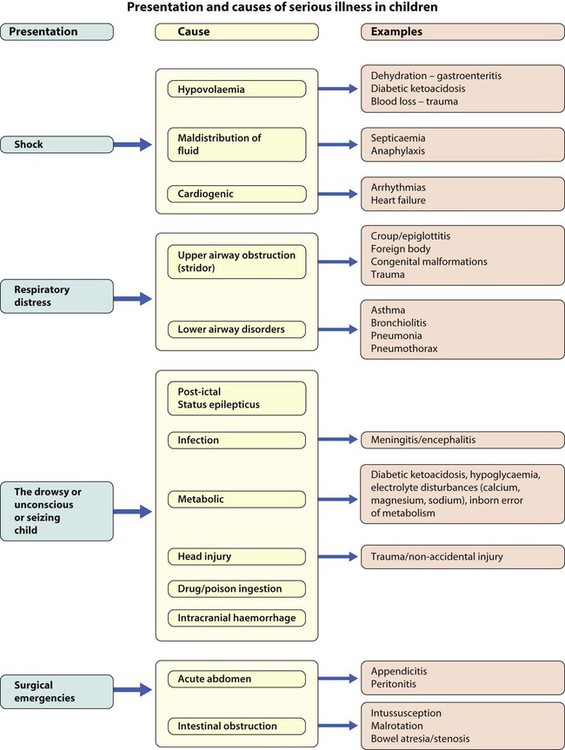
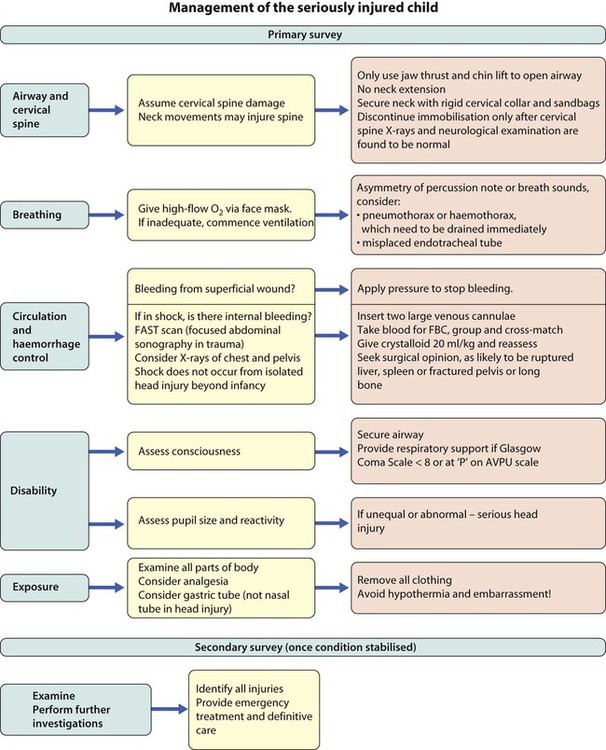
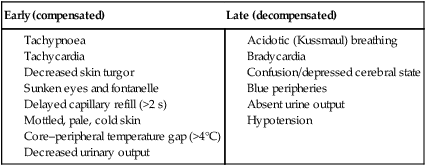
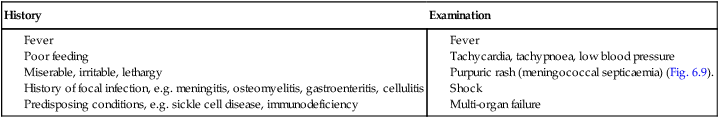
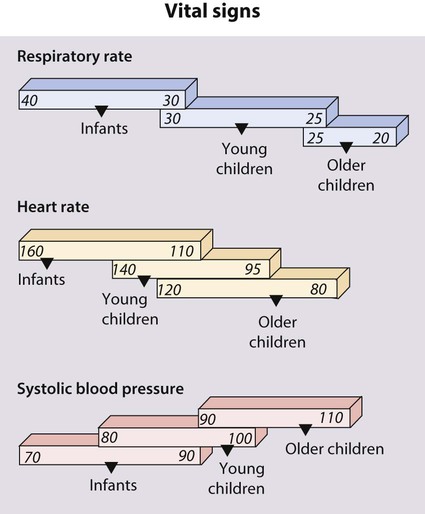
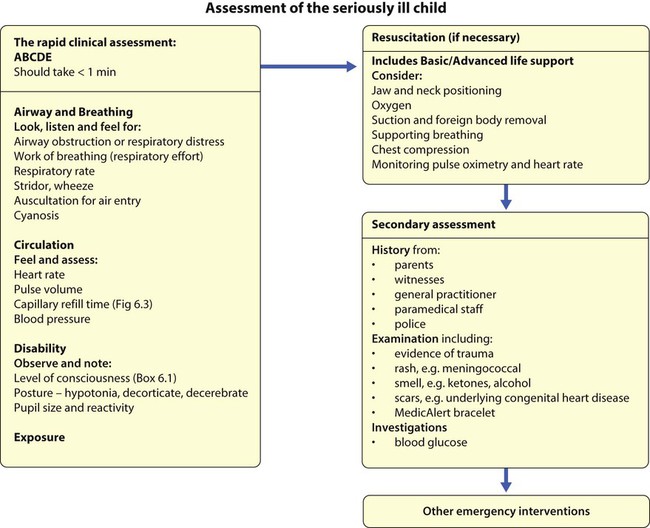
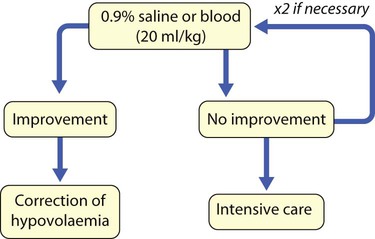
The rapid clinical assessment of the seriously ill child will identify if there is potential respiratory, circulatory or neurological failure. This should take less than 1 minute. Normal vital signs are shown in Figure 6.1 and how a rapid assessment is performed is shown in Figure 6.2. The seriously ill child may present with shock, respiratory distress, as a drowsy/unconscious or fitting child or with a surgical emergency. Their causes are listed in Figure 6.4. In children, the key to successful outcome is the early recognition and active management of conditions that are life-threatening and potentially reversible. Children normally require a much higher fluid intake per kilogram of body weight than adults (Table 6.1). This is because they have a higher surface area to volume ratio and a higher basal metabolic rate. Children may therefore become dehydrated if: Table 6.1 Fluid intake at different ages • they are unable to take oral fluids • there are additional fluid losses due to fever, diarrhoea or increased insensible losses (e.g. due to increased sweating or tachypnoea) • there is loss of the normal fluid-retaining mechanisms, e.g. burns, the permeable skin of premature infants, increased urinary losses or capillary leak. The clinical features of shock are manifestations of compensatory physiological mechanisms to maintain the circulation and the direct effects of poor perfusion of tissues and organs (Box 6.2). In early, compensated shock, the blood pressure is maintained by increased heart and respiratory rate, redistribution of blood from venous reserve volume and diversion of blood flow from non-essential tissues such as the skin in the peripheries, which become cold, to the vital organs like brain and heart. In shock due to dehydration, there is usually >10% loss of body weight (see Ch. 13) and a profound metabolic acidosis which is compounded by failure to feed and drink while severely ill. After acute blood loss or redistribution of blood volume because of infection, low blood pressure is a late feature. It signifies that compensatory responses are failing. Rapid restoration of the intravascular circulating volume is the priority (Fig. 6.8). This will usually be with 0.9% saline, or blood if following trauma.
Paediatric emergencies
The seriously ill child
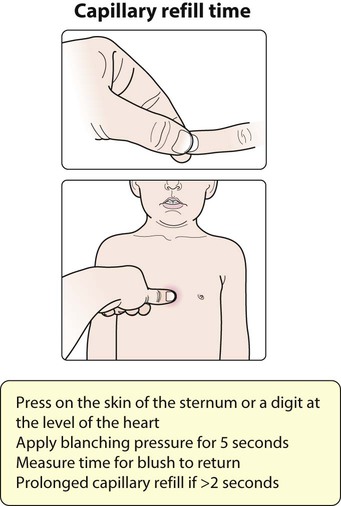
![]() Capillary refill time is affected by body exposure to a cold environment.
Capillary refill time is affected by body exposure to a cold environment.
Shock
Why are children so susceptible to fluid loss?
Body weight
Fluid requirement/24 h
Volume/kg per hour (approximate)
First 10 kg
100 ml/kg
4 ml/kg
Second 10 kg
50 ml/kg
2 ml/kg
Subsequent kg
20 ml/kg
1 ml/kg
Examples of calculations
Infant (7 kg)
700 ml
28 ml/h
Child (18 kg)
1000 + 400 = 1400 ml
40 + 16 = 56 ml/h
Adolescent (42 kg)
1000 + 500 + 440 = 1940 ml
40 + 20 + 22 = 82 ml/h
Clinical features
Management priorities
Fluid resuscitation
Paediatric emergencies