9 Postoperative/Posttraumatic Changes Synonyms: liponecrosis microcystica calcificata. Fat necrosis is a localized area of dead adipose tissue characterized by morphological changes resulting from progressive enzymatic degradation. Leukocytic and histiocytic infiltrates are encountered in new areas of fat necrosis. Gradually, well-vascularized granulation tissue develops. The transformation into scar tissue is usually complete in a matter of weeks. The coalescence of liquefied adipose tissue can lead to formation of so-called oil cysts. Signal intensity equivalent to that of parenchyma (Fig. 9.1b). Oil cysts present as rounded lesions with a hyperintense (fat-equivalent) signal (Figs. 9.2b, 9.3b). Possible signal loss due to macrocalcifications (Figs. 9.4b, 9.5a). A fresh fat necrosis presents as an ill-defined, hyperintense area (Fig. 9.1c). Later, when oil cysts are present, round lesions with central, fat-equivalent signal intensity are seen (signal-free in IR T2w sequence due to fat suppression) (Figs. 9.3c, 9.4c). Otherwise no characteristic changes after 6 months. In the early phase when capillary sprouting takes place (first 6 months after trauma/surgery), fat necrosis presents as a localized, sometimes well-defined (Fig. 9.1a,d), but usually ill-defined (Fig. 9.2a,d) area with increased CM uptake (Fig. 9.1a,d). Initial signal enhancement is usually moderate (Fig. 9.1e). The postinitial signal increase is typically persistent or displays a plateau. In the late phase (> 6 months) there is usually no more contrast enhancement (Figs. 9.3a, d, 9.5b). Mild enhancement may be seen when there is an additional inflammatory component (Fig. 9.4d).
Fat Necrosis
 A fresh fat necrosis can be very difficult to differentiate from breast cancer, i.e., breast cancer recurrence in breast MRI, as well as in mammography and breast ultrasound.
A fresh fat necrosis can be very difficult to differentiate from breast cancer, i.e., breast cancer recurrence in breast MRI, as well as in mammography and breast ultrasound.
 MR Mammography: Fat Necrosis
MR Mammography: Fat Necrosis
T1-Weighted Sequence (Precontrast)
T2-Weighted Sequence
T1-Weighted Sequence (Contrast Enhanced)
Fat necrosis: General information | |
Etiology: | Posttraumatic (e.g., injury, surgery, needle biopsy), inflammation, foreign body reaction (e.g., silicone, parafin). |
Risk of malignant transformation: | No increased risk. |
Findings | |
Clinical: | Usually occult. Large findings may present as a mass or thickening. |
Mammography: | Round, oval, or irregular mass lesion. Homogeneous and hyperdense. No specific findings. New fat necrosis: ill-defined area of increased density. Older fat necrosis: improving demarcation of density. Oil cysts: rounded, centrally radiolucent lesions possibly containing bizarre or rim calcifications. |
Ultrasonography: | Great variability: from round, well-defined lesions to irregularly shaped lesions showing echo texture typical of malignancy. |
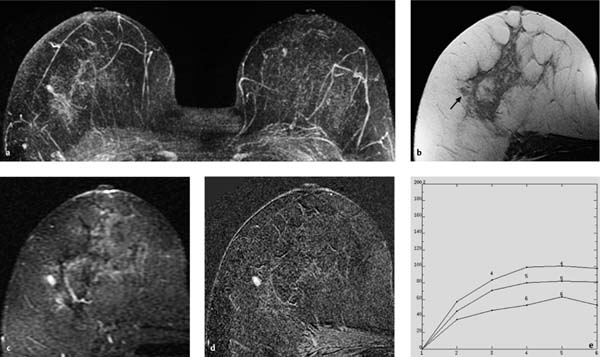
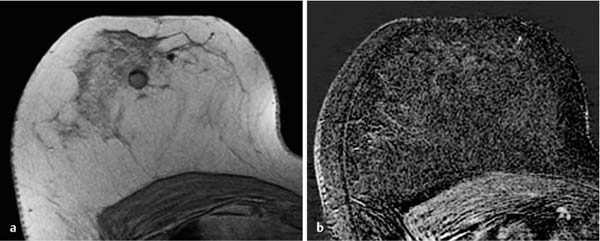
Fig. 9.1a–e Fresh fat necrosis.
a Subtraction MIP: oval, hypervascularized focus in the lateral aspect of the right breast.
b T1w precontrast slice image: corresponding oval focus (4 mm, arrow) within the lipomatous breast tissue lateral to the parenchymal body.
c IR T2w slice image: lesion displays a high signal intensity, i.e., water content.
d Early subtraction slice image: strong contrast enhancement.
e Unspecific TIC.
Percutaneous biopsy-proven diagnosis.
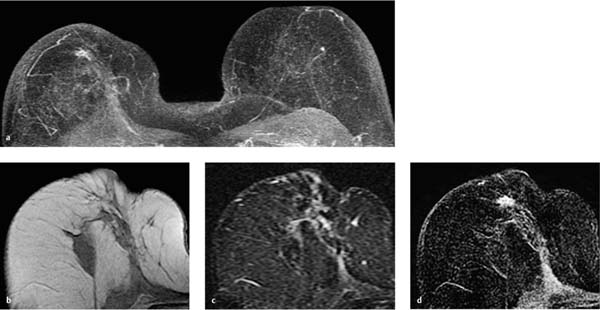
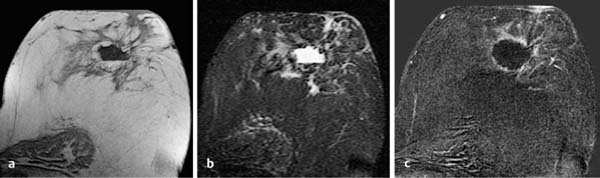
Fig. 9.2a–d Fat necrosis: several weeks after surgery.
a Subtraction MIP: irregular, hypervascularized lesion in the scar tissue area of the right breast, 8 weeks after breast-conserving therapy.
b T1w precontrast slice image: morphologic distortion in the right breast due to scar tissue. Slight signal increase in fat necrosis.
c IR T2w slice image (fat saturated): mild reactive edematous changes in scar tissue area.
d Early subtraction slice image: rim-enhancement around discrete central liquid inclusions.
a Subtraction MIP: unremarkable findings 2 years after breast-conserving therapy.
b T1w precontrast slice image: localized area of scar tissue with oval, fat-containing area (arrow). Skin thickening.
c IR T2w slice image (fat saturated): reactive edematous changes of cutaneous and subcutaneous areas after radiation therapy. Complete signal suppression of oval fat necrosis.
d Early subtraction slice image: fat necrosis displays no contrast enhancement.
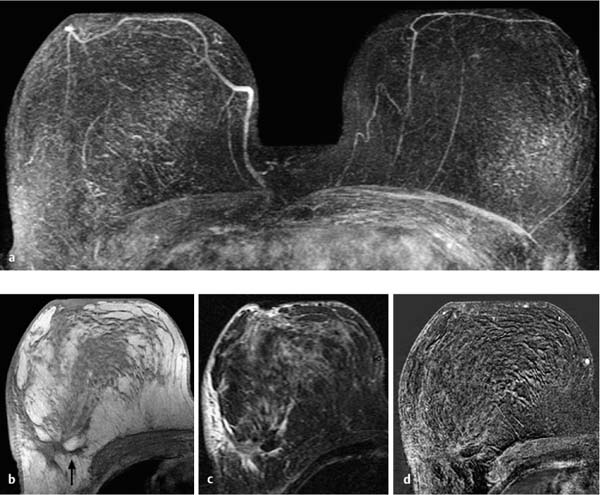
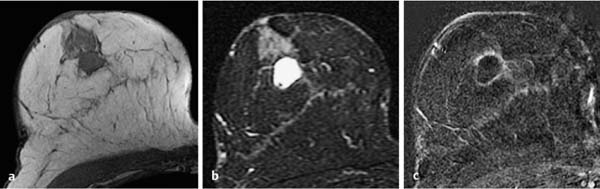
Fig. 9.4a–d Oil cyst.
a Subtraction MIP: unremarkable findings several years after diagnostic excision.
b T1w precontrast slice image: round lesion with fat-equivalent internal signal and peripheral punctate signal extinction due to calcification.
c IR T2w slice image (fat saturated): mildly elevated signal intensity (water content) of parenchyma. Signal suppression of the lesion’s internal liquefied fat.
d Early subtraction slice image: very discrete rim-enhancement.
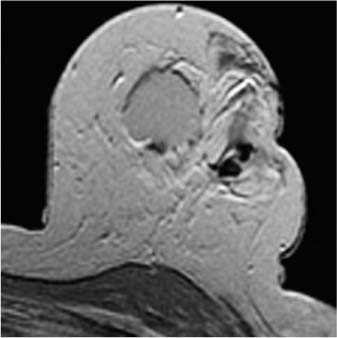
Fig. 9.5a, b Oil cyst.
a T1w precontrast slice image: round oil cyst with slightly elevated internal signal and peripheral signal extinction due to calcification.
b Early subtraction slice image: fat necrosis displays no contrast enhancement.
Seroma
A seroma is a localized collection of wound serum in the tissues, for example after surgery.
 MR Mammography: Seroma
MR Mammography: Seroma
T1-Weighted Sequence (Precontrast)
More or less circumscribed area usually demonstrating a slightly hypointense signal in comparison with surrounding parenchyma (Fig. 9.7a). Occasionally cushionlike or villuslike internal structures along or stemming from internal seroma wall (Fig. 9.6a).
T2-Weighted Sequence
Hyperintense fluid within seroma (Figs. 9.6b, 9.7b).
T1-Weighted Sequence (Contrast Enhanced)
Immediately after surgery CM uptake is usually slight, after several days it is stronger in areas immediately surrounding the seroma (Figs. 9.6c, 9.7c).
Seroma: General information | |
Age peak: | No age dependence. Postoperative. |
Risk of malignant transformation: | No increased risk. |
Findings | |
Clinical: | Small seromas are clinically occult. Large findings may present as an elastic mass. |
Mammography: | Seromas within dense parenchymal areas are often mammographically occult. Within lipomatous areas: round, hyperdense mass. |
Ultrasonography: | Well-circumscribed, liquid-.lled mass (similar to a cyst). Occasionally villuslike, noncystic internal structures on the seroma wall. |
Seroma is a frequent postoperative finding without major clinical significance. Large seromas may be an indication for fine-needle aspiration. | |
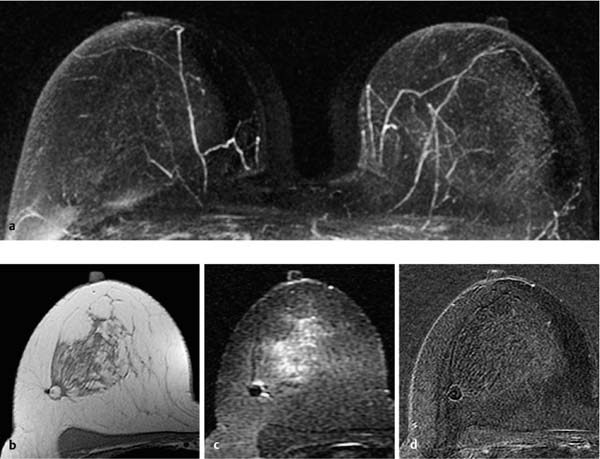
Fig. 9.6a–c Postoperative seroma.
a T1w precontrast slice image: round lesion with surrounding capsule and polypous structures adhering to the internal wall.
b IR T2w slice image: high signal intensity (water content) within the seroma.
c Early subtraction slice image: discrete enhancement of seroma wall. Polypous structures display no perfusion.
Fig. 9.7a–c Postoperative seroma.
a T1w precontrast slice image: lobulated, hypointense lesion with surrounding capsule.
b IR T2w slice image: high signal intensity (water content) within the seroma.
c Early subtraction slice image: discrete enhancement of seroma wall.
Hematoma
A breast hematoma is an intramammary hemorrhage, for example, due to intervention or surgery.
 MR Mammography: Hematoma
MR Mammography: Hematoma
T1-Weighted Sequence (Precontrast)
A hematoma shows a typical signal intensity, as in other regions of the body, depending on the time elapsed since its development. A fresh hemorrhage demonstrates a homogeneous high signal intensity (Fig. 9.8). A subacute hematoma shows a low internal signal with a hyperintense peripheral ring (Fig. 9.9). An old hematoma may be hyperintense (Fig. 9.10a).
T2-Weighted Sequence
A fresh hematoma displays a homogeneous low signal intensity. With increasing age, a hypointense peripheral ring develops (Fig. 9.10b).
T1-Weighted Sequence (Contrast Enhanced)
Diffuse reactive CM uptake occurs in the parenchyma surrounding a subacute hematoma. With increasing age, the reactive changes decrease and usually disappear completely (Fig. 9.10c).
Hematoma: General information | |
Incidence: | Often after intervention. Occasionally after surgery. Rare after other trauma. |
Risk of malignant transformation: | No increased risk. |
Findings | |
Clinical: | Small hematomas are clinically occult. Large findings may present as a palpable mass. Later visible skin pigmentation. |
Mammography: | Hematomas within dense parenchymal areas are often mammographically occult. Within lipomatous areas: round, hyperdense mass. |
Ultrasonography: | Well-circumscribed, hypoechoic structure. |
Incidental finding without major clinical significance. Large hematomas may be an indication for fine-needle aspiration. | |
Fig. 9.8 Acute hematoma. Hyperintense, fat-equivalent lesion in the T1w precontrast image immediately after percutaneous vacuumassisted biopsy.