52 Platelet Disorders
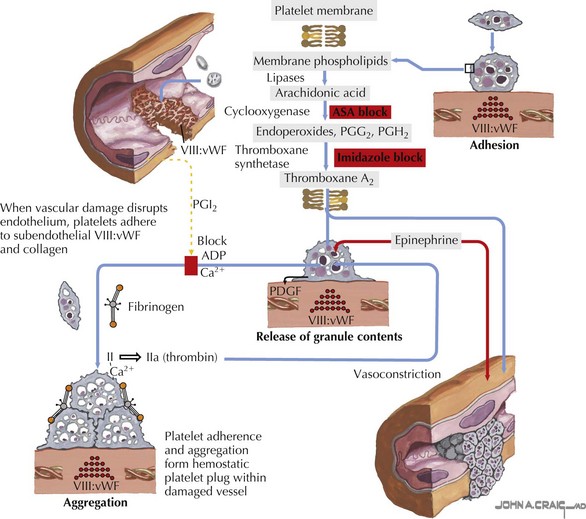
Platelets are small anucleate cell particles (5-7 µL in volume) that play a critical role in primary hemostasis. At the time of vascular injury, platelets rush to the site of vascular damage and adhere to the exposed collagen, forming a temporary platelet plug to prevent continued bleeding. The platelets are then activated and undergo changes in their shape and structure. These changes allow the platelets to bind to fibrinogen and aggregate with one another, thus propagating the platelet plug. Activation of platelets also causes secretion of the chemicals contained in the platelet storage granules. These chemicals recruit new platelets and contain many compounds needed to continue primary hemostasis and activate secondary hemostasis (Figure 52-1).
Etiology and Pathogenesis
Acquired Platelet Disorders
Acquired platelet disorders are far more common than congenital platelet disorders. The most common reason for acquired thrombocytopenia or an acquired platelet abnormality is drug exposure. Dozens of medications can cause thrombocytopenia or abnormalities in platelet function. These medications can act by inhibiting bone marrow production of platelets or activating or creating antibodies to platelets, or they can have a direct toxic effect on platelets. Refer to Table 52-1 for a list of some of the common medications resulting in thrombocytopenia and platelet function abnormalities. Heparin-induced thrombocytopenia (HIT) is a special case and is discussed again later this chapter.
Table 52-1 Common Medications Resulting in Thrombocytopenia or Platelet Function Abnormalities
| Drugs Associated with Thrombocytopenia | Drugs Associated with Abnormal Platelet Function |
|---|---|
Antibiotics
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|