91 Pneumonia and Respiratory Infections
Etiology and Pathogenesis
Microbiology
The common causes of CAP in healthy children in the developed world vary by age group, although an extensive number of pathogens can cause CAP (Table 91-1). Respiratory viruses such as respiratory syncytial virus (RSV); influenza A and B; parainfluenza 1, 2, and 3; adenovirus; and human metapneumovirus (hMPV) can be identified in up to half of patients admitted to the hospital for CAP. These viral pathogens may be identified alone or as part of a co-infection with bacteria. First described in 2001, hMPV, similar to RSV infection in young children, causes a spectrum of respiratory disease ranging from mild bronchiolitis to severe pneumonia.
Table 91-1 Common Bacterial and Viral Causes of Community-Acquired Pneumonia by Age in Healthy Children in the Developed World
| ≤3 Months Old | 3 Months to 5 Years Old | ≥5 Years Old |
|---|---|---|
| Bacteria | Bacteria | Bacteria |
| Group B streptococcus | Streptococcus pneumoniae | Streptococcus pneumoniae |
| Enteric gram-negative bacilli | Mycoplasma pneumoniae | Mycoplasma pneumoniae |
| Streptococcus pneumoniae | Chlamydophila pneumoniae* | Chlamydophila pneumoniae* |
| Bordetella pertussis | Staphylococcus aureus | Staphylococcus aureus |
| Chlamydia trachomatis Staphylococcus aureus | Haemophilus influenzae (nontypable) | |
| Lower Respiratory Viruses | Lower Respiratory Viruses | Lower Respiratory Viruses |
| Respiratory syncytial virus | Respiratory syncytial virus | Influenza A and B |
| Influenza A and B | Influenza A and B | |
| Parainfluenza viruses 1, 2, 3 | Parainfluenza viruses 1, 2, 3 | |
| Human metapneumovirus | Human metapneumovirus | |
| Rhinovirus | Rhinovirus | |
| Adenovirus | Adenovirus | |
| Bocavirus | Bocavirus | |
| Coronaviruses | Coronaviruses |
* Formerly Chlamydia pneumoniae.
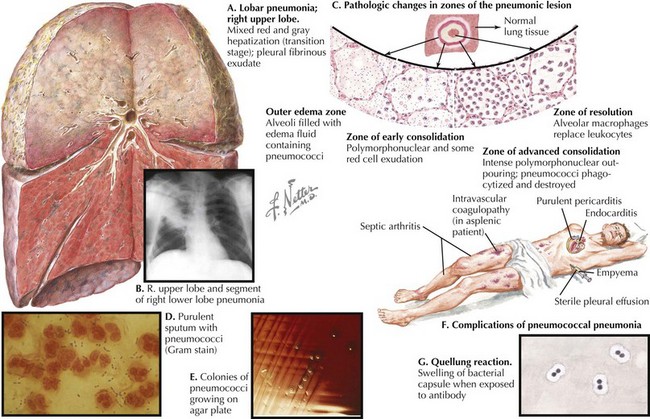
Streptococcus pneumoniae is the most common bacterial cause of childhood CAP (Figure 91-1). Randomized trials of the heptavalent pneumococcal conjugate vaccine (PCV7) demonstrated that the incidence of radiographically confirmed pneumonia was reduced by 20% in vaccine recipients compared with placebo recipients, suggesting that S. pneumoniae causes at least 20% of CAP cases. Postlicensure epidemiologic studies have shown a 39% decrease in all-cause pneumonia hospitalizations in children younger than 2 years of age but nonsignificant decreases in older children. Thus, the significant role of pneumococcus as a cause of childhood CAP drives the choice of empiric antibiotic therapy for younger children.
Pathogenesis
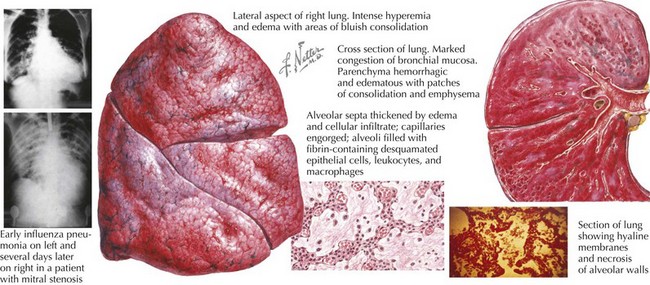
Viral illness alone, such as influenza, can cause severe and necrotizing pneumonia (Figure 91-2). Preceding viral illness may play a part in the pathogenesis of bacterial pneumonia. One study demonstrated that rates of invasive pneumococcal disease each winter season rose in close association with respiratory viral illness diagnoses (RSV, influenza, and hMPV), suggesting that the respiratory damage caused by viral respiratory illness may allow for subsequent bacterial pneumonia. Such data do not prove the direct causation of invasive bacterial pneumonia as a consequence of viral respiratory infection, however. Likewise, a randomized trial of children receiving a pneumococcal vaccine found fewer admissions for both pneumococcal pneumonia and hMPV pneumonia among vaccine recipients compared with placebo recipients, suggesting that hospitalizations for hMPV may involve co-infection with pneumococcus.
Clinical Presentation and Differential Diagnosis
The differential diagnosis of lower respiratory infection includes pulmonary anatomic abnormalities, foreign bodies and chemical irritants, autoimmune diseases, and malignancies, among others (Box 91-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree