23 Otolaryngology
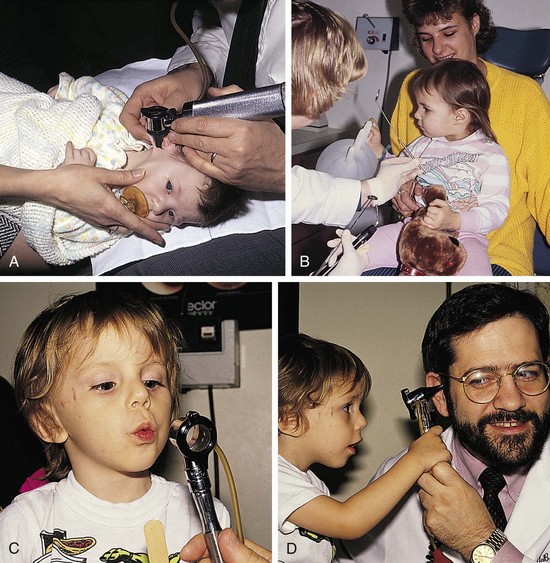
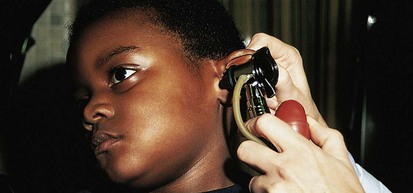
Whenever possible, the child should be allowed to sit on the parent’s lap. Pacifiers, puppets and other toys, and tongue blades with faces drawn on them can all serve to reduce anxiety, enlist the child’s trust, and distract attention. Gradual introduction of the equipment can also be helpful, especially if done in a playful way. The child can be asked to blow out the otoscope light while the examiner turns it off, urged to catch the light spot as the examiner moves it around, and even allowed to look in the parent’s or examiner’s ears (Fig. 23-1, A-D). Parents can also help demonstrate maneuvers for opening the mouth, panting to depress the tongue, and holding the head back. Although this may take a little additional time at the outset, it often saves considerable time in the long run and makes future follow-up examinations far easier.
Ear Disorders
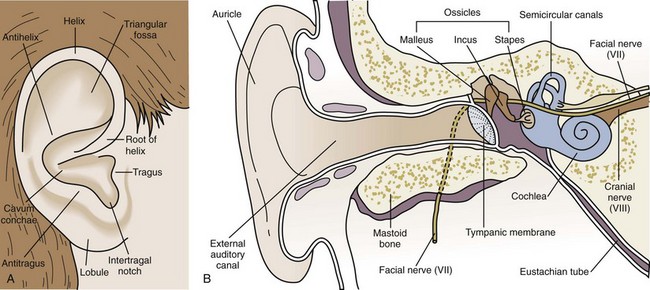
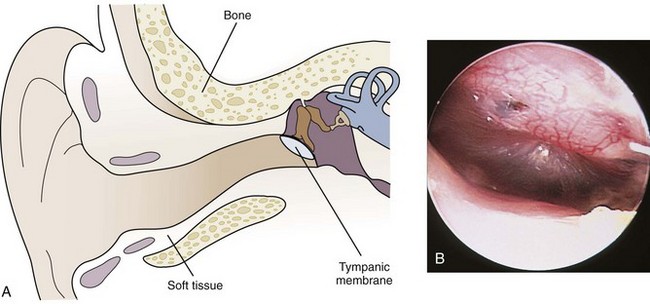
A brief review of the anatomy of the ear is helpful in developing a logical approach to any clinical abnormalities that may be encountered. The ear is conveniently divided into the following three regions (Fig. 23-2):
1 The external ear includes the pinna, or auricle, and the external auditory canal, up to and including the tympanic membrane.
2 The middle ear is made up of the middle ear space, the inner surface of the eardrum, the ossicles, and the mastoid.
3 The inner ear comprises the cochlea (hearing), the labyrinth and semicircular canals (balance), and the main nerve trunks of the seventh and eighth cranial nerves.
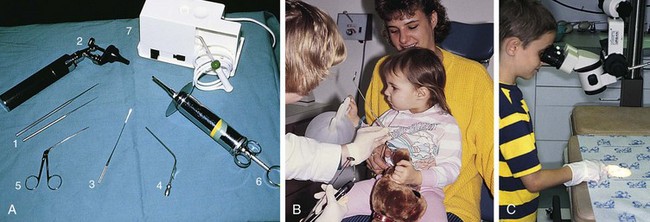
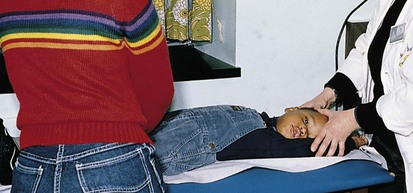
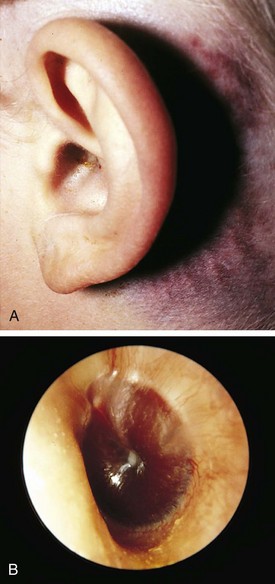
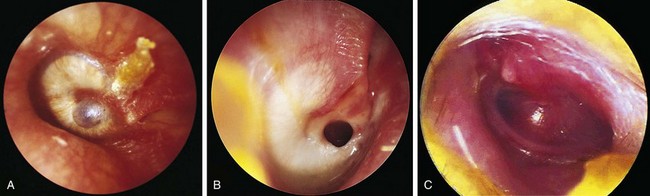
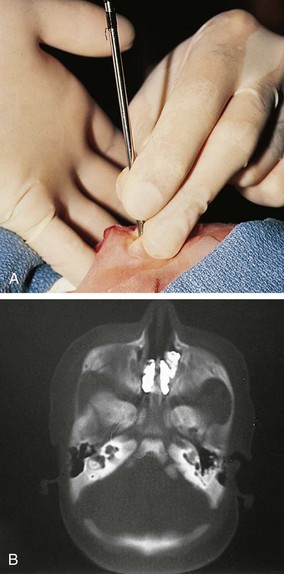
The examination should include inspection of the auricle, periauricular tissues, and external auditory canal and visualization of the entire tympanic membrane, including assessment of its mobility in response to positive and negative pressure with pneumatic otoscopy. This necessitates clearing the canal of cerumen or discharge by using a curette, cotton wick, lavage, or suction, and presumes that the tympanic membrane is intact (Fig. 23-3, A and B). Use of a surgical otoscope head or an examining microscope assists visualization during the cleaning process. These procedures should be performed carefully and gently and attempted only after the child has been carefully immobilized to avoid trauma (Fig. 23-4). It is extraordinarily easy to injure the canal during the process of cleaning the external ear. Hence great care must be taken; otherwise bleeding from the ensuing trauma obscures the examination and upsets the patient and parent. Steadying of the examiner’s hands on the child’s head while using the otoscope and instruments is an essential skill to avoid ear trauma. Both the patient and parent should be given a clear explanation of the procedure beforehand. Allowing older children to handle and look through the equipment before cleaning the ear reduces anxiety and enhances cooperation (see Fig. 23-3, C).
Because the external auditory canal is often angulated in infants and young children, gentle lateral traction on the pinna is frequently necessary to assist visualization of the eardrum itself (Fig. 23-5). In infants the tympanic membrane tends to be oriented at a greater angle (Fig. 23-6, A and B); the landmarks are less prominent; and the skin that lines the canal, being loosely attached, moves readily on insufflation of air, simulating a normally mobile eardrum. To avoid confusion, the canal should be inspected as the speculum is inserted to ensure that the transition between canal wall and tympanic membrane is visualized.
1 Use adequate light. A bright halogen lamp is better than an ordinary light bulb. Replace bulbs routinely every 4 to 6 months, and provide for routine battery charging.
2 Choose a speculum of sufficient diameter and length to allow adequate penetration (10 to 15 mm) into the external canal for good eardrum visualization and a good seal for pneumatic otoscopy.
3 Restrain the patient (on the parent’s lap or on the examining table).
4 Brace the hand holding the otoscope on the child’s head to avoid ear canal trauma.
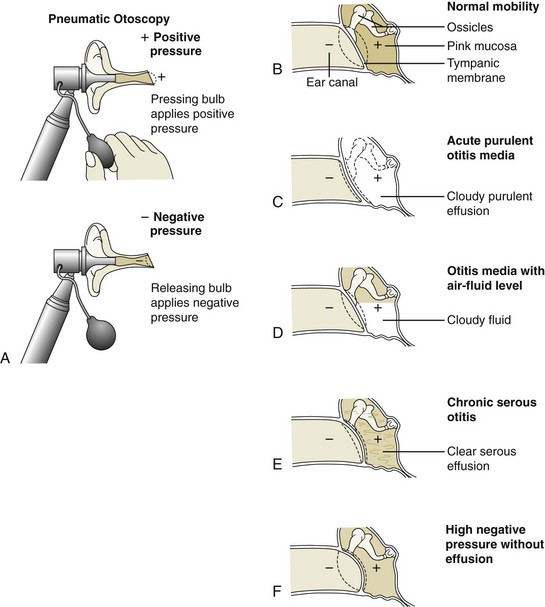
When otoscopic findings are unclear or when it is difficult to obtain a good air seal for pneumatic otoscopy, tympanometry can be highly useful in evaluating patients older than 8 months of age (Fig. 23-7). The procedure is not of value in young infants because the abundance of loose connective tissue lining the ear canal and the laxity of the cartilage at the entrance increase canal wall compliance and invalidate the results.
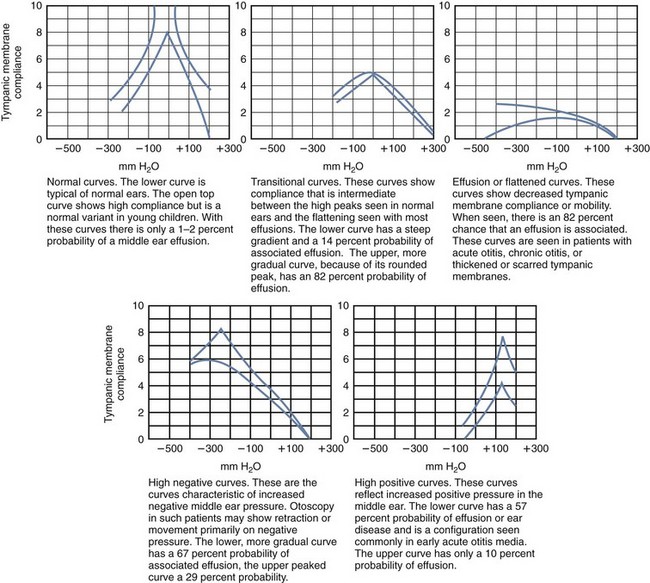
Figure 23-7 Tympanometric patterns of various conditions of the middle ear.
(Courtesy Mrs. Ruth Bachman, Pittsburgh, Pa.)
Because otitis media can be a reflection of both immunologic and anatomic abnormalities, the practitioner should be suspicious of possible underlying immune or temporal bone defects when seeing patients with chronic or frequently recurrent otitis media. The temporal bone is the bony housing for the auditory and vestibular systems. In addition, it provides bony protection for the facial nerve as it crosses from the brainstem to the facial muscles. The growth and development of this bone are affected in syndromes such as Treacher Collins that are characterized by altered midface growth (Fig. 23-8). The soft tissues attached to the temporal bone, such as the muscles controlling eustachian tube function, can be abnormal in children with cleft palates (see Palatal Disorders, later). As a result, children with these disorders tend to have an increased incidence of otitis media.
Disorders Of The External Ear
The “Four D’s”
Discharge
Discharge is a common complaint with a number of possible causes. When there is thick, white discharge and erythema of the canal wall, the physician should gently pull on the pinna. If this maneuver elicits pain and the canal wall is edematous, primary otitis externa is the likely diagnosis (Fig. 23-9), although prolonged drainage from untreated otitis media with perforation may present a similar picture (see Disorders of the Middle Ear, later). When the middle ear is the source of otic discharge, the tympanic membrane is abnormal and should show evidence of perforation (see Fig. 23-26). The major predisposing condition to primary otitis externa is prolonged excessive moisture in the ear canal, which promotes bacterial or fungal overgrowth. Thus this is a common problem in swimmers. Another major source is the presence of a foreign body in the ear canal (see Fig. 23-19), which stimulates an intense inflammatory response and production of a foul-smelling purulent discharge. Thus when otic drainage is encountered, the discharge must be gently removed under appropriate magnification to assess the condition of the tympanic membrane and to rule out the presence of perforation and foreign objects. This can be accomplished either by gentle siphoning and wiping with cotton wicks or by careful suctioning (see Fig. 23-3).
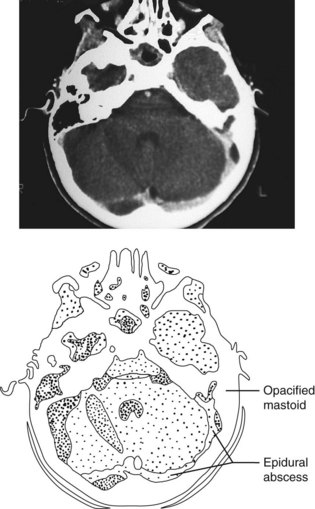
Displacement
Displacement of the pinna away from the skull is a worrisome sign. The most severe condition causing displacement is mastoiditis, resulting from extension of a middle ear infection through the mastoid air cells and out to the periosteum of the skull. In addition to displacement, important clinical signs of mastoiditis include erythema and edema and possibly fluctuance of the skin overlying the mastoid, exquisite tenderness on palpation of the mastoid process, a sagging ear canal, purulent otorrhea, fever, and usually toxicity (Fig. 23-10). This condition is now considered unusual and is seen mainly in patients with long-standing, untreated, or inadequately treated otitis media. Recognition, prompt institution of parenteral antibiotic therapy, and myringotomy with culture and sensitivity testing are crucial because there is significant risk of central nervous system (CNS) extension. The use of a CT scan will delineate the extent of involvement and assist the surgical approach (Fig. 23-11). Mastoidectomy is indicated in cases complicated by bone erosion, or CNS extension, and in those in whom intravenous (IV) antibiotics and myringotomy fail to produce complete resolution.
Other conditions characterized by displacement of the pinna away from the head include parotitis, primary cellulitis of the periauricular tissues, and edema secondary to insect bites or contact dermatitis. Parotitis is differentiated by finding prominent induration and enlargement of the parotid gland anterior and inferior to the external ear, together with blunting of the angle of the mandible on palpation (see Chapter 12). Primary cellulitis is characterized by erythema and tenderness but can often be distinguished clinically from mastoiditis by the presence of associated skin lesions that antecede the inflammation (Fig. 23-12). In cases secondary to untreated external otitis or otitis media with perforation, the picture may be clinically similar. Localized contact dermatitis and angioedema may be erythematous, but they are also pruritic and nontender. The former condition is characterized by microvesicular skin changes (Fig. 23-13), whereas in the latter condition, a precipitating insect bite can often be identified on inspection (Fig. 23-14).
Discoloration
Discoloration is another important sign and is commonly a feature of conditions producing displacement. Erythema of the pinna is common when there is inflammation, with or without infection (see Fig. 23-10, B and Figs. 23-12 to 23-14). Ecchymotic discoloration may be encountered with trauma. When this overlies the mastoid tip, the area immediately posterior to the pinna, it is termed a Battle sign (Fig. 23-15, A) and usually reflects a basilar skull fracture. In such cases the canal wall should be checked for tears and the tympanic membrane for perforation or a hemotympanum (blood behind the tympanic membrane; Fig. 23-15, B). These findings are generally more helpful in making the diagnosis than routine skull x-rays, which are often inconclusive. CT can usually confirm the diagnosis of a basilar skull fracture. Recognition that bruising of the pinna and/or postauricular area can be a manifestation of child abuse is most important (see Chapter 6).
Deformity
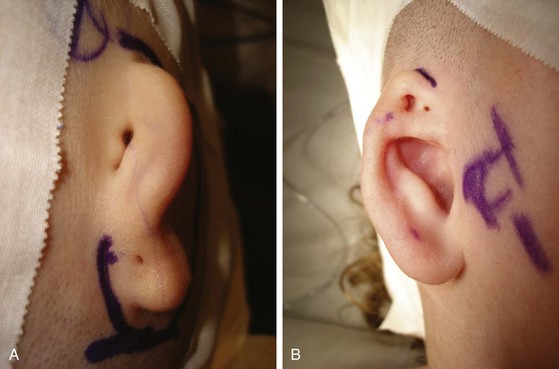
When the external ear is grossly misshapen or microtic, associated anomalies of middle ear structures are common and hearing loss may be significant (Fig. 23-16, A and B). Severe deformities stem from developmental anomalies of the branchial arches, which contribute to both external ear and middle ear structures. Such abnormalities warrant a thorough evaluation in infancy to ensure early recognition and treatment of hearing loss. Deformity of the pinna can be the result of hereditary factors or exposure to teratogens, but at times it is simply produced by unusual intrauterine positioning. Most deformities are minor and represent isolated malformations of mostly cosmetic significance (Fig. 23-17, D). In some instances they may be part of a picture of multiple congenital anomalies (Fig. 23-17, A-C; see also Fig. 23-8 and Chapter 1).
Preauricular sinuses and cysts constitute two of the more common congenital abnormalities. These are congenital remnants located anterior to the pinna with an overlying surface dimple (Fig. 23-18, A). These cysts are vulnerable to infection and abscess formation (Fig. 23-18, B), which necessitate needle aspiration or incision and drainage in conjunction with antistaphylococcal antibiotics. Once infection has occurred, recurrence is common unless the entire sinus is completely excised. This procedure should be undertaken once inflammation has subsided. A preauricular sinus may also result from branchio-oto-renal syndrome (also known as Melnick-Fraser syndrome), an autosomal dominant disorder characterized by bilateral preauricular sinuses, ear anomalies, branchial cleft anomalies in the neck, and renal problems.
Foreign Objects and Secondary Trauma
It is not unusual for children to put paper, beads, and other foreign objects into their ear canals (Fig. 23-19, A). Small insects also on occasion may become trapped in the external ear (Fig. 23-19, B). In some cases small objects may be embedded in cerumen and missed on inspection. As noted earlier, if present for more than a few days, the foreign material stimulates an inflammatory response and production of a purulent discharge that is often foul-smelling and may obscure the presence of the inciting foreign body. Removal of some objects can be accomplished by use of otologic alligator forceps or by irrigation of the ear canal; others—particularly spherical objects—require use of a Day (right angle) hook or suction (Fig. 23-19, C; see also Fig. 23-3). Foreign objects may also be the cause of painful abrasions or lacerations of the external auditory canal or even perforation of the tympanic membrane. Insertion of pencils or sticks into the ear canal by the child and parental attempts to clean the canal with a cotton swab are the most common modes of such injury.

Figure 23-19 Otic foreign bodies. A, This child inserted a bead into her ear. The object must be removed carefully to prevent further trauma. B, This patient experienced a period of intense buzzing, pain, and itching in the ear that abated after a few hours. If the tympanic membrane is intact, olive or mineral oil may be used to drown the insect. C, A blunt-tipped, right-angled Day hook, small wire loop curette, Hartmann forceps, and an alligator forceps (and see Fig. 23-3, A) are useful instruments for removing foreign bodies from the external auditory canal.
Exposure to concussive forces such as a direct blow (which may be accidental or inflicted) or an explosion can also result in perforation (Fig. 23-20, A and B). Patients with traumatic perforations must be carefully assessed for signs of injury to deeper structures. If tympanic membrane perforation occurs as a result of penetration by a foreign object or of concussive forces, the physician must be particularly aware of the possibility of middle ear or inner ear damage. Evidence of hearing loss, vertigo, nystagmus, facial nerve injury, or cerebrospinal fluid leak should prompt urgent otolaryngologic consultation because an emergency surgical exploration may be indicated.
Disorders Of The Middle Ear
The normal tympanic membrane is thin, translucent, neutrally positioned, and mobile. The ossicles, particularly the malleus, are generally visible through the membrane (Fig. 23-21). Adequate assessment of the tympanic membrane requires that the examiner note four major characteristics: (1) thickness, (2) degree of translucence, (3) position relative to neutral, and (4) mobility. Application of gentle positive and negative pressure, using a properly sealed pneumatic otoscope (Fig. 23-22), produces brisk movement of the eardrum when the ear is free of disease and abnormal movement when fluid is present, when the drum is thickened or scarred, or when there is an increase in either positive or negative pressure (Fig. 23-23). An abnormality in any one of the four major characteristics suggests middle ear pathology.
Acute Otitis Media
Acute otitis media is the term used to describe acute infection and inflammation of the middle ear. Associated inflammation and edema of the eustachian tube mucosa appear to play key roles in the pathogenesis by impeding drainage of the middle ear fluid. In some children, anatomic or chronic physiologic abnormalities of the eustachian tube predispose to infection. The problem is commonly seen in conjunction with an acute upper respiratory tract infection, and its onset is often heralded by a secondary temperature spike one to several days after the onset of respiratory symptoms. The major offending organisms are bacterial respiratory pathogens. The most commonly isolated organisms and their relative frequency, shown in Table 23-1, demonstrate the rise of penicillin-resistant Streptococcus pneumoniae. A small proportion of cases constitute an exception to these percentages, that is, those in which otitis is accompanied by conjunctivitis. Nontypable Haemophilus influenzae is found to be causative in 70% to 75% of these cases. Increasing rates of β-lactamase positivity in these organisms, as well as the rising incidence of penicillin-resistant S. pneumoniae, has necessitated the use of high-dose amoxicillin and/or greater use of β-lactamase–resistant antibiotic regimens whenever this scenario is seen. Sulfa drugs may also be useful for therapy of community-acquired methicillin-resistant Staphylococcus aureus, which is becoming increasingly common.
Table 23-1 Acute Otitis Media: Most Commonly Isolated Bacterial Pathogens and Their Relative Frequency
| Bacterial Pathogen | Number of Isolates (% of Total) | Number Resistant (%) |
|---|---|---|
| Streptococcus pneumoniae | 49 (44) | 18 (37) |
| Haemophilus influenzae | 46 (41) | 21 (46) |
| Moraxella catarrhalis | 16 (14) | 16 (100) |
| Staphylococcus aureus | 0 (0) | 0 (0) |
| Total | 111 (100) | 55 (50) |
In acute otitis media the classic findings on inspection of the tympanic membrane are erythema and injection; bulging that obscures the malleus; thickening, often with a grayish-white or yellow hue, reflecting a purulent effusion; and reduced mobility (Fig. 23-24, A). However, crying produces erythema of the eardrum, and thus tympanic erythema in a crying child is of little diagnostic value. The patient is usually febrile and, if old enough, typically complains of otalgia. However, in many cases this “textbook picture” is not seen. This is probably due in part to time of presentation, the virulence of the particular pathogen, and host factors.
Accuracy in diagnosis necessitates meticulous inspection during otoscopy and knowledge of the various modes of presentation. Children may have fever of a few hours’ duration and otalgia (or if very young, fever and irritability) yet have no abnormality on otoscopy. If re-examined the next day, many of these patients have clear evidence of acute otitis media. Some have erythema and bubbles or air–fluid or air–pus levels (a result of venting by the eustachian tube) without bulging and with nearly normal mobility of the eardrum (Fig. 23-24, B). In still other cases the drum may be full and poorly mobile with cloudy fluid behind it but with minimal erythema (Fig. 23-24, C). In some patients the drum is retracted, moves primarily or only in response to negative pressure, and shows signs of inflammation and/or a cloudy effusion.
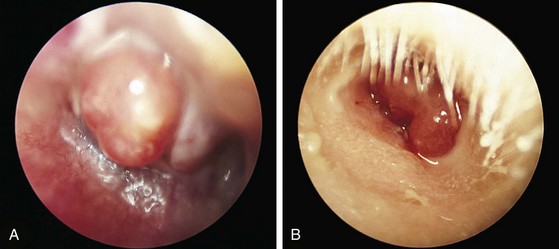
On occasion the signs and symptoms of otitis media may be accompanied by formation of a bullous lesion on the surface of the tympanic membrane, a condition termed bullous myringitis (Fig. 23-25). These children usually complain of intense pain. Whereas this phenomenon is most commonly associated with Mycoplasma infection in adults, any of the usual pediatric pathogens (see Table 23-1) can be causative in children. Finally, acute otitis media may, by virtue of increasing middle ear pressure, result in acute perforation of the tympanic membrane. On presentation the canal may be filled with purulent material; however, tugging on the pinna usually does not elicit pain, and erythema and edema of the canal wall are minimal or absent. Cleansing with a cotton wick or suction usually reveals an inflamed drum with a barely visible perforation (Fig. 23-26).
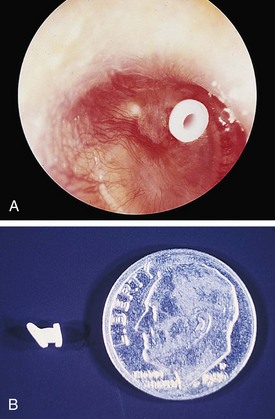
Otitis Media with Effusion (Serous Otitis Media)
Serous effusion in the middle ear may result from an upper respiratory tract infection, or it may be the residual of treated acute otitis. In many instances this effusion is not spontaneously cleared but instead remains in the middle ear for weeks or months, resulting in a persistent clear gray or yellow effusion behind the eardrum (Fig. 23-27). Persistence appears to result in part from eustachian tube dysfunction with poor drainage and ventilation. Pneumatic otoscopy often reveals poor mobility of the tympanic membrane, and mobility is noted primarily on negative pressure. The latter is thought to develop as a result of absorption of middle ear gases by mucosal cells, creating a vacuum that persists with the fluid because of failure of ventilation by the eustachian tube. Such long-standing effusions impair hearing. Persistence of bilateral serous effusions for more than 3 to 4 months with hearing loss is an indication for myringotomy and insertion of tubes (see Fig. 23-29, A and B) to improve hearing.
Chronic–Recurrent Otitis Media
Chronic or chronic–recurrent otitis media with effusion (COME) is common in young children. Patients subject to this condition appear to have significant and prolonged eustachian tube dysfunction. This “otitis-prone” state may be a seemingly isolated phenomenon, or it can be a feature of a number of syndromes characterized by palatal dysfunction or malformation or by facial hypoplasia or deformity. These conditions include cleft palate, Crouzon syndrome, Down syndrome, and the mucopolysaccharidoses and mucolipidoses (see Fig. 23-8; and see Palatal Disorders, later). Chronic obstructive adenoidal hypertrophy may also be a predisposing condition. Less commonly, immunodeficiency and immotile cilia syndrome are identified as underlying etiologic conditions.
Chronic otitis media is associated with significant morbidity in terms of intermittent or chronic hearing impairment, intermittent discomfort, and the sequelae of recurrent infection. Over months or years, the process produces permanent myringosclerotic changes in which the tympanic membrane becomes whitened, thickened, and scarred (Fig. 23-28, A). Chronic perforations are common (Fig. 23-28, B). Patients with persistent middle ear infections despite medical therapy, those with frequent recurrences, and children with chronic severe tympanic membrane retraction (Fig. 23-28, C) appear to benefit from surgical drainage and insertion of tympanostomy tubes that vent the middle ear (Fig. 23-29). Persistence of a serous effusion for longer than 3 to 4 months with significant hearing loss is also an indication for myringotomy and insertion of tubes. Once placed, tubes should be checked at intervals for presence and patency. Spontaneous extrusion generally occurs 6 to 24 months after insertion. When tubes have been inserted, it is wise to prevent contamination of the middle ear with water. The need for earplugs in children with tubes or a perforation is the subject of some controversy, but in general their use is still recommended.
Other Middle Ear Disorders
Mass Lesions Involving the Tympanic Membrane
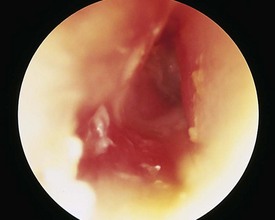
The most common and one of the most serious mass lesions of the eardrum is a cholesteatoma. It can present as a defect in the tympanic membrane through which persistent drainage occurs, or it can appear as a white cystic mass behind or involving the eardrum. It consists of trapped epithelial tissue that grows beneath the surface of the membrane (Fig. 23-30). Although a few are congenital with an intact tympanic membrane, the majority are sequelae of untreated or chronic–recurrent otitis media with a tympanic membrane defect. If a cholesteatoma is not removed surgically, it continues to enlarge; becomes locally destructive; and can erode the mastoid bone, destroy the ossicles, and even invade the inner ear structures or cranium. Progressive hearing impairment is usually a feature of this condition. Congenital cholesteatoma is rare. It is seen under an intact tympanic membrane in the anterior superior quadrant of the middle ear.
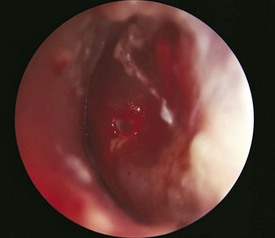
Granulomas or polyps of the tympanic membrane (Fig. 23-31) can also develop in children with chronic middle ear infections. The most common cause of aural polyps in children is an old, retained tympanostomy tube. Cholesteatoma is another predisposing condition. These tissues often bleed easily, which can frighten the patient, the parent, and the physician. Left untreated, polyps can enlarge to fill the canal and by expansion can progressively damage the drum and the ossicles. Therefore prompt surgical removal is indicated if therapy with topical and oral antimicrobials is unsuccessful.
Distortions of the Tympanic Membrane
Thin, dimeric portions of the eardrum may be observed in patients with chronic middle ear disease, or they may develop after extrusion of a tympanostomy tube (Fig. 23-32; see also Fig. 23-28, A). These thinned areas are the result of abnormal healing of perforations and are hypermobile on pneumatic otoscopy. The important points to note on examination are whether the full depth of the pocket is visible or partly hidden, its location with respect to the ossicles, and whether or not it is dry. If the ear canal and drum are not dry, an active infection and/or cholesteatoma is present. In cases of severe deformity, aggressive therapy including ventilation of the middle ear and surgical excision of the pocket may be necessary.
Nasal Disorders
Nasal Examination
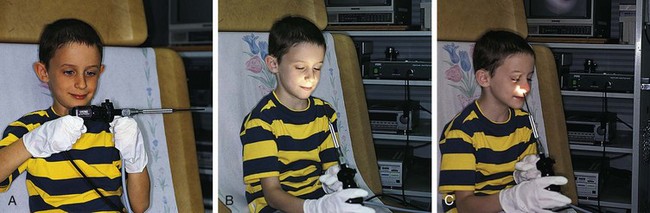
A more thorough examination is possible with a nasal endoscope; this enables full visualization of internal nasal structures. Before starting, the nose is sprayed with a decongestant to shrink the nasal mucosa and with a topical anesthetic. With patience, older children can be coaxed through the insertion and examination. Allowing them to hold and inspect the device, test the light, look at themselves on the monitor, and even insert the tip into their nose assists cooperation (Fig. 23-33, A-C). Most children younger than 5 years of age require immobilization, either on a papoose board or with parental and nursing assistance. The nasal endoscope is a useful tool, and this type of examination can be done readily in the otolaryngologist’s office.
Nasal Congestion and Obstruction
Nasopharyngitis Secondary to Gastroesophageal Reflux (Reflux Rhinitis)
Infants with gastroesophageal reflux disease (GERD) may develop persistent nasal congestion and rhinorrhea with varying degrees of mucosal inflammation and edema in response to exposure to gastric contents. Snoring and/or coughing during sleep are common associated symptoms. Although vomiting or frequent spitting, sometimes with passage of regurgitated material through the nose, may be reported, often such symptoms are absent. The section Otolaryngologic Manifestations of Gastroesophageal Reflux Disease near the end of this chapter details the spectrum of signs and symptoms that may assist in diagnosis of GERD-related nasal disorders.
Congenital Causes of Nasal Obstruction
Choanal Atresia and Stenosis
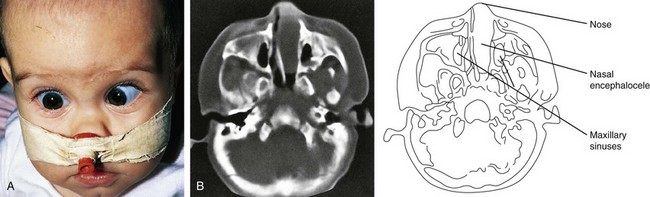
Choanal atresia may be bony (90%) or membranous (10%), bilateral or unilateral. Newborns with bilateral choanal atresia manifest severe respiratory distress at delivery, with cyanosis that is relieved by crying and returns with rest (paradoxic cyanosis). The true nature of the problem can elude detection if the physician relies solely on passing soft feeding catheters through the nose to determine patency, because these can buckle or curl within the nose. The correct diagnosis is best made with a van Buren urethral sound or a firm plastic suction catheter (both no. 8 French). This is passed gently along the floor of the nose, close to the septum. If bony resistance is encountered, the diagnosis of choanal atresia is suspected (Fig. 23-34, A) and can be confirmed by endoscopy or by obtaining a CT scan of the nose and nasopharynx with fine overlapping cuts (Fig. 23-34, B).
Immediate relief of neonatal respiratory distress from bilateral choanal atresia may be accomplished by insertion of an oral airway (or a firm nipple from which the tip has been cut away) into the mouth. Definitive studies can then be performed to aid in planning surgical correction. Infants with unilateral choanal atresia (Fig. 23-35) are usually asymptomatic at birth; however, with time they develop a persistent unilateral nasal discharge.
Congenital Mass Lesions
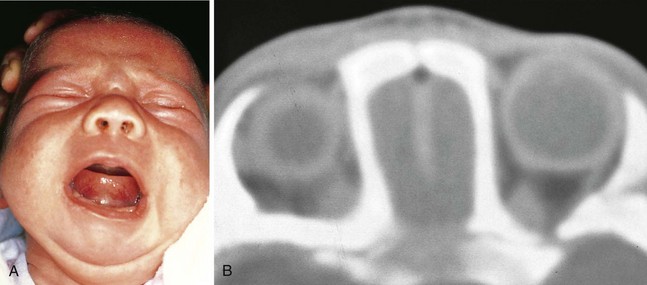
An encephalocele is an outpouching of brain tissue through a congenital bony defect in the midline of the skull. Some patients have craniofacial deformities and a rounded subcutaneous swelling between the eyes or adjacent to the nose. In other instances the neural tissue prolapses into the nasal cavity or nasopharynx, resulting in signs and symptoms of nasal obstruction without obvious external anomalies (Fig. 23-36, A). On occasion, a grapelike mass may be seen within the nares or protruding into the back of the mouth. The mass is usually identified by diagnostic radiography. CT (Fig. 23-36, B) is particularly helpful in delineating the extent of the mass and the underlying bony defect. Repair requires a collaborative effort by specialists in otolaryngology, neurosurgery, and in some cases plastic surgery.
Nasal dermoids are embryonic cysts containing ectodermal and mesodermal tissue. They present as round, firm subcutaneous masses located on the dorsum of the nose, close to the midline (Fig. 23-37, A). Examination of the overlying skin frequently reveals a small dimple, at times with extruding hair. Some of these cysts have deep extensions down to the nasal septum or through the cribriform plate into the cranium. Thorough evaluation by axial and coronal CT scans (Fig. 23-37, B) and MRI is necessary to determine extent and to plan repair. If such cysts are not removed, secondary infection is common and often results in fistula formation.
Papillomas (Fig. 23-38) are similar growths that occur on the distal nasal mucosa near the mucocutaneous junction. These growths should be excised to improve appearance and confirm diagnosis; they do not cause obstruction.
Acquired Forms of Nasal Obstruction
Adenoidal and Tonsillar Hypertrophy
The lymphoid tissue that constitutes the tonsils and adenoids is relatively small in infancy, gradually enlarges until 8 to 10 years of age, and then usually begins to shrink in size. In most instances this normal process of hypertrophy results in mild to moderate enlargement of these structures and does not constitute a problem. A small percentage of children, however, develop marked adenoidal and tonsillar hypertrophy, with attendant symptoms of nasal obstruction and rhinorrhea. A few even have difficulty swallowing solid foods. Recurrent infection appears to be the most common inciting factor, although atopy may play a role in some cases. On occasion, mononucleosis is the initiating event, resulting in rapid enlargement of adenoidal and tonsillar tissues that is then slow to resolve (see Tonsillitis/Pharyngitis, later; and see Chapter 12). In most children, progressive adenoidal enlargement appears to be the cumulative result of a series of upper respiratory tract infections. The consequent obstruction to normal flow of secretions then starts a vicious circle, making the child more vulnerable to recurrent infections of the ears, sinuses, and nasopharynx, which in turn further exacerbate the adenoidal and tonsillar hypertrophy.
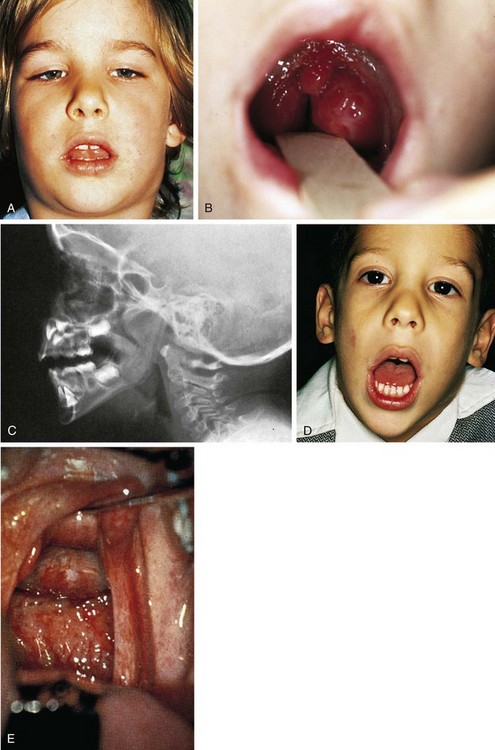
Regardless of the mode of origin, when adenoidal hypertrophy is marked, blockage of the nasal airway becomes severe and results in mouth breathing, chronic rhinorrhea, inability to blow the nose, and snoring during sleep (Fig. 23-39, A). Speech becomes hyponasal and muffled. The child holds his or her mouth open and has little or no airflow through the nares, and his or her tonsils may also meet at the midline (Fig. 23-39, B). A lateral neck x-ray examination reveals a large adenoidal shadow impinging on the nasal airway (Fig. 23-39, C). For many patients these features are noted primarily in the course of acute illness; however, a number of children have symptoms even when free of acute infection. When obstruction is severe, sleep disturbance may result. This is characterized by restlessness and retractions when recumbent, snoring, and frequent waking. Some patients begin to sleep sitting up, and many manifest daytime fatigue, irritability, and short attention span. Symptoms are worse during sleep because relaxation of the pharyngeal muscles further increases the degree of upper airway obstruction. In severe cases this results in periods of hypoxia and hypercarbia. Because a patient may look relatively healthy when awake (with the exception of having to breathe through the mouth), it is important to observe for retractions and to assess the pattern of breathing after the child has been recumbent for a period of time or, better still, during a nap. Use of polysomnography or continuous pulse oximetry may help confirm or establish the diagnosis and determine the severity of sleep apnea. Polysomnography may be useful to assess the severity of the sleep-disordered breathing. If severe obstruction persists for a prolonged period of time, cor pulmonale (with signs of right ventricular hypertrophy on electrocardiogram and chest radiograph) and abnormal facial growth may result (Fig. 23-39, D).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree