
NST: Fetal tachy is often present w/ intra-amniotic infxn
Oligohydramnios → variable decelerations
• Lab tests:
Ferning: Place fluid from vaginal vault on a dry slide; salts in the amniotic fluid produce a delicate ferning pattern under microscope.
pH: Amniotic fluid has a basic pH → turns pH paper blue (nitrazine test)
Also nitrazine positive: Bld, bact vaginosis, semen.
• Diagnostic procedures
Indigo carmine amniotic infusion “tampon test”
Indigo carmine injected into the amniotic sac via amniocentesis
Tampon inserted vaginally to detect blue color indicating leakage of amniotic fluid
If amniocentesis performed to assess chorioamnionitis, get cell count, gram stain, gluc, & cx (aerobic/anaerobic/myco- and ureaplasma)
Management
• Previable (<24 w): May be managed outpt, w/o Abx, until viability
Major complications: Limb contractures, pulm hypoplasia
Should be offered termination via D&E or induction
• Early preterm (24–34 w):
Antenatal corticosteroids (up to 32–34 w depending on institutional protocol)
Admit to inpt observation in nearly all cases
No indication for tocolytics
Collect GBS culture
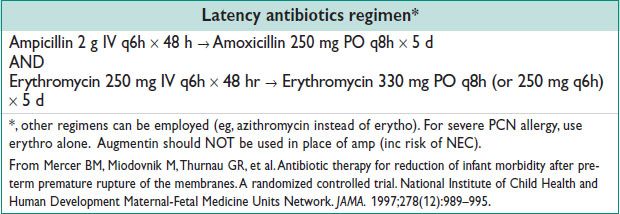
Latency Antibiotics
↑ duration of Preg (“latency period”) on avg 1 w
↓ neonat morbidity (respiratory distress, NEC)
Does not ↓ incid of chorio
Induction at 34 w gest or w/ signs of preterm labor, chorio, abruption, fetal distress
• ≥34 w (PLoS Med 2012;9:e1001208):
Unless contraindications exist to vaginal deliv, induction may be attempted
After 34 w, no difference in neonat sepsis btw induction & conservative mgmt, but trend toward ↓ neonat morbidity w/ induction
More likely to see variable decelerations during labor → ↑ CD for fetal intolerance
GBS status should be assessed during latency & appropriate therapy in labor
PRETERM LABOR
Definition and Epidemiology
• Labor (ctx + cervical dilation) occurring before 37 w gest
• Preterm labor occurs in ∼40–50% of all pregnancies
• Preterm deliv occurs in roughly 12% of pregnancies → ∼35% of all health care spending for infants in US
Etiology
• Poorly understood, but risk factors include multi gest/uterine over distension, bact infxn, placental abruption, cervical insufficiency, prior preterm labor
Clinical Manifestation
• Physical exam findings of labor including persistent uterine contractions (>4/20 min or 8/h) leading to changes in cervical effacement & dilation.
• Occ includes rupture of membranes
Physical Exam
• Painful uterine contractions leading to cervical change, and eval for PPROM, abruption, etc
Diagnostic Workup/Studies (Obstet Gynecol 2012;120:964)
• Pelvic exam:
Sterile speculum and digital exam to evaluate cervical dilation
Collect fFN swab
GBS swab if deliv is not imminent & has not been collected previously
Sterile vaginal exam to directly assess cervix (must be after fFN collected!)
• Labs:
fFN: Basement membrane peptide present in amniotic membranes. Can be tested via cervical swab – not reliable w/ vaginal bleeding, recent (<24 h) intercourse or vaginal exam. If negative, 95% do not deliver in 14 d (Br J Obstet Gyneacol 1996;103:648)
• US:
Transvaginal US measurement of cervical length <25 mm is a/w preterm deliv
Treatment and Medications (Obstet Gynecol 2012;119:1308)
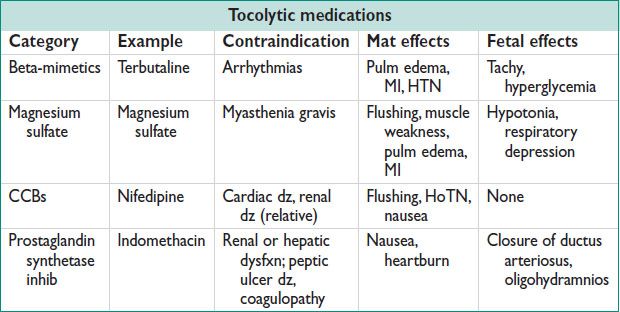
• Prior to 34 w gest:
Administer corticosteroids for fetal lung maturation
Tocolytics only to allow for Cort administration or mat xfer – no pharmacotherapy proven to stop preterm labor
• Prior to 32 w gest:
Magnesium sulfate administration for fetal neuroprotection (N Engl J Med 2008;359:895)
• Prevention of recurrent preterm birth:
17-OH progesterone caproate (250 mg IM weekly) starting at 16 w until 36 w (30% reduction in recurrent preterm deliv) (N Engl J Med 2003;348:2379)
Serial cervical length measurements starting at 16–24 w/ poss cerclage placement if cervical length <25 mm. See short cervix, above. (Am J Obstet Gynecol 2009;201:375)
POSTPARTUM HEMORRHAGE (PPH)
Definition and Epidemiology (Obstet Gynecol 2006;108:1039)
• Bld loss >500 cc w/ a vaginal deliv or >1000 cc w/ a CD (total EBL)
• Common, w/ incid 2–3% of all births in the United States (Am J Obstet Gynecol 2010;202:353). Clinically, excessive bld loss causing symptomatic anemia (palps, SOB, lightheadedness) &/or signs of hypovolemia (tachy, HoTN, hypoxemia)
• Major cause of mat mortality (Cochrane Database Syst Rev 2007;1:CD003249). Risk of death 1:1000 births in developing countries & 1:100,000 births in developed countries.
• Primary (Early) PPH: W/i 24 h of deliv, caused by uterine atony, genital tract lacerations, bladder or urethral lacerations, retained products of conception, invasive placentation (eg, accreta), uterine rupture or inversion, coagulopathy
• Secondary (Late) PPH: From 24 h–12 w after deliv, caused by infxn, retained products of conception, placental site subinvolution, coagulopathy
Etiology
Uterine atony (most common cause) from: Distended uterus (multi gest, polyhydramnios); impaired uterine contractility (tocolytic meds or anesthetics, prolonged use of meds for labor induction) (Am J Obstet Gynecol 2011;204:56); intraamniotic infxn (chorio); distended bladder (prevents lower uterine segment contraction)
• Trauma: Genital tract laceration (vaginal or cervical); surgical injury
• Retained placental tissue (normally or abnormally implanted)
• Coagulopathy: Consumptive coagulopathy from ongoing hemorrhage; HELLP syn; sev preeclampsia; amniotic fluid embolism (w/ DIC); sepsis; fetal demise
• Bleeding may not be apparent if intra- or retroperitoneal bleed, or if genital tract hematoma
Physical Exam
• Bimanual exam to assess for atony or retained placental tissue. Consider bedside US to evaluate for retained placental tissue.
• Thorough inspection of the genital tract for laceration or hematoma
• Tachy & HoTN seen when bld loss approaches 1500–2000 cc
Diagnostic Workup/Studies
• Identify origin of bleeding:
Visualize cervix & vagina to evaluate for lacerations
Bimanual uterine massage to assess for uterine atony
Bedside US to view poss retained products
Manual evacuation of uterine cavity for poss extraction of retained products
Place Foley catheter (distended bladder may contribute to poor uterine tone)
• Labs: Bld type & cross, CBC, PT/INR, PTT, fibrinogen. 5 mL of bld in red top tube at bedside → clot in 8–10 min if fibrinogen >150 mg/dL.
• Immediately begin treating for the suspected origin of hemorrhage (eg, for uterine atony administer uterotonics, perform bimanual uterine massage)
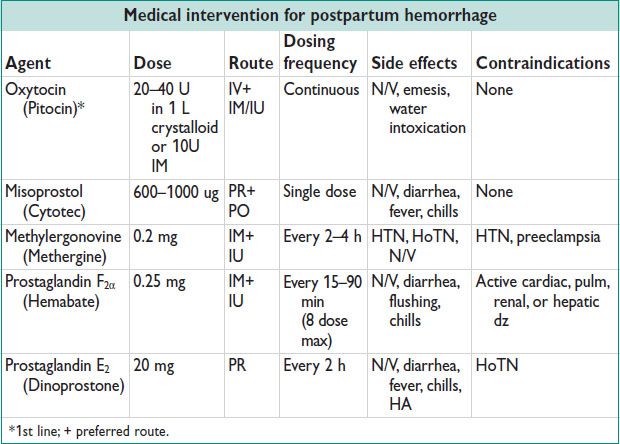
Medical Therapies for PPH
• Oxytocin (Pitocin) Routine use during the 3rd stage of labor significantly reduces the incid of PPH (Cochrane Database Syst Rev 2001;(4):CD001808). Can bolus for PPH, though some risk for HoTN. Onset of action: ∼1 min (IV), 3–5 min (IM).
• Misoprostol May cause fever, chills/shivering, GI distress. Onset of action: 100 min (PR) (vs. 8 min PO, 11 min SL, 20 min PV)
• Methylergonovine Onset of action: 2–5 min (IM).
• Carboprost tromethamine (Hemabate) May cause bronchospasm in asthmatics. May rpt q15–90 min as needed, w/ max cumulative dose 2 mg. Onset of action: 15–30 min (IM).
Procedural Therapies for PPH
• Uterine massage for atony (external, bimanual)
• Manual extraction of placenta
• D&C/ Suction curettage of the uterus for retained placenta
• Uterine tamponade: Balloon catheter placement (Foley or Bakri balloon, or lap packing) for tamponade, esp lower uterine segment atony
• Uterine compression sutures (eg, B-Lynch) or mattress sutures
• Uterine artery embolization (interv radiol)
Figure 11.3 Management of uterine atony with bimanual massage