88 Osteomyelitis and Other Bone and Joint Infections
Osteomyelitis
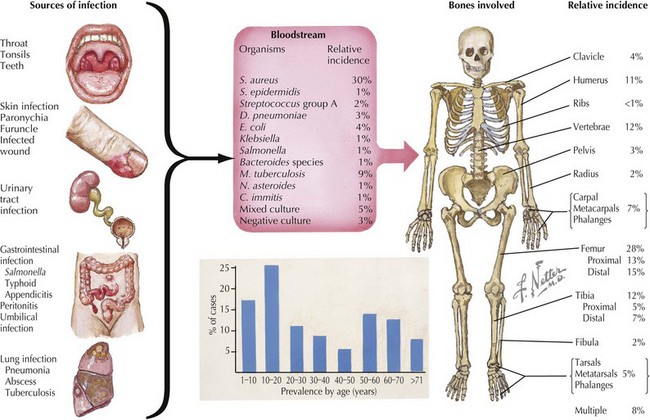
Osteomyelitis is inflammation of bone caused by bacterial or, less often, fungal infection. Osteomyelitis is categorized both by the mechanism of pathogen transmission to the bone (hematogenous, direct extension) and by the clinical presentation (acute, subacute, or chronic). In children, hematogenous spread of bacteria to the bone is the most common mode of transmission (Figure 88-1). Less often, osteomyelitis is the result of contiguous spread from a soft tissue infection or direct inoculation by penetration, such as after trauma or surgery. Vascular insufficiency is a rare cause of osteomyelitis in children. Eighty-five percent of cases of osteomyelitis occur in children younger than 16 years of age (50% in children younger than 5 years of age), with a male-to-female ratio of 2 : 1, except within the first year of life, when both genders are affected equally. Long bones (femur, tibia, humerus, in that order of frequency) followed by bones of the hands and feet and pelvis are the most common sites involved (see Figure 88-1). Approximately 5% of patients have multiple foci.
Etiology
Isolation of a bacterial source of osteomyelitis occurs in 50% to 80% of patients when both blood and bone are cultured. The bacteria responsible for osteomyelitis in children vary by age and underlying condition (see Figure 88-1). Staphylococcus aureus is the most common pathogen in any age group (70%-90% of cases), with community-acquired methicillin-resistant S. aureus (CA-MRSA) becoming more prevalent in recent years. In infants younger than 2 months of age, group B streptococci and gram-negative enteric bacteria are seen in addition to S. aureus. In children younger than 5 years of age, S. aureus, Streptococcus pyogenes, Streptococcus pneumoniae, and Kingella kingae are leading causes of osteomyelitis. Children older than 5 years of age are most commonly infected by S. aureus or S. pyogenes. Neisseria gonorrhoeae may be the etiologic agent in sexually active adolescents.
Pathogenesis
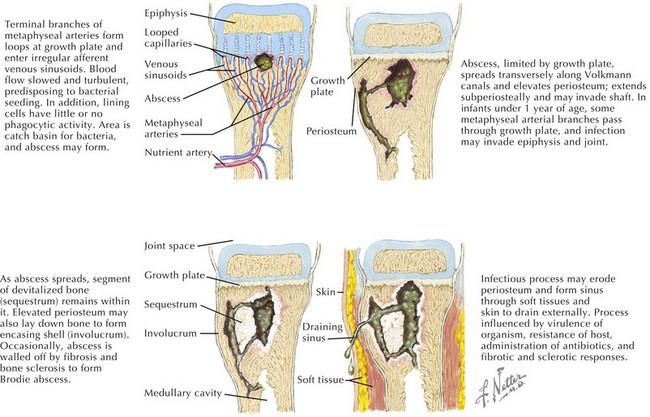
The pathogenesis of acute hematogenous osteomyelitis is dictated by the anatomy of growing bone in young children. The rich vascular supply of the metaphysis and its sluggish flow allow deposition of bacteria that enter via the nutrient artery (Figure 88-2). An absence of macrophages in the metaphyseal capillary loops allows bacterial replication, inducing an inflammatory response that may lead to abscess formation, infarction of bone, and necrosis. Acute hematogenous osteomyelitis is preceded by minor trauma to the site of infection in one-third of cases; resultant small hematomas may make the underlying metaphysis more favorable for bacterial deposition.
Diagnosis
Plain radiographs show soft tissue swelling within 3 days of symptom onset; osteolytic lesions and periosteal elevation are apparent after 10 to 20 days; and after 1 month of symptoms, sclerosis of bone can be seen. Technetium-99 bone scanning has a sensitivity of 80% to 100% for osteomyelitis and can be helpful early on when plain films are normal and can identify multiple sites of infection, when present. Because the radionuclide bone scan can be falsely negative in 5% to 20% of children in the first few days of illness, magnetic resonance imaging (MRI) may be performed. MRI has a sensitivity of 92% to 100% for osteomyelitis and is effective in distinguishing soft tissue infection (e.g., cellulitis) from osteomyelitis. Pelvic and vertebral osteomyelitis are best imaged by MRI. Additionally, chronic osteomyelitis may have a different appearance from acute osteomyelitis on MRI (Figure 88-3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree