FIGURE 43-1 Rates of induction by gestational age among non-Hispanic white singleton livebirths ≥ 37 weeks from 1992 through 2003. (Redrawn from Zhang, 2010, with permission.)
There are contradictory findings concerning maternal demographic factors such as parity, prior postterm birth, socioeconomic class, and age as risks for postterm pregnancy. Olesen and associates (2006) analyzed various risk factors in 3392 participants in the 1998 to 2001 Danish Birth Cohort. Only prepregnancy body mass index (BMI) ≥ 25 and nulliparity were significantly associated with prolonged pregnancy. Caughey (2009) and Arrowsmith (2011) and their coworkers also reported similar associations.
The tendency for some mothers to have repeated postterm births suggests that some prolonged pregnancies are biologically determined. And Mogren and colleagues (1999) reported that prolonged pregnancy recurred across generations in Swedish women. When mother and daughter had a prolonged pregnancy, the risk for the daughter to have a subsequent postterm pregnancy was increased two- to threefold. In another Swedish study, Laursen and associates (2004) found that maternal, but not paternal, genes influenced prolonged pregnancy. As noted in Chapter 21 (p. 426), rare fetal–placental factors that have been reported as predisposing to postterm pregnancy include anencephaly, adrenal hypoplasia, and X-linked placental sulfatase deficiency (MacDonald, 1965).
PERINATAL MORTALITY
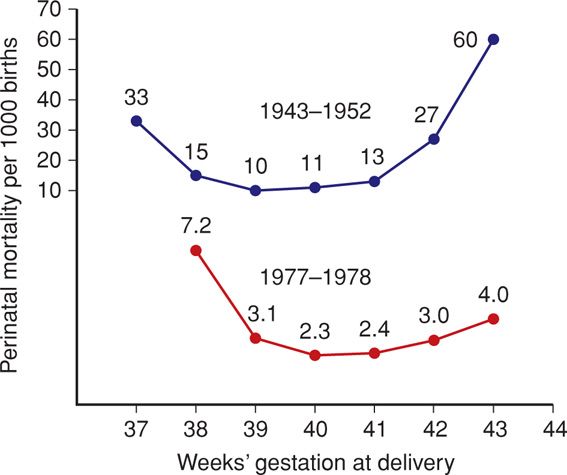
Perinatal mortality rates increase after the expected due date has passed. This is best seen when perinatal mortality rates are analyzed from times before widespread intervention for postterm pregnancies. In two large Swedish studies shown in Figure 43-2, after reaching a nadir at 39 to 40 weeks, the perinatal mortality rate increased as pregnancy exceeded 41 weeks. This trend has also been reported for the United States (MacDorman, 2009). Another study in this country of more than 2.5 million births has similar findings (Cheng, 2008). The major causes of death in these pregnancies included gestational hypertension, prolonged labor with cephalopelvic disproportion, “unexplained anoxia,” and malformations. Similar outcomes were reported by Olesen and colleagues (2003) in 78,022 women with postterm pregnancies delivered before routine labor induction was adopted in Denmark. Moster and associates (2010) found increased rates of cerebral palsy in postterm births, and Yang and coworkers (2010) reported lower intelligence quotient (IQ) scores at age 6.5 years in children born ≥ 42 weeks’ gestation. Conversely, autism was not associated with postterm birth (Gardener, 2011).
FIGURE 43-2 Perinatal mortality rates in late pregnancy according to gestational age in Sweden of all births during 1943–1952 compared with those during 1977–1978. The partially compressed scale is used for convenience in depiction. (Adapted from Bakketeig, 1991, and Lindell, 1956.)
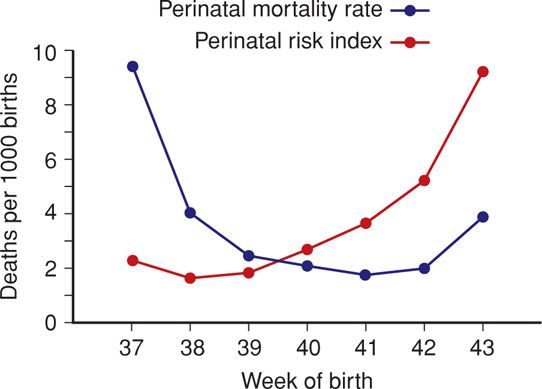
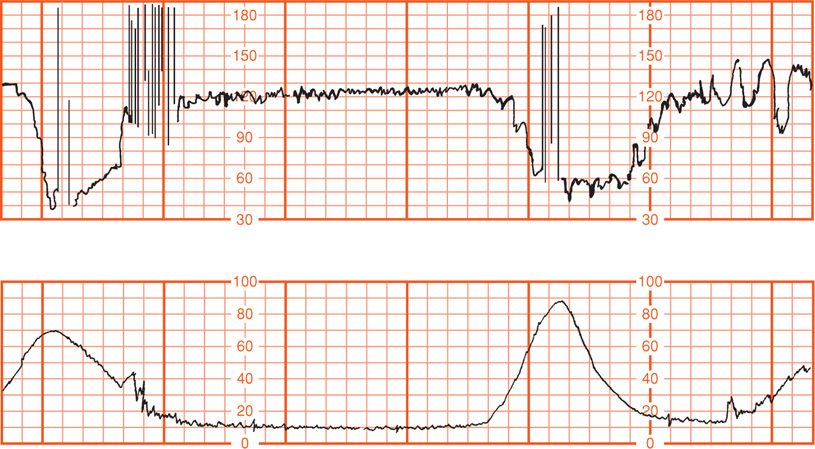
Alexander and colleagues (2000a) reviewed 56,317 consecutive singleton pregnancies delivered at ≥ 40 weeks between 1988 and 1998 at Parkland Hospital. As shown in Table 43-1, labor was induced in 35 percent of pregnancies completing 42 weeks. The rate of cesarean delivery for dystocia and fetal distress was significantly increased at 42 weeks compared with earlier deliveries. More infants of postterm pregnancies were admitted to intensive care units. Importantly, the incidence of neonatal seizures and deaths doubled at 42 weeks. Smith (2001) has challenged analyses such as these because the population at risk for perinatal mortality in a given week consists of all ongoing pregnancies rather than just the births in a given week. Figure 43-3 shows perinatal mortality rates calculated using only births in a given week of gestation from 37 to 43 completed weeks compared with the cumulative probability—the perinatal index—of death when all ongoing pregnancies are included in the denominator. As shown, delivery at 38 weeks had the lowest risk index for perinatal death.
TABLE 43-1. Pregnancy Outcomes in 56,317 Consecutive Singleton Pregnancies Delivered at or Beyond 40 Weeks at Parkland Hospital from 1988 through 1998
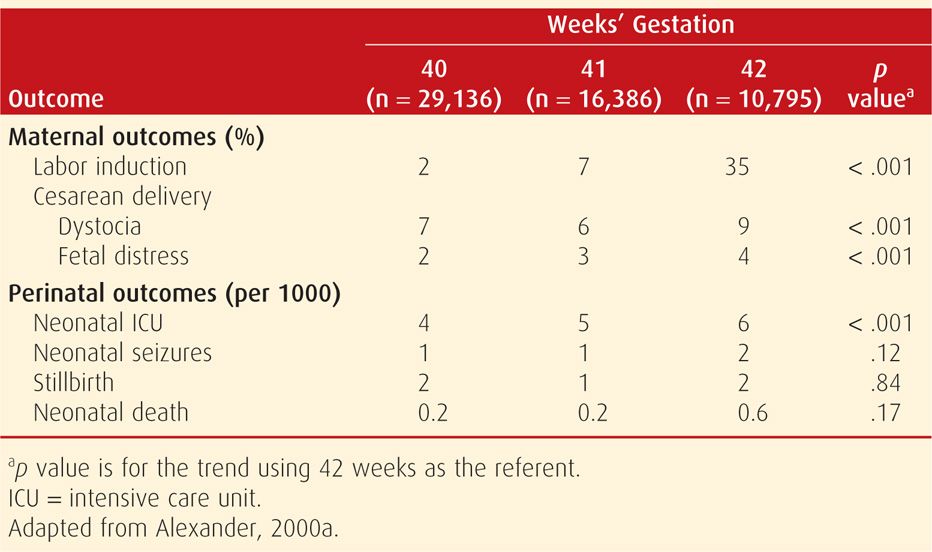
FIGURE 43-3 Perinatal mortality rate and perinatal risk index for births between 37 and 43 weeks in Scotland from 1985 through 1996. The perinatal mortality rate is the number of perinatal deaths with delivery in a given gestational week divided by the total number of births in that week multiplied by 1000. The perinatal risk index is the cumulative probability of perinatal death multiplied by 1000. (Redrawn from Smith, 2001, with permission.)
PATHOPHYSIOLOGY
 Postmaturity Syndrome
Postmaturity Syndrome
The postmature infant presents a unique appearance such as shown in Figure 43-4. Features include wrinkled, patchy, peeling skin; a long, thin body suggesting wasting; and advanced maturity in that the infant is open-eyed, unusually alert, and appears old and worried. Skin wrinkling can be particularly prominent on the palms and soles. The nails are typically long. Most postmature infants are not technically growth restricted because their birthweight seldom falls below the 10th percentile for gestational age. On the other hand, severe growth restriction—which logically must have preceded completion of 42 weeks—may be present.
FIGURE 43-4 Postmaturity syndrome. Infant delivered at 43 weeks’ gestation with thick, viscous meconium coating the desquamating skin. Note the long, thin appearance and wrinkling of the hands.
The incidence of postmaturity syndrome in infants at 41, 42, or 43 weeks, respectively, has not been conclusively determined. In one of the rare contemporary reports that chronicle postmaturity, Shime and colleagues (1984) found this syndrome in approximately 10 percent of pregnancies between 41 and 43 weeks. The incidence increased to 33 percent at 44 weeks. Associated oligohydramnios substantially increases the likelihood of postmaturity. Trimmer and associates (1990) reported that 88 percent of infants were postmature if there was oligohydramnios defined by a sonographic maximal vertical amnionic fluid pocket that measured ≤ 1 cm at 42 weeks.
 Placental Dysfunction
Placental Dysfunction
Clifford (1954) proposed that the skin changes of postmaturity were due to loss of the protective effects of vernix caseosa. He also attributed the postmaturity syndrome to placental senescence, although he did not find placental degeneration histologically. Still, the concept that postmaturity is due to placental insufficiency has persisted despite an absence of morphological or significant quantitative findings (Larsen, 1995; Rushton, 1991). There are findings that placental apoptosis—programmed cell death—was significantly increased at 41 to 42 completed weeks compared with that at 36 to 39 weeks (Smith, 1999). Several proapoptotic genes such as kisspeptin were shown to be upregulated in postterm placental explants compared with the same genes in term placental explants (Torricelli, 2012). The clinical significance of such apoptosis is currently unclear.
Jazayeri and coworkers (1998) investigated cord blood erythropoietin levels in 124 appropriately grown newborns delivered from 37 to 43 weeks. The only known stimulator of erythropoietin is decreased partial oxygen pressure. Thus, they sought to assess whether fetal oxygenation was compromised due to placental aging in postterm pregnancies. All women had an uncomplicated labor and delivery. These investigators reported that cord blood erythropoietin levels were significantly increased in pregnancies reaching 41 weeks or more. Although Apgar scores and acid-base studies were normal, these researchers concluded that there was decreased fetal oxygenation in some postterm gestations.
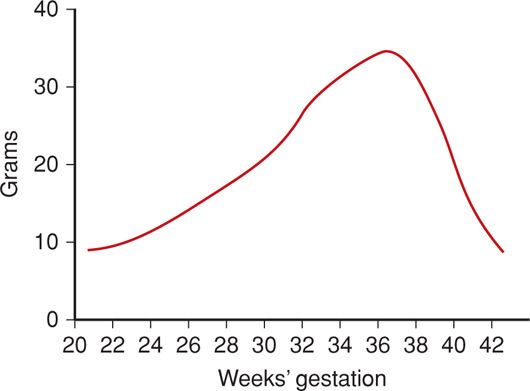
Another scenario is that the postterm fetus may continue to gain weight and thus be unusually large at birth. This at least suggests that placental function is not severely compromised. Indeed, continued fetal growth is the norm—albeit at a slower rate beginning at 37 completed weeks (Fig. 43-5). Nahum and colleagues (1995) confirmed that fetal growth continues until at least 42 weeks, however, Link and associates (2007) showed that umbilical blood flow did not increase concomitantly.
 Fetal Distress and Oligohydramnios
Fetal Distress and Oligohydramnios
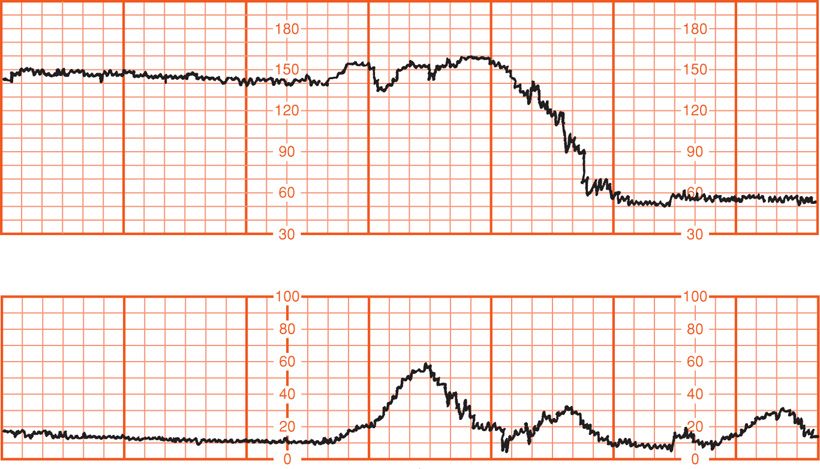
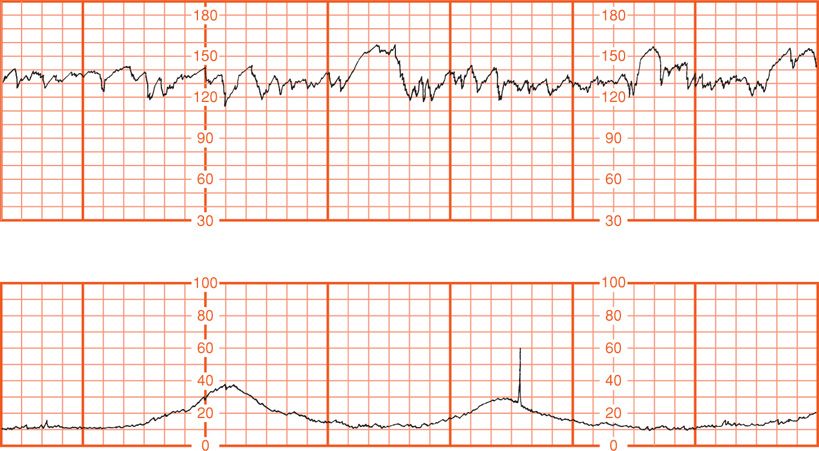
The principal reasons for increased risks to postterm fetuses were described by Leveno and associates (1984). Both antepartum fetal jeopardy and intrapartum fetal distress were found to be the consequence of cord compression associated with oligohydramnios. In their analysis of 727 postterm pregnancies, intrapartum fetal distress detected with electronic monitoring was not associated with late decelerations characteristic of uteroplacental insufficiency. Instead, one or more prolonged decelerations such as shown in Figure 43-6 preceded three fourths of emergency cesarean deliveries for nonreassuring fetal heart rate tracings. In all but two cases, there were also variable decelerations (Fig. 43-7). Another common fetal heart rate pattern, although not ominous by itself, was the saltatory baseline shown in Figure 43-8. As described in Chapter 24 (p. 484), these findings are consistent with cord occlusion as the proximate cause of the nonreassuring tracings. Other correlates included oligohydramnios and viscous meconium. Schaffer and colleagues (2005) implicated a nuchal cord in abnormal intrapartum fetal heart rate patterns, meconium, and compromised newborn condition in prolonged pregnancies.
FIGURE 43-6 Prolonged fetal heart rate deceleration before emergency cesarean delivery in a postterm pregnancy with oligohydramnios. (Redrawn from Leveno, 1984, with permission.)
FIGURE 43-7 Severe—less than 70 bpm for 60 seconds or longer—variable decelerations in a postterm pregnancy with oligohydramnios. (Redrawn from Leveno, 1984, with permission.)
FIGURE 43-8 Saltatory baseline fetal heart rate showing oscillations exceeding 20 bpm and associated with oligohydramnios in a postterm pregnancy. (Redrawn from Leveno, 1984, with permission.)
The volume of amnionic fluid normally continues to decrease after 38 weeks and may become problematic (Fig. 11-1, p. 233). Moreover, meconium release into an already reduced amnionic fluid volume results in thick, viscous meconium that may cause meconium aspiration syndrome (Chap. 33, p. 637).
Trimmer and coworkers (1990) sonographically measured hourly fetal urine production using sequential bladder volume measurements in 38 pregnancies of ≥ 42 weeks. Diminished urine production was found to be associated with oligohydramnios. They hypothesized that decreased fetal urine flow was likely the result of preexisting oligohydramnios that limited fetal swallowing. Oz and associates (2002), using Doppler waveforms, concluded that fetal renal blood flow is reduced in those postterm pregnancies complicated by oligohydramnios. The study mentioned above, by Link and associates (2007), showed that umbilical blood flow did not increase past term.
 Fetal-Growth Restriction
Fetal-Growth Restriction
It was not until the late 1990s that the clinical significance of fetal-growth restriction in the otherwise uncomplicated pregnancy became more fully appreciated. Divon (1998) and Clausson (1999) and their coworkers analyzed births between 1991 and 1995 in the National Swedish Medical Birth Registry. As shown in Table 43-2, stillbirths were more common among growth-restricted infants who were delivered after 42 weeks. Indeed, a third of postterm stillborn infants were growth restricted. During this time in Sweden, labor induction and antenatal fetal testing usually commenced at 42 weeks. In a study from Parkland Hospital, Alexander and colleagues (2000d) analyzed outcomes for 355 infants who were ≥ 42 weeks and whose birthweights were < 3rd percentile. They compared these with outcomes of 14,520 similarly aged infants above the 3rd percentile and found that morbidity and mortality rates were significantly increased in the growth-restricted infants. Notably, a fourth of all stillbirths associated with prolonged pregnancy were in this comparatively small number of growth-restricted infants.
TABLE 43-2. Effects of Fetal-Growth Restriction by Gestational Age on Stillbirth Rates in 537,029 Swedish Women Delivered before and after 42 Weeks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree