NORMAL PLACENTA
Placental abnormalities are better understood with knowledge of placental implantation, development, and anatomy presented in Chapter 5 (p. 88). At term, the “typical” placenta weighs 470 g, is round to oval with a 22-cm diameter, and has a central thickness of 2.5 cm (Benirschke, 2012). It is composed of a placental disc, extraplacental membranes, and three-vessel umbilical cord. The maternal surface is the basal plate, which is divided by clefts into portions—termed cotyledons. These clefts mark the site of internal septa, which extend into the intervillous space. The fetal surface is the chorionic plate, into which the umbilical cord inserts, typically in the center. Large fetal vessels that originate from the cord vessels then spread and branch across the chorionic plate before entering stem villi of the placenta parenchyma. In tracing these, fetal arteries almost invariably cross over veins. The chorionic plate and its vessels are covered by thin amnion, which can be easily peeled away from a postdelivery specimen.
Sonographically, the normal placenta is homogenous and 2 to 4 cm thick, lies against the myometrium, and indents into the amnionic sac. The retroplacental space is a hypoechoic area that separates the myometrium from the placenta’s basal plate and measures less than 1 to 2 cm. During prenatal sonographic examinations, placental location and relationship to the internal cervical os are recorded. The umbilical cord is also imaged, its fetal and placental insertion sites examined, and its vessels counted.
Many placental lesions can be identified grossly or sonographically, but many abnormalities require histopathological examination for clarification. A detailed description of these is beyond the scope of this chapter, and interested readers are referred to textbooks by Benirschke (2012), Fox (2007), Faye-Petersen (2006), and their colleagues.
ABNORMALITIES OF THE PLACENTA
 Shape and Size
Shape and Size
In contrast to the normal architecture described earlier, placentas may infrequently form as separate, nearly equally sized discs. This is a bilobate placenta, but is also known as bipartite placenta or placenta duplex. In these, the cord inserts between the two placental lobes—either into a connecting chorionic bridge or into intervening membranes.
A placenta containing three or more equally sized lobes is rare and termed multilobate. However, more frequently, one or more small accessory lobes—succenturiate lobes—may develop in the membranes at a distance from the main placenta (Fig. 6-1). These lobes have vessels that course through the membranes. If these vessels overlie the cervix to create a vasa previa, they can cause dangerous fetal hemorrhage if torn (p. 123). An accessory lobe may also be retained in the uterus after delivery and cause postpartum uterine atony and hemorrhage.
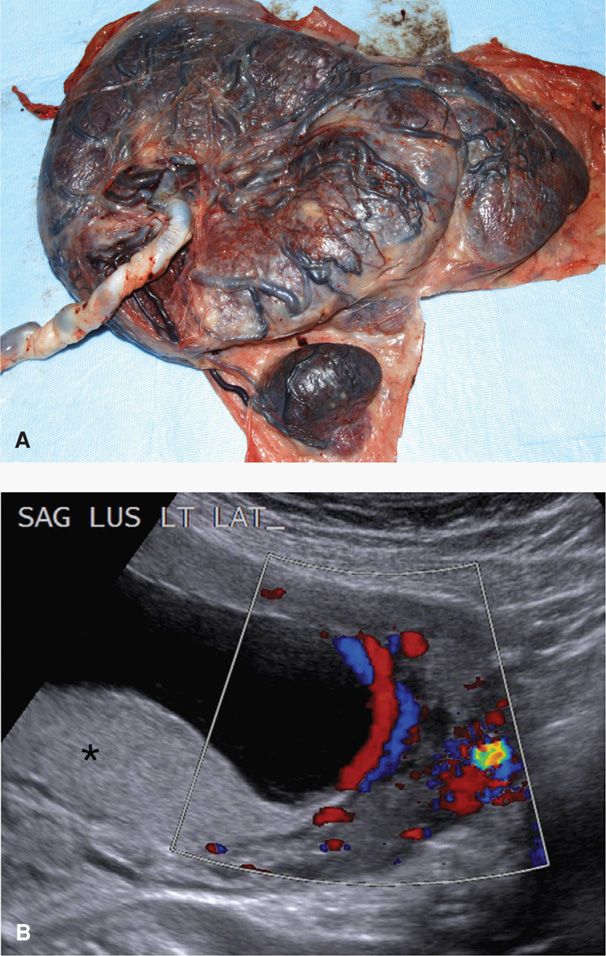
FIGURE 6-1 Succenturiate lobe. A. Vessels extend from the main placental disk to supply the small round succenturiate lobe located beneath it. (Photograph contributed by Dr. Jaya George.) B. Sonographic imaging with color Doppler shows the main placental disk implanted posteriorly (asterisk). The succenturiate lobe is located on the anterior uterine wall across the amnionic cavity. Vessels are identified as the long red and blue crossing tubular structures that travel within the membranes to connect these two portions of placenta.
Rarely, the portion of fetal membranes covered by functioning villi varies from the norm. With placenta membranacea, all or nearly all of the membranes are covered with villi. This placentation may occasionally give rise to serious hemorrhage because of associated placenta previa or accreta (Greenberg, 1991). A ring-shaped placenta may be a variant of placenta membranacea. The placenta is annular, and a partial or complete ring of placental tissue is present. These abnormalities appear to be associated with a greater likelihood of antepartum and postpartum bleeding and fetal-growth restriction (Faye-Petersen, 2006). With placenta fenestrata, the central portion of a placental disc is missing. In some instances there is an actual hole in the placenta, but more often, the defect involves only villous tissue, and the chorionic plate remains intact. Clinically, it may erroneously prompt a search for a retained placental cotyledon.
During pregnancy, the normal placenta increases its thickness at a rate of approximately 1 mm per week. Although not measured as a component of routine sonographic evaluation, this thickness typically does not exceed 40 mm (Hoddick, 1985). Placentomegaly defines those thicker than 40 mm and commonly results from striking villous enlargement. This may be secondary to maternal diabetes or severe maternal anemia, or to fetal hydrops or infection caused by syphilis, toxoplasmosis, or cytomegalovirus. Less commonly, villi are enlarged and edematous and fetal parts are present, such as in cases of partial mole or a complete mole that coexists with a normal twin (Chap. 20, p. 398). Cystic vesicles are also seen with placental mesenchymal dysplasia. Vesicles in this rare condition correspond to enlarged stem villi, but unlike molar pregnancy, there is not excessive trophoblast proliferation (Woo, 2011). And in some cases, rather than villous enlargement, placentomegaly may result from collections of blood or fibrin. Examples of this that are subsequently discussed on page 119 include massive perivillous fibrin deposition, intervillous or subchorionic thromboses, and large retroplacental hematomas.
 Extrachorial Placentation
Extrachorial Placentation
The chorionic plate normally extends to the periphery of the placenta and has a diameter similar to that of the basal plate. With extrachorial placentation, however, the chorionic plate fails to extend to this periphery and leads to a chorionic plate that is smaller than the basal plate (Fig. 6-2). In a circummarginate placenta, fibrin and old hemorrhage lie between the placenta and the overlying amniochorion. In contrast, with a circumvallate placenta the peripheral chorion is a thickened, opaque, gray-white circular ridge composed of a double fold of chorion and amnion. Sonographically, the double fold can be seen as a thick, linear band of echoes extending from one placental edge to the other. On cross section, it appears as a “shelf.” This is important clinically because its location may help to differentiate this shelf from amnionic bands and amnionic sheets, which are described subsequently.
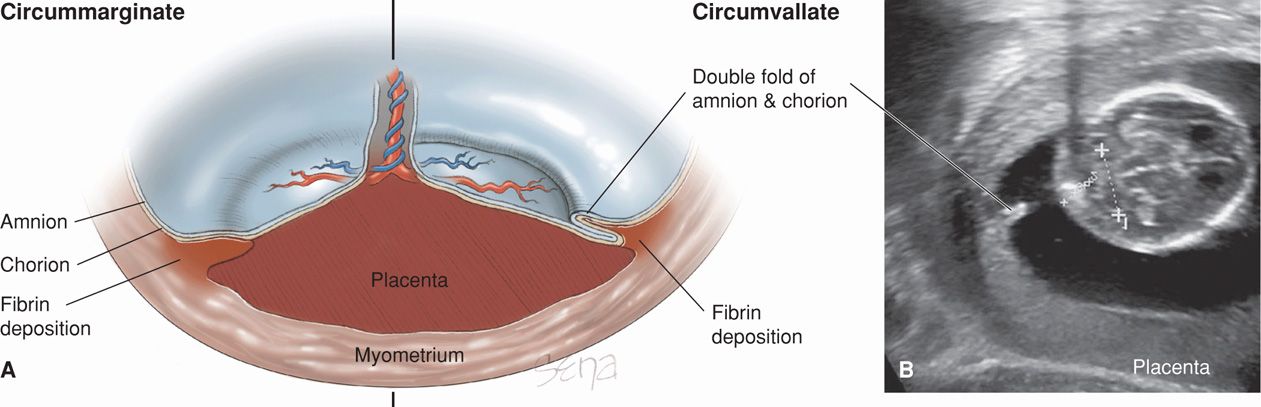
FIGURE 6-2 A. In this illustration, circummarginate (left) and circumvallate (right) varieties of extrachorial placentation are shown. A circummarginate placenta is covered by a single layer of amniochorion. B. This transabdominal gray-scale sonographic image shows a circumvallate placenta. The double fold of amnion and chorion creates a broad, opaque white ring and ridge on the fetal surface.
Clinically, most pregnancies with an extrachorial placenta have normal outcomes. In observational studies in which the diagnosis was made by placental examination, circumvallate placenta was associated with increased risk for antepartum bleeding and preterm birth (Lademacher, 1981; Suzuki, 2008a). In a prospective sonographic investigation, however, Shen and colleagues (2007a) found a circumvallate placenta—described as a placental “shelf”—in more than 10 percent of early second-trimester pregnancies. Importantly, they reported that these were transient and benign.
 Placenta Accreta, Increta, and Percreta
Placenta Accreta, Increta, and Percreta
These clinically important placental abnormalities develop when trophoblast invades the myometrium to varying depths to cause abnormal adherence. They are much more likely when there is placenta previa or when the placenta implants over a prior uterine incision or perforation. As discussed further in Chapter 41 (p. 804), torrential hemorrhage is a frequent complication.
 Circulatory Disturbances
Circulatory Disturbances
These are clinically important syndromes, and in most cases, the placenta is a target organ of maternal disease. Functionally, placental perfusion disorders can be grouped into: (1) those in which there is disrupted maternal blood flow to or within the intervillous space and (2) those with disturbed fetal blood flow through the villi. These lesions are frequently identified in the normal, mature placenta. Although they can limit maximal placental blood flow, placental functional reserve prevents harm in most cases. Indeed, some estimate that up to 30 percent of placental villi can be lost without untoward fetal effects (Fox, 2007). If extensive, however, these lesions can profoundly limit fetal growth.
Placental lesions that cause abnormal perfusion are frequently seen grossly or sonographically, whereas smaller lesions are seen only by microscopic examination. Sonographically, many of these lesions, such as subchorionic fibrin deposition, perivillous fibrin deposition, and intervillous thrombosis, may be appear as focal sonolucencies within the placenta. Importantly, in the absence of maternal or fetal complications, isolated placental sonolucencies are considered incidental findings.
Maternal Blood Flow Disruption
Subchorionic Fibrin Deposition. These are caused by slowing of maternal blood flow within the intervillous space with subsequent fibrin deposition. Blood stasis specifically occurs in the subchorionic area, and lesions that develop are commonly seen as white or yellow firm plaques on the fetal surface.
Perivillous Fibrin Deposition. Maternal blood flow stasis around an individual villus results in fibrin deposition and can lead to diminished villous oxygenation and syncytiotrophoblastic necrosis (Fig. 6-3). Within limits, these grossly visible small yellow-white placental nodules are considered to be normal placental aging.
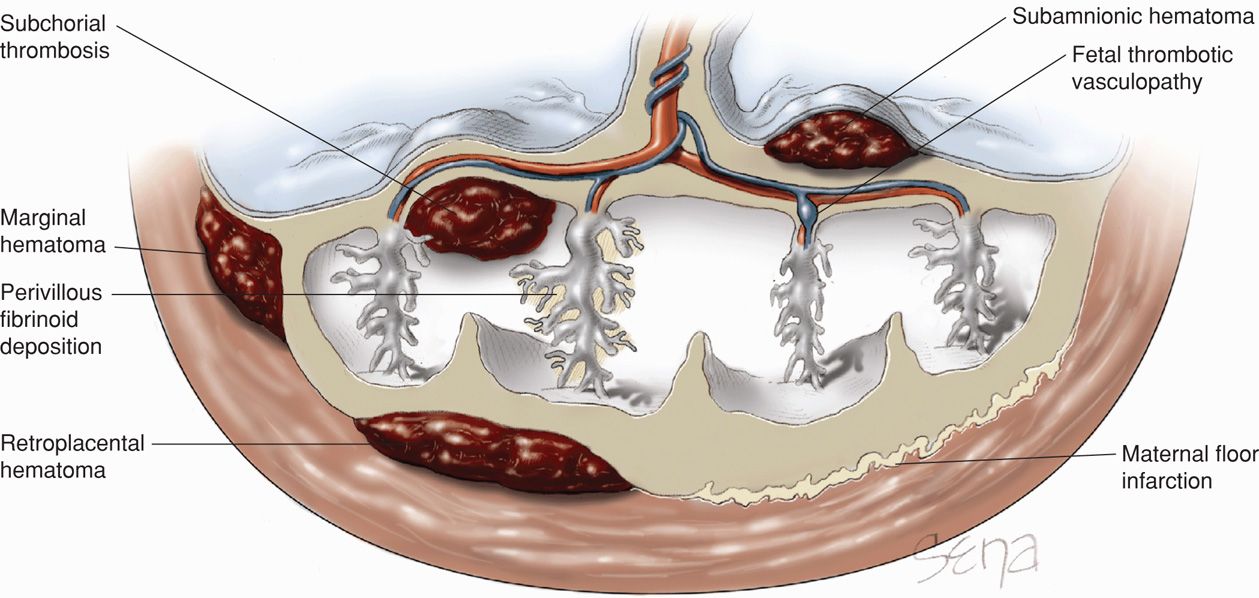
FIGURE 6-3 Potential sites of maternal- and fetal-related placental circulatory disturbances. (Adapted from Faye-Petersen, 2006.)
Maternal Floor Infarction. This extreme variant of perivillous fibrinoid deposition is a dense fibrinoid layer within the placental basal plate and is erroneously termed an infarction. The lesion has a thick, white, firm, corrugated surface that impedes normal maternal blood flow into the intervillous space. These lesions are associated with miscarriage, fetal-growth restriction, preterm delivery, and stillbirths (Andres, 1990; Mandsager, 1994). These adverse outcomes occasionally recur in subsequent pregnancies. Their etiopathogenesis is not well defined, but some cases are associated with lupus anticoagulant (Sebire, 2002, 2003). Although unsettled, other cases may be associated with maternal thrombophilias (Gogia, 2008; Katz, 2002). These lesions are not reliably imaged with prenatal sonography, but they may create a thicker basal plate.
Intervillous Thrombus. This is a collection of coagulated maternal blood normally found in the intervillous space mixed with fetal blood from a break in a villus. Grossly, these round or oval collections vary in size up to several centimeters. They appear red if recent or white-yellow if older, and they develop at any placental depth. Intervillous thrombi are common and typically not associated with adverse fetal sequelae. Because there is potential for a communication between maternal and fetal circulations, they can cause elevated maternal serum alpha-fetoprotein levels (Salafia, 1988).
Infarction. Chorionic villi themselves receive oxygen solely from maternal circulation supplied to the intervillous space. Any uteroplacental disease that diminishes or obstructs this supply can result in infarction of individual villus. These are common lesions in mature placentas and are benign in limited numbers. If they are numerous, however, placental insufficiency can develop. When they are thick, centrally located, and randomly distributed, they may be associated with preeclampsia or lupus anticoagulant.
Hematoma. The maternal-placental-fetal unit can develop a number of hematoma types as depicted in Figure 6-3. These include: (1) retroplacental hematoma—between the placenta and its adjacent decidua; (2) marginal hematoma—between the chorion and decidua at the placental periphery—known clinically as subchorionic hemorrhage; (3) subchorial thrombosis—also known as Breus mole—along the roof of the intervillous space and beneath the chorionic plate; and (4) subamnionic hematoma—these are of fetal vessel origin and found beneath the amnion but above the chorionic plate.
Sonographically, these hematomas may resemble a crescent-shaped fluid collection that is hyperechoic to isoechoic in the first week after hemorrhage, hypoechoic at 1 to 2 weeks, and finally, anechoic after 2 weeks. Most subchorionic hematomas visible sonographically are fairly small and of no clinical consequence. Extensive retroplacental, marginal, and subchorial collections have been associated with higher rates of miscarriage, placental abruption, fetal-growth restriction, preterm delivery, and adherent placenta (Ball, 1996; Madu, 2006; Nagy, 2003). In essence, placental abruption is a large clinically significant retroplacental hematoma (Chap. 41, p. 793)
Fetal Blood Flow Disruption
Placental lesions that arise from fetal circulatory disturbances are also depicted in Figure 6-3.
Fetal Thrombotic Vasculopathy. Deoxygenated fetal blood flows from the two umbilical arteries into arteries within the chorionic plate that divide and send branches out across the placental surface. These eventually supply individual stem villi, and their thrombosis will obstruct fetal blood flow. Distal to the obstruction, affected portions of the villus become infarcted and nonfunctional. Thrombi in limited numbers are normally found in mature placentas, but these may be clinically significant if many villi become infarcted.
Subamnionic Hematoma. As indicated earlier, these hematomas lie between the placenta and amnion. They most often are acute events during third-stage labor when cord traction ruptures a vessel near the cord insertion. Chronic lesions may cause fetomaternal hemorrhage or fetal-growth restriction (Deans, 1998). They also may be confused with other placental masses such as chorioangioma, which is discussed subsequently (Sepulveda, 2000; Van Den Bosch, 2000; Volpe, 2008). In most cases, Doppler interrogation will show absence of internal blood flow that permits differentiation of hematomas from other placental masses.
 Placental Calcification
Placental Calcification
Calcium salts may be deposited throughout the placenta, but are most common on the basal plate. Calcification accrues with advancing gestation and is associated with nulliparity, smoking, higher socioeconomic status, and increasing maternal serum calcium levels (Fox, 2007). Calcifications can easily be seen sonographically, and Grannum and coworkers (1979) created a grading scale from 0 to 3 that reflected increasing calcification with increasing numerical grade. However, such grading criteria have not been found useful to predict neonatal outcome (Hill, 1983; McKenna, 2005; Montan, 1986; Sau, 2004).
 Placental Tumors
Placental Tumors
Gestational Trophoblastic Disease
These pregnancy-related trophoblastic proliferative abnormalities are discussed in Chapter 20 (p. 396).
Chorioangioma
These benign tumors have components similar to blood vessels and stroma of the chorionic villus. Also called chorangioma, these placental tumors have an incidence of approximately 1 percent (Guschmann, 2003). In some cases, maternal serum alpha-fetoprotein (MSAFP) levels may be elevated with these tumors, an important diagnostic finding as discussed in Chapter 14 (p. 285). Their characteristic sonographic appearance has a well-circumscribed, rounded, predominantly hypoechoic lesion near the chorionic surface and protruding into the amnionic cavity. As shown in Figure 6-4, documenting increased blood flow by color Doppler helps to distinguish these lesions from other placental masses such as hematoma, partial hydatidiform mole, teratoma, metastases, and leiomyoma (Prapas, 2000).
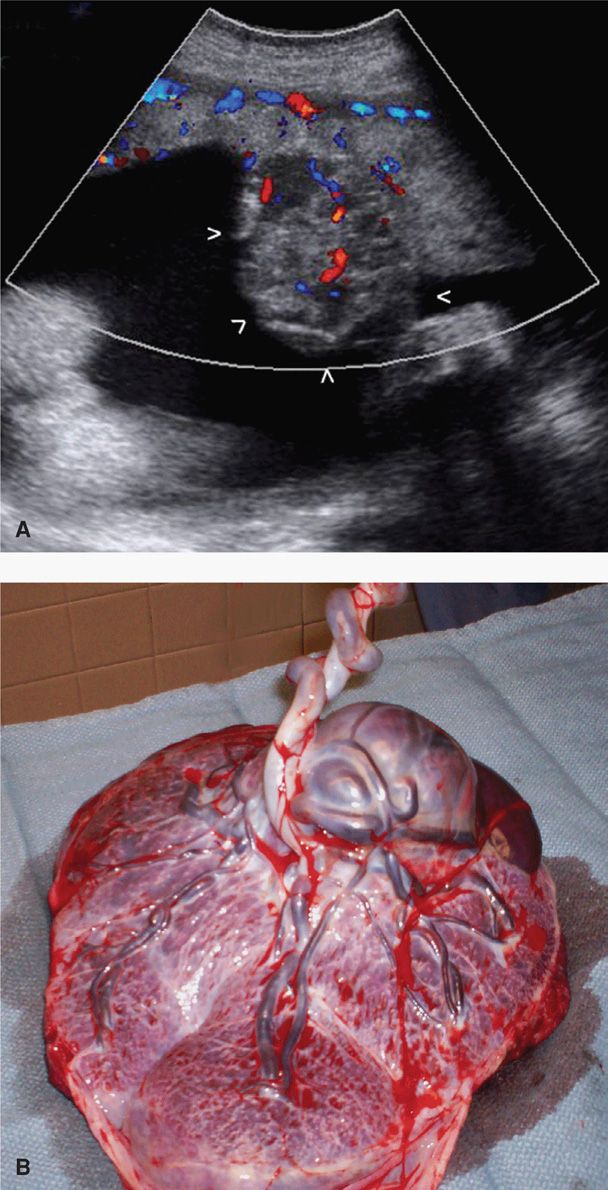
FIGURE 6-4 Placental chorioangioma. A. Color Doppler imaging displays blood flow through a large chorioangioma with its border outlined by white arrows. B. Grossly, the chorioangioma is a round, well-circumcised mass protruding from the fetal surface.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


