The processes leading to ovulation, fertilisation, and implantation of the fertilised ovum are complex and still incompletely understood. Ovulation results from an interplay between the hypothalamus, pituitary, ovary and endometrium. The ovary has two roles: the first is the endocrine function of producing oestrogen and progesterone to prepare the endometrium to receive the fertilised ovum. The second, which is intrinsically related, is gametogenesis and ovulation.
OVULATION
PITUITARY CONTROL OF OVARY
OVULATION AND MENSTRUATION
MENSTRUATION
FERTILISATION
DEVELOPMENT OF THE EMBRYO
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Physiology of Reproduction
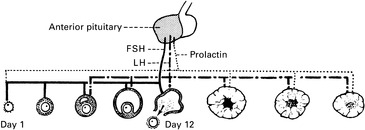
Development of the ovarian follicle occurs in response to stimulation from the pituitary gland.
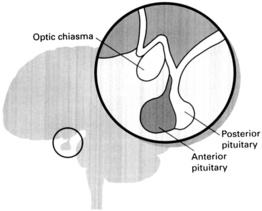
The hypothalamus and pituitary are intimately associated. Together they regulate ovarian structure and function throughout the menstrual cycle.
The hypothalamus produces gonadotrophin releasing hormone (GnRH) in a pulsatile fashion and this in turn stimulates production of the gonadotrophins follicle stimulating hormone (FSH) and luteinising hormone (LH).
The ovarian changes are controlled mainly by the anterior pituitary which produces three principal hormones: follicle stimulating hormone (FSH) stimulates follicular growth. Luteinising hormone (LH) stimulates ovulation and causes luteinisation of granulosa cells after escape of the ovum. Prolactin is also produced by the anterior pituitary.
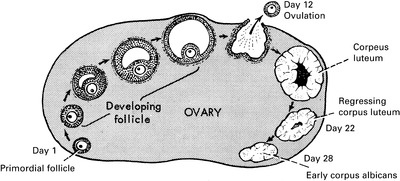
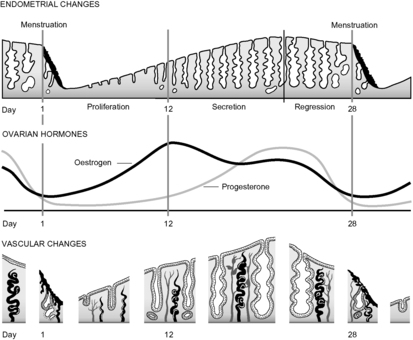
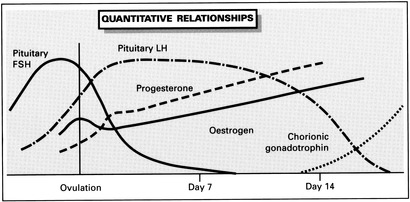
At the end of the menstrual cycle oestrogen levels are low. Low oestrogen levels stimulate production of FSH by the pituitary. FSH in turn acts upon the ovary to stimulate growth of ovarian follicles. The increasing levels of oestrogen produced by the developing follicles act on the pituitary to reduce FSH levels by the process of negative feedback. In the majority of cycles only one follicle, the so-called dominant follicle, is sufficiently large and has a greater density of FSH receptors to respond to the lower FSH levels and develops to the stage of ovulation. Non-identical twinning results when more than one follicle proceeds to ovulation. Oestrogen levels continue to rise. In the mid-cycle the nature of the ovarian control of pituitary function changes. Increasing oestrogen levels are required to produce a positive feedback mechanism which causes a surge in FSH and LH levels. This surge evokes ovulation. LH acts to increase local production of prostaglandins and proteolytic enzymes to allow oocyte extrusion. LH is responsible for the development of the corpus luteum which produces progesterone.
As ovulation approaches, the progesterone receptor content increases. Within two days of ovulation the effect of ovarian production of progesterone becomes apparent as the endometrium enters the Secretory Phase of the cycle. During this phase the mitotic activity in the epithelium ceases and the glands become dilated and tortuous. The blood vessels become more coiled. Glycogen accumulation in the endometrium reaches a peak under the combined influence of oestrogen and progesterone. These processes prepare the endometrium for embedding of the embryo. If fertilisation does not occur then progesterone and oestrogen levels decline and menstruation occurs.
For the first fourteen days after fertilisation uterine growth and the development of the decidua (the endometrium of pregnancy) are dictated by the corpus luteum under the influence of the pituitary. Thereafter the pituitary LH levels are reduced in response to the increasing levels of HCG.
Under the influence of chorionic gonadotrophin the corpus luteum continues to grow and to secrete ovarian steroids for the maintenance of uterine growth. HCG levels reach a peak around 10 to 12 weeks and thereafter decline to a lower constant level throughout pregnancy. The response to this reduction is a decrease in ovarian oestrogen and progestogen output. As the ovarian contribution to maintaining the pregnancy declines, the placenta increases steroid production. Placental steroid production is impressive and analogues of both hypothalamic and pituitary hormones are produced. The capacity to produce these hormones increases as the early placenta develops.